The placenta is a temporary embryonic and later fetal organ that begins developing from the blastocyst shortly after implantation. It plays critical roles in facilitating nutrient, gas and waste exchange between the physically separate maternal and fetal circulations, and is an important endocrine organ, producing hormones that regulate both maternal and fetal physiology during pregnancy. The placenta connects to the fetus via the umbilical cord, and on the opposite aspect to the maternal uterus in a species-dependent manner. In humans, a thin layer of maternal decidual (endometrial) tissue comes away with the placenta when it is expelled from the uterus following birth. Placentas are a defining characteristic of placental mammals, but are also found in marsupials and some non-mammals with varying levels of development.

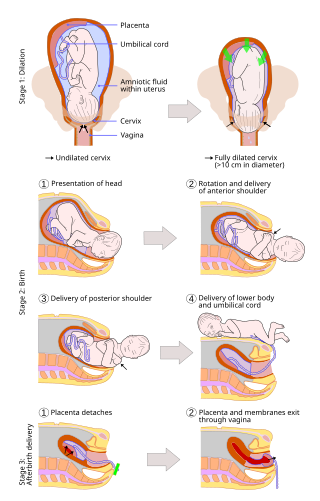
Childbirth, also known as labour, parturition and delivery, is the completion of pregnancy where one or more babies exits the internal environment of the mother via vaginal delivery or caesarean section. In 2019, there were about 140.11 million human births globally. In the developed countries, most deliveries occur in hospitals, while in the developing countries most are home births.
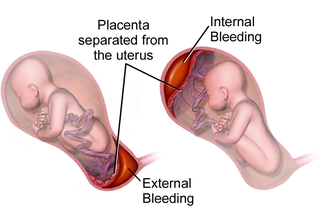
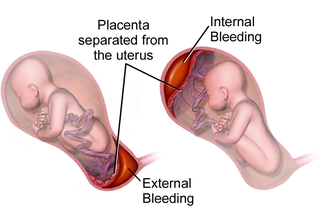
Placental abruption is when the placenta separates early from the uterus, in other words separates before childbirth. It occurs most commonly around 25 weeks of pregnancy. Symptoms may include vaginal bleeding, lower abdominal pain, and dangerously low blood pressure. Complications for the mother can include disseminated intravascular coagulopathy and kidney failure. Complications for the baby can include fetal distress, low birthweight, preterm delivery, and stillbirth.
Antepartum bleeding, also known as antepartum haemorrhage (APH) or prepartum hemorrhage, is genital bleeding during pregnancy after the 28th week of pregnancy up to delivery.
Obstetrical bleeding is bleeding in pregnancy that occurs before, during, or after childbirth. Bleeding before childbirth is that which occurs after 24 weeks of pregnancy. Bleeding may be vaginal or less commonly into the abdominal cavity. Bleeding which occurs before 24 weeks is known as early pregnancy bleeding.

Uterine atony is the failure of the uterus to contract adequately following delivery. Contraction of the uterine muscles during labor compresses the blood vessels and slows flow, which helps prevent hemorrhage and facilitates coagulation. Therefore, a lack of uterine muscle contraction can lead to an acute hemorrhage, as the vasculature is not being sufficiently compressed. Uterine atony is the most common cause of postpartum hemorrhage, which is an emergency and potential cause of fatality. Across the globe, postpartum hemorrhage is among the top five causes of maternal death. Recognition of the warning signs of uterine atony in the setting of extensive postpartum bleeding should initiate interventions aimed at regaining stable uterine contraction.

Postpartum bleeding or postpartum hemorrhage (PPH) is often defined as the loss of more than 500 ml or 1,000 ml of blood following childbirth. Some have added the requirement that there also be signs or symptoms of low blood volume for the condition to exist. Signs and symptoms may initially include: an increased heart rate, feeling faint upon standing, and an increased breathing rate. As more blood is lost, the patient may feel cold, blood pressure may drop, and they may become restless or unconscious. The condition can occur up to six weeks following delivery.
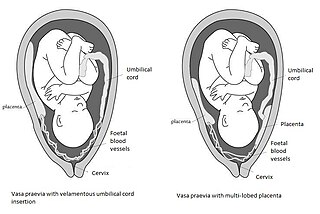
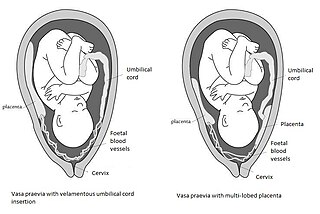
Vasa praevia is a condition in which fetal blood vessels cross or run near the internal opening of the uterus. These vessels are at risk of rupture when the supporting membranes rupture, as they are unsupported by the umbilical cord or placental tissue.

Carbetocin, sold under the brand names Pabal among others, is a medication used to prevent excessive bleeding after childbirth, particularly following Cesarean section. It appears to work as well as oxytocin. Due to it being less economical than other options, use is not recommended by NHS Scotland. It is given by injection into a vein or muscle.
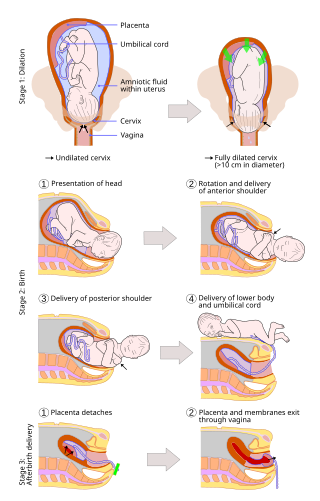
A vaginal delivery is the birth of offspring in mammals through the vagina. It is the most common method of childbirth worldwide. It is considered the preferred method of delivery, with lower morbidity and mortality than Caesarean sections (C-sections).

Uterine inversion is when the uterus turns inside out, usually following childbirth. Symptoms include postpartum bleeding, abdominal pain, a mass in the vagina, and low blood pressure. Rarely inversion may occur not in association with pregnancy.
An asynclitic birth or asynclitism are terms used in obstetrics to refer to childbirth in which there is malposition of the head of the fetus in the uterus, relative to the birth canal. Asynclitic presentation is different from a shoulder presentation, in which the shoulder is presenting first. Many babies enter the pelvis in an asynclitic presentation, and most asynclitism corrects spontaneously as part of the normal birthing process.

Velamentous cord insertion is a complication of pregnancy where the umbilical cord is inserted in the fetal membranes. It is a major cause of antepartum hemorrhage that leads to loss of fetal blood and associated with high perinatal mortality. In normal pregnancies, the umbilical cord inserts into the middle of the placental mass and is completely encased by the amniotic sac. The vessels are hence normally protected by Wharton's jelly, which prevents rupture during pregnancy and labor. In velamentous cord insertion, the vessels of the umbilical cord are improperly inserted in the chorioamniotic membrane, and hence the vessels traverse between the amnion and the chorion towards the placenta. Without Wharton's jelly protecting the vessels, the exposed vessels are susceptible to compression and rupture.
An obstetric labor complication is a difficulty or abnormality that arises during the process of labor or delivery.
A uterotonic, also known as an oxytocic or ecbolic, is a type of medication used to induce contraction or greater tonicity of the uterus. Uterotonics are used both to induce labor and to reduce postpartum hemorrhage.

Circumvallate placenta is a rare condition affecting about 1-2% of pregnancies, in which the amnion and chorion fetal membranes essentially "double back" on the fetal side around the edges of the placenta. After delivery, a circumvallate placenta has a thick ring of membranes on its fetal surface. Circumvallate placenta is a placental morphological abnormality associated with increased fetal morbidity and mortality due to the restricted availability of nutrients and oxygen to the developing fetus.

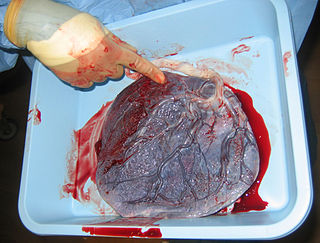
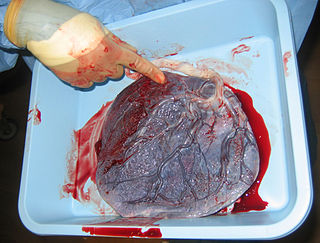
Placental expulsion occurs when the placenta comes out of the birth canal after childbirth. The period from just after the baby is expelled until just after the placenta is expelled is called the third stage of labor.

Prolonged labor is the inability of a woman to proceed with childbirth upon going into labor. Prolonged labor typically lasts over 20 hours for first time mothers, and over 14 hours for women that have already had children. Failure to progress can take place during two different phases; the latent phase and active phase of labor. The latent phase of labor can be emotionally tiring and cause fatigue, but it typically does not result in further problems. The active phase of labor, on the other hand, if prolonged, can result in long term complications.
Fundal massage, also called uterine massage, is a technique used to reduce bleeding and cramping of the uterus after childbirth or after an abortion. As the uterus returns to its nonpregnant size, its muscles contract strongly, which can cause pain. Fundal massage can be performed with one hand over the pubic bone, firmly massaging the uterine fundus, or with the addition of one hand in the vagina compressing the two uterine arteries. Routine use of fundal massage can prevent postpartum or post-abortion hemorrhage and can reduce pain; it may also reduce the need for uterotonics, medications that cause the uterus to contract. It is used to treat uterine atony, a condition where the uterus lacks muscle tone and is soft to the touch instead of firm.

Emergency childbirth is the precipitous birth of an infant in an unexpected setting. In planned childbirth, mothers choose the location and obstetric team ahead of time. Options range from delivering at home, at a hospital, a medical facility or a birthing center. Sometimes, birth can occur on the way to these facilities, without a healthcare team. The rates of unplanned childbirth are low. If the birth is imminent, emergency measures may be needed. Emergency services can be contacted for help in some countries.