Related Research Articles

Bacterial vaginosis (BV) is an infection of the vagina caused by excessive growth of bacteria. Common symptoms include increased vaginal discharge that often smells like fish. The discharge is usually white or gray in color. Burning with urination may occur. Itching is uncommon. Occasionally, there may be no symptoms. Having BV approximately doubles the risk of infection by a number of sexually transmitted infections, including HIV/AIDS. It also increases the risk of early delivery among pregnant women.

Candidiasis is a fungal infection due to any species of the genus Candida. When it affects the mouth, in some countries it is commonly called thrush. Signs and symptoms include white patches on the tongue or other areas of the mouth and throat. Other symptoms may include soreness and problems swallowing. When it affects the vagina, it may be referred to as a yeast infection or thrush. Signs and symptoms include genital itching, burning, and sometimes a white "cottage cheese-like" discharge from the vagina. Yeast infections of the penis are less common and typically present with an itchy rash. Very rarely, yeast infections may become invasive, spreading to other parts of the body. This may result in fevers, among other symptoms.

Trichomoniasis (trich) is an infectious disease caused by the parasite Trichomonas vaginalis. About 70% of affected people do not have symptoms when infected. When symptoms occur, they typically begin 5 to 28 days after exposure. Symptoms can include itching in the genital area, a bad smelling thin vaginal discharge, burning with urination, and pain with sex. Having trichomoniasis increases the risk of getting HIV/AIDS. It may also cause complications during pregnancy.
Gardnerella vaginalis is a species of Gram-variable-staining facultative anaerobic bacteria. The organisms are small non-spore-forming, nonmotile coccobacilli.

The female reproductive system is made up of the internal and external sex organs that function in the reproduction of new offspring. The human female reproductive system is immature at birth and develops to maturity at puberty to be able to produce gametes, and to carry a fetus to full term. The internal sex organs are the vagina, uterus, fallopian tubes, and ovaries. The female reproductive tract includes the vagina, uterus, and fallopian tubes and is prone to infections. The vagina allows for sexual intercourse and childbirth, and is connected to the uterus at the cervix. The uterus or womb accommodates the embryo, which develops into the fetus. The uterus also produces secretions, which help the transit of sperm to the fallopian tubes, where sperm fertilize ova produced by the ovaries. The external sex organs are also known as the genitals and these are the organs of the vulva including the labia, clitoris, and vaginal opening.

Vaginal discharge is a mixture of liquid, cells, and bacteria that lubricate and protect the vagina. This mixture is constantly produced by the cells of the vagina and cervix, and it exits the body through the vaginal opening. The composition, amount, and quality of discharge varies between individuals and can vary throughout the menstrual cycle and throughout the stages of sexual and reproductive development. Normal vaginal discharge may have a thin, watery consistency or a thick, sticky consistency, and it may be clear or white in color. Normal vaginal discharge may be large in volume but typically does not have a strong odor, nor is it typically associated with itching or pain. While most discharge is considered physiologic or represents normal functioning of the body, some changes in discharge can reflect infection or other pathological processes. Infections that may cause changes in vaginal discharge include vaginal yeast infections, bacterial vaginosis, and sexually transmitted infections. The characteristics of abnormal vaginal discharge vary depending on the cause, but common features include a change in color, a foul odor, and associated symptoms such as itching, burning, pelvic pain, or pain during sexual intercourse.
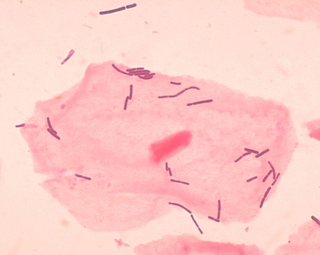
Vaginal flora, vaginal microbiota or vaginal microbiome are the microorganisms that colonize the vagina. They were discovered by the German gynecologist Albert Döderlein in 1892 and are part of the overall human flora. The amount and type of bacteria present have significant implications for an individual's overall health. The primary colonizing bacteria of a healthy individual are of the genus Lactobacillus, such as L. crispatus, and the lactic acid they produce is thought to protect against infection by pathogenic species.
A vaginal disease is a pathological condition that affects part or all of the vagina.
Female genital disease is a disorder of the structure or function of the female reproductive system that has a known cause and a distinctive group of symptoms, signs, or anatomical changes. The female reproductive system consists of the ovaries, fallopian tubes, uterus, vagina, and vulva. Female genital diseases can be classified by affected location or by type of disease, such as malformation, inflammation, or infection.
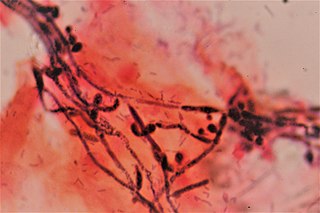
Vaginal yeast infection, also known as candidal vulvovaginitis and vaginal thrush, is excessive growth of yeast in the vagina that results in irritation. The most common symptom is vaginal itching, which may be severe. Other symptoms include burning with urination, a thick, white vaginal discharge that typically does not smell bad, pain during sex, and redness around the vagina. Symptoms often worsen just before a woman's period.

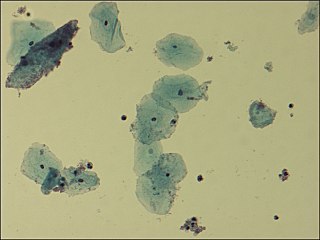
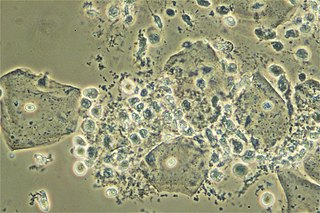
A vaginal wet mount is a gynecologic test wherein a sample of vaginal discharge is observed by wet mount microscopy by placing the specimen on a glass slide and mixing with a salt solution. It is used to find the cause of vaginitis and vulvitis.
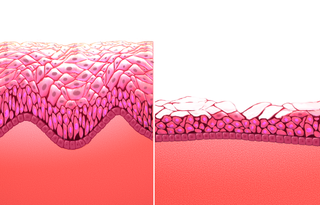
Atrophic vaginitis is inflammation of the vagina as a result of tissue thinning due to not enough estrogen. Symptoms may include pain with sex, vaginal itchiness or dryness, and an urge to urinate or burning with urination. It generally does not resolve without ongoing treatment. Complications may include urinary tract infections.
The vaginal flora in pregnancy, or vaginal microbiota in pregnancy, is different from the vaginal flora before sexual maturity, during reproductive years, and after menopause. A description of the vaginal flora of pregnant women who are immunocompromised is not covered in this article. The composition of the vaginal flora significantly differs in pregnancy. Bacteria or viruses that are infectious most often have no symptoms.
Aerobic vaginitis (AV) is a form of vaginitis first described by Donders et al. in 2002. It is characterized by a more or less severe disruption of the lactobacillary flora, along with inflammation, atrophy, and the presence of a predominantly aerobic microflora, composed of enteric commensals or pathogens.

The vaginal epithelium is the inner lining of the vagina consisting of multiple layers of (squamous) cells. The basal membrane provides the support for the first layer of the epithelium-the basal layer. The intermediate layers lie upon the basal layer, and the superficial layer is the outermost layer of the epithelium. Anatomists have described the epithelium as consisting of as many as 40 distinct layers of cells. The mucus found on the epithelium is secreted by the cervix and uterus. The rugae of the epithelium create an involuted surface and result in a large surface area that covers 360 cm2. This large surface area allows the trans-epithelial absorption of some medications via the vaginal route.

Lactobacillus vaccines are used in the therapy and prophylaxis of non-specific bacterial vaginitis and trichomoniasis. The vaccines consist of specific inactivated strains of Lactobacilli, called "aberrant" strains in the relevant literature dating from the 1980s. These strains were isolated from the vaginal secretions of patients with acute colpitis. The lactobacilli in question are polymorphic, often shortened or coccoid in shape and do not produce an acidic, anti-pathogenic vaginal environment. A colonization with aberrant lactobacilli has been associated with an increased susceptibility to vaginal infections and a high rate of relapse following antimicrobial treatment. Intramuscular administration of inactivated aberrant lactobacilli provokes a humoral immune response. The production of specific antibodies both in serum and in the vaginal secretion has been demonstrated. As a result of the immune stimulation, the abnormal lactobacilli are inhibited, the population of normal, rod-shaped lactobacilli can grow and exert its defense functions against pathogenic microorganisms.
LACTIN-V, also known as CTV-05 or as Lactobacillus crispatus CTV-05, is a live biopharmaceutical medication containing a strain of Lactobacillus crispatus (L. crispatus) which is under development for the treatment of urinary tract infections (UTIs) and bacterial vaginosis (BV). It is administered intravaginally and is described as the first vaginal microbiome (VMB)-based live biotherapeutic product (LBP). Depletion of hydrogen peroxide (H2O2)-producing Lactobacillus strains such as Lactobacillus crispatus in the vagina has been strongly associated with BV and UTIs. Most commercially available probiotic Lactobacillus strains are not vaginal strains and do not appear to improve vaginal or urinary health outcomes. The Centers for Disease Control and Prevention (CDC)'s Sexually Transmitted Infections Treatment Guidelines (2021) noted that intravaginal LACTIN-V produced a considerably lower recurrence of BV following initial antibiotic treatment with metronidazole in a randomized controlled trial. However, the guidelines also noted that LACTIN-V is not yet Food and Drug Administration (FDA)-approved or commercially available. As of December 2021, LACTIN-V is in phase 2/3 clinical trials for the treatment of UTIs and is in phase 2 trials for the treatment of BV. It was originated by GyneLogix and is under development by Osel Inc., the National Institute of Allergy and Infectious Diseases, and other organizations.

TOL-463 is an anti-infective medication which is under development for the treatment of bacterial vaginosis (BV) and vulvovaginal candidiasis (VVC). It is a boric acid-based vaginal anti-infective enhanced with ethylenediaminetetraacetic acid (EDTA) which was designed to have improved activity against vaginal bacterial and fungal biofilms while sparing protective lactobacilli. EDTA enhances the antimicrobial activity of boric acid and improves its efficacy against relevant biofilms. In a small phase 2 randomized controlled trial, TOL-463 as an insert or gel achieved clinical cure rates of 50–59% against BV and 81–92% against VVC in women who had one or both conditions. It was effective and safe in the study, though it was without indication of superiority over other antifungal medications for VVC. The cure rates against BV with TOL-463 were said to be comparable to those with recently approved antibiotic treatments like single-dose oral secnidazole (58%) and single-dose metronidazole vaginal gel (41%). As of May 2019, TOL-463 is in phase 2 clinical trials for the treatment of BV and VVC. It was originated by Toltec Pharmaceuticals and is under development by Toltec Pharmaceuticals and the National Institute of Allergy and Infectious Diseases.
References
- 1 2 3 4 5 6 7 "Vaginitis". NICHD. 2016. Retrieved October 14, 2018.
- 1 2 3 4 5 6 "What causes vaginitis?". NICHD. 2016. Retrieved October 14, 2018.
- 1 2 3 4 5 6 7 8 "Overview of Vaginitis". Merck Manuals Professional Edition. May 2018. Retrieved October 14, 2018.
- 1 2 3 4 "Vaginitis". ACOG. September 2017. Retrieved October 14, 2018.
- ↑ Ferri FF (2016). Ferri's Clinical Advisor 2017 E-Book: 5 Books in 1. Elsevier Health Sciences. p. 1333. ISBN 9780323448383.
- ↑ Beyitler İ, Kavukcu S (April 2017). "Clinical presentation, diagnosis and treatment of vulvovaginitis in girls: a current approach and review of the literature". World Journal of Pediatrics. 13 (2): 101–105. doi:10.1007/s12519-016-0078-y. PMID 28083751. S2CID 23511706.
- ↑ Romano ME (September 2020). "Prepubertal Vulvovaginitis". Clinical Obstetrics and Gynecology. 63 (3): 479–485. doi:10.1097/GRF.0000000000000536. PMID 32282354. S2CID 215758924.
- 1 2 Paladine HL, Desai UA (March 1, 2018). "Vaginitis: Diagnosis and Treatment". American Family Physician. 97 (5): 321–329. PMID 29671516.
- 1 2 3 4 5 "Trichomoniasis." Gale: Contemporary Women's Issues. HealthyWomen, Dec. 2010. Web. April 7, 2011.
- ↑ Rose L (April 20, 2020). "Postpartum Vaginal Odor - Treating Feminine Odor After a Baby".
- 1 2 3 "Bacterial Vaginosis." Gale: Contemporary Women's Issues. HealthyWomen, Dec. 2010. Web. April 7, 2011.
- ↑ Kissinger P, Adamski, A (September 2013). "Trichomoniasis and HIV interactions: a review". Sexually Transmitted Infections. 89 (6): 426–33. doi:10.1136/sextrans-2012-051005. PMC 3748151 . PMID 23605851.
- 1 2 Petrova MI, Lievens E, Malik S, Imholz N, Lebeer S (2015). "Lactobacillus species as biomarkers and agents that can promote various aspects of vaginal health". Frontiers in Physiology. 6: 81. doi: 10.3389/fphys.2015.00081 . ISSN 1664-042X. PMC 4373506 . PMID 25859220.
- ↑ Mastromarino P, Vitali B, Mosca L (2013). "Bacterial vaginosis: a review on clinical trials with probiotics" (PDF). New Microbiologica. 36 (3): 229–238. PMID 23912864.
- ↑ Donders GG, Vereecken A, Bosmans E, Dekeersmaecker A, Salembier G, Spitz B (January 2002). "Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis". BJOG. 109 (1): 34–43. doi:10.1111/j.1471-0528.2002.00432.x. hdl: 10067/1033820151162165141 . PMID 11845812. S2CID 8304009.
- ↑ Hudson T (2007). Women's Encyclopedia of Natural Medicine. New York: McGraw-Hill. ISBN 978-0-07-146473-4.
- ↑ Musthyala NB, Indulkar S, Palwai VR, Babaiah M, Ali MA, Marriapam P (April 2019). "Amebic infection of the female genital tract: a report of three cases". Journal of Mid-Life Health. 10 (2): 96–98. doi: 10.4103/jmh.JMH_152_18 . PMC 6643709 . PMID 31391760.
- ↑ "Yeast Infections With Diabetes – Diabetes and Yeast Infections". Archived from the original on February 2, 2009. Retrieved January 26, 2009.
- ↑ Northrup C (2010). Women's Bodies, Women's Wisdom: Creating Physical and Emotional Health and Healing. New York: Bantam. pp. 297–9.
- ↑ Choices NH (2018). "What causes a woman to bleed after sex? - Health questions - NHS Choices" . Retrieved February 7, 2018.
- 1 2 "Yeast Infections." Gale: Contemporary Women's Issues. HealthyWomen, Dec. 2010. Web. April 7, 2011.
- ↑ Sobel JD, Reichman O, Misra D, Yoo W (April 2011). "Prognosis and treatment of desquamative inflammatory vaginitis". Obstet Gynecol. 117 (4): 850–5. doi:10.1097/AOG.0b013e3182117c9e. PMID 21422855. S2CID 205473642.
- ↑ Tansarli GS, Kostaras EK, Athanasiou S, Falagas ME (2013). "Prevalence and treatment of aerobic vaginitis among non-pregnant women: evaluation of the evidence for an underestimated clinical entity". European Journal of Clinical Microbiology & Infectious Diseases. 32 (8): 977–84. doi:10.1007/s10096-013-1846-4. PMID 23443475. S2CID 14514975.
- ↑ Vulvovaginal atrophy and atrophic vaginitis have been the preferred terms for this condition and cluster of symptoms until recently. These terms are now regarded as inaccurate in describing changes to the whole genitourinary system occurring after menopause. The term atrophic vaginitis suggests that the vaginal is inflamed or infected. Though this may be true, inflammation and infection are not the major components of postmenopausal changes to the vagina after menopause. The former terms do not describe the negative effects on the lower urinary tract which can be the most troubling symptoms of menopause for women.
- ↑ Portman D, Gass M (2014). "Genitourinary syndrome of menopause: New terminology for vulvovaginal atrophy from the International Society for the Study of Women's Sexual Health and The North American Menopause Society". Maturitas. 79 (3): 349–354. doi:10.1016/j.maturitas.2014.07.013. PMID 25179577.
- 1 2 NHS Choices, United Kingdom National Health Service -Preventing vaginal thrush, reviewed 2012-02-17, retrieved June 10, 2013
- ↑ Vaginal Health Organization How to avoid getting a Vaginal Yeast Infection July 10, 2010
- ↑ Anukam K, Osazuwa E, Ahonkhai I, Ngwu M, Osemene G, Bruce AW, Reid G (May 2006). "Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial". Microbes Infect. 8 (6): 1450–4. doi:10.1016/j.micinf.2006.01.003. PMID 16697231.
- ↑ Vujic G, Jajac Knez A, Despot Stefanovic V, Kuzmic Vrbanovic V (May 2013). "Efficacy of orally applied probiotic capsules for bacterial vaginosis and other vaginal infections: a double-blind, randomized, placebo-controlled study". Eur J Obstet Gynecol Reprod Biol. 168 (1): 75–9. doi:10.1016/j.ejogrb.2012.12.031. PMID 23395559.
- ↑ Bradshaw CS, Pirotta M, De Guingand D, Hocking JS, Morton AN, Garland SM, Fehler G, Morrow A, Walker S. (April 2012). "Efficacy of oral metronidazole with vaginal clindamycin or vaginal probiotic for bacterial vaginosis: randomised placebo-controlled double-blind trial". PLOS ONE. 7 (4): e34540. Bibcode:2012PLoSO...734540B. doi: 10.1371/journal.pone.0034540 . PMC 3317998 . PMID 22509319.
- ↑ Senok AC, Verstraelen H, Temmerman M, Botta GA (October 2009). "Probiotics for the treatment of bacterial vaginosis". Cochrane Database Syst Rev (4): CD006289. doi:10.1002/14651858.CD006289.pub2. PMID 19821358.
- ↑ Sherrard J, Ison, C, Moody, J, Wainwright, E, Wilson, J, Sullivan, A (March 10, 2014). "United Kingdom National Guideline on the Management of Trichomonas vaginalis 2014". International Journal of STD & AIDS. 25 (8): 541–549. doi:10.1177/0956462414525947. PMID 24616117. S2CID 7181478.
- ↑ Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, Reboli AC, Schuster MG, Vazquez JA, Walsh TJ, Zaoutis TE, Sobel JD (December 16, 2015). "Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America". Clinical Infectious Diseases. 62 (4): e1–50. doi:10.1093/cid/civ933. PMC 4725385 . PMID 26679628.
- ↑ Wang C, Han C, Geng N, Fan A, Wang Y, Yue Y, Zhang H, Xue F (2016). "Efficacy of oral moxifloxacin for aerobic vaginitis". European Journal of Clinical Microbiology & Infectious Diseases. 35 (1): 95–101. doi:10.1007/s10096-015-2513-8. PMID 26526787. S2CID 15238909.
- ↑ Donders GG, Ruban K, Bellen G (2015). "Selecting Anti-Microbial Treatment of Aerobic Vaginitis". Current Infectious Disease Reports. 17 (5): 477. doi:10.1007/s11908-015-0477-6. PMID 25896749. S2CID 34979527.
- ↑ Mendling W, Weissenbacher ER, Gerber S, Prasauskas V, Grob P (2016). "Use of locally delivered dequalinium chloride in the treatment of vaginal infections: a review". Archives of Gynecology and Obstetrics. 293 (3): 469–84. doi:10.1007/s00404-015-3914-8. PMC 4757629 . PMID 26506926.
- 1 2 Huang Y, Shen C, Shen Y, Cui H (January 2024). "Assessing the Efficacy of Clotrimazole and Metronidazole Combined Treatment in Vaginitis: A Meta-Analysis". Altern Ther Health Med. 30 (1): 186–191. PMID 37773671.
- ↑ Wu YQ, Tong T (2023). "Curcumae Rhizoma: A botanical drug against infectious diseases". Frontiers in Pharmacology. 13. doi: 10.3389/fphar.2022.1015098 . PMC 9871392 . PMID 36703758.
- ↑ Benyas D, Sobel JD (2022). "Mixed Vaginitis Due to Bacterial Vaginosis and Candidiasis". Journal of Lower Genital Tract Disease. 26 (1): 68–70. doi:10.1097/LGT.0000000000000641. PMID 34840242. S2CID 244713847.
- 1 2 Hoffman B, Schorge J, Bradshaw K, Halvorson L, Schaffer J, Corton MM (April 22, 2016). Williams Gynecology, Third Edition. McGraw Hill Professional. ISBN 9780071849098.