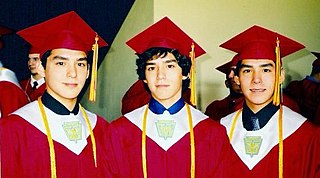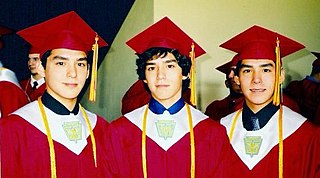
A multiple birth is the culmination of one multiple pregnancy, where in the mother gives birth to two or more babies. A term most applicable to vertebrate species, multiple births occur in most kinds of mammals, with varying frequencies. Such births are often named according to the number of offspring, as in twins and triplets. In non-humans, the whole group may also be referred to as a litter, and multiple births may be more common than single births. Multiple births in humans are the exception and can be exceptionally rare in the largest mammals.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

The chorion is the outermost fetal membrane around the embryo in mammals, birds and reptiles (amniotes). It develops from an outer fold on the surface of the yolk sac, which lies outside the zona pellucida, known as the vitelline membrane in other animals. In insects, it is developed by the follicle cells while the egg is in the ovary. Some mollusks also have chorions as part of their eggs. For example, fragile octopus eggs have only a chorion as their envelope.

Selective reduction is the practice of reducing the number of fetuses in a multiple pregnancy, such as quadruplets, to a twin or singleton pregnancy. The procedure is also called multifetal pregnancy reduction. The procedure is most commonly done to reduce the number of fetuses in a multiple pregnancy to a safe number, when the multiple pregnancy is the result of use of assisted reproductive technology; outcomes for both the mother and the babies are generally worse the higher the number of fetuses. The procedure is also used in multiple pregnancies when one of the fetuses has a serious and incurable disease, or in the case where one of the fetuses is outside the uterus, in which case it is called selective termination.

Obstetric ultrasonography, or prenatal ultrasound, is the use of medical ultrasonography in pregnancy, in which sound waves are used to create real-time visual images of the developing embryo or fetus in the uterus (womb). The procedure is a standard part of prenatal care in many countries, as it can provide a variety of information about the health of the mother, the timing and progress of the pregnancy, and the health and development of the embryo or fetus.

A molar pregnancy, also known as a hydatidiform mole, is an abnormal form of pregnancy in which a non-viable fertilized egg implants in the uterus. It falls under the category of gestational trophoblastic diseases. During a molar pregnancy, the uterus contains a growing mass characterized by swollen chorionic villi, resembling clusters of grapes. The occurrence of a molar pregnancy can be attributed to the fertilized egg lacking an original maternal nucleus. As a result, the products of conception may or may not contain fetal tissue. These molar pregnancies are categorized into two types: partial moles and complete moles, where the term 'mole' simply denotes a clump of growing tissue or a ‘growth'.

Twin-to-twin transfusion syndrome (TTTS), also known as feto-fetal transfusion syndrome (FFTS), twin oligohydramnios-polyhydramnios sequence (TOPS) and stuck twin syndrome, is a complication of monochorionic multiple pregnancies in which there is disproportionate blood supply between the fetuses. This leads to unequal levels of amniotic fluid between each fetus and usually leads to death of the undersupplied twin and, without treatment, usually death or a range of birth defects or disabilities for a surviving twin, such as underdeveloped, damaged or missing limbs, digits or organs, especially cerebral palsy.

Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.

Hydrops fetalis or hydrops foetalis is a condition in the fetus characterized by an accumulation of fluid, or edema, in at least two fetal compartments. By comparison, hydrops allantois or hydrops amnion is an accumulation of excessive fluid in the allantoic or amniotic space, respectively.

An abdominal pregnancy is a rare type of ectopic pregnancy where the embryo or fetus is growing and developing outside the uterus, in the abdomen, and not in a fallopian tube, an ovary, or the broad ligament.

Placenta accreta occurs when all or part of the placenta attaches abnormally to the myometrium. Three grades of abnormal placental attachment are defined according to the depth of attachment and invasion into the muscular layers of the uterus:
- Accreta – chorionic villi attached to the myometrium, rather than being restricted within the decidua basalis.
- Increta – chorionic villi invaded into the myometrium.
- Percreta – chorionic villi invaded through the perimetrium.
Postterm pregnancy is when a woman has not yet delivered her baby after 42 weeks of gestation, two weeks beyond the typical 40-week duration of pregnancy. Postmature births carry risks for both the mother and the baby, including fetal malnutrition, meconium aspiration syndrome, and stillbirths. After the 42nd week of gestation, the placenta, which supplies the baby with nutrients and oxygen from the mother, starts aging and will eventually fail. Postterm pregnancy is a reason to induce labor.

A nuchal scan or nuchal translucency (NT) scan/procedure is a sonographic prenatal screening scan (ultrasound) to detect chromosomal abnormalities in a fetus, though altered extracellular matrix composition and limited lymphatic drainage can also be detected.
Placental insufficiency or utero-placental insufficiency is the failure of the placenta to deliver sufficient nutrients to the fetus during pregnancy, and is often a result of insufficient blood flow to the placenta. The term is also sometimes used to designate late decelerations of fetal heart rate as measured by cardiotocography or an NST, even if there is no other evidence of reduced blood flow to the placenta, normal uterine blood flow rate being 600mL/min.

Kyprianos "Kypros" Nicolaides is a Greek Cypriot physician of British citizenship, Professor of Fetal Medicine at King's College Hospital, London. He is one of the pioneers of fetal medicine and his discoveries have revolutionised the field. He was elected to the US National Academy of Medicine in 2020 for 'improving the care of pregnant women worldwide with pioneering rigorous and creative approaches, and making seminal contributions to prenatal diagnosis and every major obstetrical disorder'. This is considered to be one of the highest honours in the fields of health and medicine and recognises individuals who have demonstrated outstanding professional achievement and commitment to service.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.

Monoamniotic twins are identical or semi-identical twins that share the same amniotic sac within their mother's uterus. Monoamniotic twins are always monochorionic and are usually termed Monoamniotic-Monochorionic twins. They share the placenta, but have two separate umbilical cords. Monoamniotic twins develop when an embryo does not split until after formation of the amniotic sac, at about 9–13 days after fertilization. Monoamniotic triplets or other monoamniotic multiples are possible, but extremely rare. Other obscure possibilities include multiples sets where monoamniotic twins are part of a larger gestation such as triplets, quadruplets, or more.
The following outline is provided as an overview of and topical guide to obstetrics:

Twin anemia-polycythemia sequence(TAPS) is a chronic type of unbalanced fetal transfusion in monochorionic twins that results in polycythemia in the TAPS recipient and anemia in the TAPS donor due to tiny placental anastomoses. Post-laser TAPS and spontaneous TAPS are the two forms of TAPS. Unlike twin-twin transfusion syndrome, which arises when twin oligohydramnios polyhydramnios sequence (TOPS) is absent, TAPS develops in its absence.
The anomaly scan, also sometimes called the anatomy scan, 20-week ultrasound, or level 2 ultrasound, evaluates anatomic structures of the fetus, placenta, and maternal pelvic organs. This scan is an important and common component of routine prenatal care. The function of the ultrasound is to measure the fetus so that growth abnormalities can be recognized quickly later in pregnancy, to assess for congenital malformations and multiple pregnancies, and to plan method of delivery.