| Local anesthesia | |
|---|---|
| MeSH | D000772 |
Local anesthesia is any technique to induce the absence of sensation in a specific part of the body, [1] generally for the aim of inducing local analgesia, i.e. local insensitivity to pain, although other local senses may be affected as well. It allows patients to undergo surgical and dental procedures with reduced pain and distress. In many situations, such as cesarean section, it is safer and therefore superior to general anesthesia. [2]
The following terms are often used interchangeably:
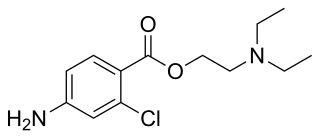
A local anesthetic is a drug that causes reversible local anesthesia and a loss of nociception. When it is used on specific nerve pathways (nerve block), effects such as analgesia (loss of pain sensation) and paralysis (loss of muscle power) can be achieved. Clinical local anesthetics belong to one of two classes: aminoamide and aminoester local anesthetics. Synthetic local anesthetics are structurally related to cocaine. They differ from cocaine mainly in that they have no abuse potential and do not act on the sympathoadrenergic system, i.e. they do not produce hypertension or local vasoconstriction, with the exception of Ropivacaine and Mepivacaine that do produce weak vasoconstriction. Unlike other forms of anesthesia, a local can be used for a minor procedure in a surgeon's office as it does not put you into a state of unconsciousness. However, the physician should have a sterile environment available before doing a procedure in their office.
Local anesthetics vary in their pharmacological properties and they are used in various techniques of local anesthesia such as:
Adverse effects depend on the local anesthetic method and site of administration discussed in depth in the local anesthetic sub-article, but overall, adverse effects can be:
Local pain management that uses other techniques than analgesic medication include:

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.

A local anesthetic (LA) is a medication that causes absence of all sensation in a specific body part without loss of consciousness, as opposed to a general anesthetic, which eliminates all sensation in the entire body and causes unconsciousness. Local anesthetics are most commonly used to eliminate pain during or after surgery. When it is used on specific nerve pathways, paralysis also can be induced.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

Transcutaneous electrical nerve stimulation is the use of electric current produced by a device to stimulate the nerves for therapeutic purposes. TENS, by definition, covers the complete range of transcutaneously applied currents used for nerve excitation although the term is often used with a more restrictive intent, namely to describe the kind of pulses produced by portable stimulators used to reduce pain. The unit is usually connected to the skin using two or more electrodes which are typically conductive gel pads. A typical battery-operated TENS unit is able to modulate pulse width, frequency, and intensity. Generally, TENS is applied at high frequency (>50 Hz) with an intensity below motor contraction or low frequency (<10 Hz) with an intensity that produces motor contraction. More recently, many TENS units use a mixed frequency mode which alleviates tolerance to repeated use. Intensity of stimulation should be strong but comfortable with greater intensities, regardless of frequency, producing the greatest analgesia. While the use of TENS has proved effective in clinical studies, there is controversy over which conditions the device should be used to treat.

Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.

The mental nerve is a sensory nerve of the face. It is a branch of the posterior trunk of the inferior alveolar nerve, itself a branch of the mandibular nerve (CN V3), itself a branch of the trigeminal nerve (CN V). It provides sensation to the front of the chin and the lower lip, as well as the gums of the anterior mandibular (lower) teeth. It can be blocked with local anaesthesia for procedures on the chin, lower lip, and mucous membrane of the inner cheek. Problems with the nerve cause chin numbness.
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.

A spinal cord stimulator (SCS) or dorsal column stimulator (DCS) is a type of implantable neuromodulation device that is used to send electrical signals to select areas of the spinal cord for the treatment of certain pain conditions. SCS is a consideration for people who have a pain condition that has not responded to more conservative therapy. There are also spinal cord stimulators under research and development that could enable patients with spinal cord injury to walk again via epidural electrical stimulation (EES).
Dental anesthesia is the application of anesthesia to dentistry. It includes local anesthetics, sedation, and general anesthesia.
Electroanalgesia is a form of analgesia, or pain relief, that uses electricity to ease pain. Electrical devices can be internal or external, at the site of pain (local) or delocalized throughout the whole body. It works by interfering with the electric currents of pain signals, inhibiting them from reaching the brain and inducing a response; different from traditional analgesics, such as opiates which mimic natural endorphins and NSAIDs that help relieve inflammation and stop pain at the source. Electroanalgesia has a lower addictive potential and poses less health threats to the general public, but can cause serious health problems, even death, in people with other electrical devices such as pacemakers or internal hearing aids, or with heart problems.

Twilight anesthesia is an anesthetic technique where a mild dose of sedation is applied to induce anxiolysis, hypnosis, and anterograde amnesia. The patient is not unconscious, but sedated. During surgery or other medical procedures, the patient is under what is known as a "twilight state", where the patient is relaxed and "sleepy", able to follow simple directions by the doctor, and is responsive. Generally, twilight anesthesia causes the patient to forget the surgery and the time right after. It is used for a variety of surgical procedures and for various reasons. Just like regular anesthesia, twilight anesthesia is designed to help a patient feel more comfortable and to minimize pain associated with the procedure being performed and to allow the medical practitioner to practice without interruptions.
Continuous wound infiltration (CWI) refers to the continuous infiltration of a local anesthetic into a surgical wound to aid in pain management during post-operative recovery.

Brachial plexus block is a regional anesthesia technique that is sometimes employed as an alternative or as an adjunct to general anesthesia for surgery of the upper extremity. This technique involves the injection of local anesthetic agents in close proximity to the brachial plexus, temporarily blocking the sensation and ability to move the upper extremity. The subject can remain awake during the ensuing surgical procedure, or they can be sedated or even fully anesthetized if necessary.
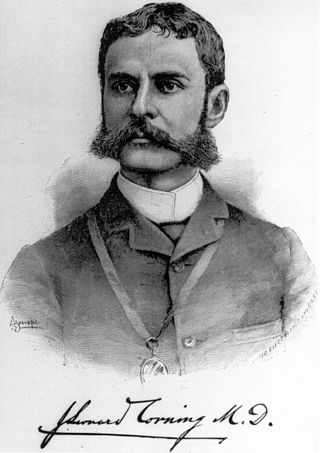
James Leonard Corning was an American neurologist, mainly known for his early experiments on neuraxial blockade in New York City.
Occipital nerve stimulation (ONS), also called peripheral nerve stimulation (PNS) of the occipital nerves, is used to treat chronic migraine patients who have failed to respond to pharmaceutical treatments.
Fascia iliaca blocks is a local anesthetic nerve block, a type of regional anesthesia technique, used to provide analgesia or anaesthesia to the hip and thigh. FICB can performed by using ultrasound or with a loss of resistance technique, the latter sometimes referred to as the "two-pop-method". FICB works by affecting the femoral, obturator and the lateral cutaneous nerves with a local anesthetic.
Obstetric anesthesia or obstetric anesthesiology, also known as ob-gyn anesthesia or ob-gyn anesthesiology, is a sub-specialty of anesthesiology that provides peripartum pain relief (analgesia) for labor and anesthesia for cesarean deliveries ('C-sections').

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults it is used for chronic low back pain management.