Related Research Articles

Caesarean section, also known as C-section or caesarean delivery, is the surgical procedure by which one or more babies are delivered through an incision in the mother's abdomen. It is often performed because vaginal delivery would put the baby or mother at risk. Reasons for the operation include obstructed labor, twin pregnancy, high blood pressure in the mother, breech birth, shoulder presentation, and problems with the placenta or umbilical cord. A caesarean delivery may be performed based upon the shape of the mother's pelvis or history of a previous C-section. A trial of vaginal birth after C-section may be possible. The World Health Organization recommends that caesarean section be performed only when medically necessary.

Anesthesia or anaesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients.

Anesthesiology, anaesthesiology, or anaesthesia is the medical specialty concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialized in anesthesiology is called an anesthesiologist, anaesthesiologist, or anaesthetist, depending on the country. In some countries the terms are synonymous, while in other countries they refer to different positions and anesthetist is only used for non-physicians, such as nurse anesthetists.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory of the experience, it is also possible for victims to have awareness with explicit recall, where they can remember the events related to their surgery.

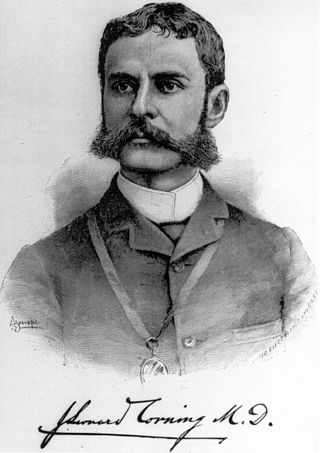
Epidural administration is a method of medication administration in which a medicine is injected into the epidural space around the spinal cord. The epidural route is used by physicians and nurse anesthetists to administer local anesthetic agents, analgesics, diagnostic medicines such as radiocontrast agents, and other medicines such as glucocorticoids. Epidural administration involves the placement of a catheter into the epidural space, which may remain in place for the duration of the treatment. The technique of intentional epidural administration of medication was first described in 1921 by Spanish military surgeon Fidel Pagés.
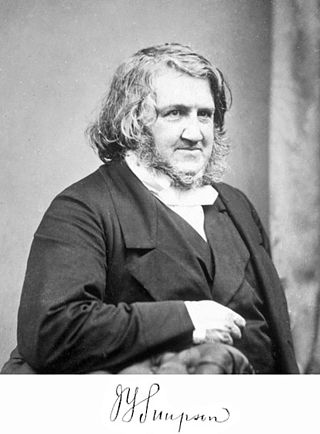
Sir James Young Simpson, 1st Baronet,, was a Scottish obstetrician and a significant figure in the history of medicine. He was the first physician to demonstrate the anaesthetic properties of chloroform on humans and helped to popularise its use in medicine.

Bupivacaine, marketed under the brand name Marcaine among others, is a medication used to decrease feeling in a specific area. In nerve blocks, it is injected around a nerve that supplies the area, or into the spinal canal's epidural space. It is available mixed with a small amount of epinephrine to increase the duration of its action. It typically begins working within 15 minutes and lasts for 2 to 8 hours.
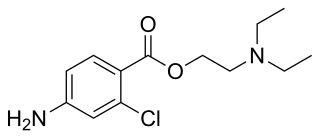
Chloroprocaine is a local anesthetic given by injection during surgical procedures and labor and delivery. Chloroprocaine vasodilates; this is in contrast to cocaine which vasoconstricts. Chloroprocaine is an ester anesthetic.

Methoxyflurane, sold under the brand name Penthrox among others, is an inhaled medication primarily used to reduce pain following trauma. It may also be used for short episodes of pain as a result of medical procedures. Onset of pain relief is rapid and of a short duration. Use is only recommended with direct medical supervision.

Patient-controlled analgesia (PCA) is any method of allowing a person in pain to administer their own pain relief. The infusion is programmable by the prescriber. If it is programmed and functioning as intended, the machine is unlikely to deliver an overdose of medication. Providers must always observe the first administration of any PCA medication which has not already been administered by the provider to respond to allergic reactions.

Throughout recorded history, attempts at producing a state of general anesthesia can be traced back to the writings of ancient Sumerians, Babylonians, Assyrians, Egyptians, Indians, and Chinese. Despite significant advances in anatomy and surgical technique during the Renaissance, surgery remained a last-resort treatment largely due to the pain associated with it. However, scientific discoveries in the late 18th and early 19th centuries paved the way for the development of modern anesthetic techniques.
The following outline is provided as an overview of and topical guide to anesthesia:
The history of neuraxial anaesthesia dates back to the late 1800s and is closely intertwined with the development of anaesthesia in general. Neuraxial anaesthesia, in particular, is a form of regional analgesia placed in or around the Central Nervous System, used for pain management and anaesthesia for certain surgeries and procedures.

No Pain Labor & Delivery – Global Health Initiative is a non-for-profit organization. Founded in 2006, the program focuses on correcting the unnecessarily high caesarean delivery rate and the poor utilization of neuraxial labor analgesia in China.

Pain management during childbirth is the treatment or prevention of pain that a woman may experience during labor and delivery. The amount of pain a woman feels during labor depends partly on the size and position of her baby, the size of her pelvis, her emotions, the strength of the contractions, and her outlook. Tension increases pain during labor. Virtually all women worry about how they will cope with the pain of labor and delivery. Childbirth is different for each woman and predicting the amount of pain experienced during birth and delivery can not be certain.
Gertie Florentine Marx (1912-2004) was an obstetric anesthesiologist, "internationally known as 'the mother of obstetric anaesthesia'". Marx pioneered the use of epidural analgesia during childbirth, and was the founding editor of the quarterly Obstetric Anesthesia Digest.

Caudal anaesthesia is a form of neuraxial regional anaesthesia conducted by accessing the epidural space via the sacral hiatus. It is typically used in paediatrics to provide peri- and post-operative analgesia for surgeries below the umbilicus. In adults it is used for chronic low back pain management.
References
- ↑ "Medical Definition of PERIPARTUM". www.merriam-webster.com.
- ↑ Stoelting RK, Miller RD (2007). Basics of anesthesia. Philadelphia: Churchill Livingstone. p. 515. ISBN 978-81-312-2898-2.
{{cite book}}: CS1 maint: location missing publisher (link) - ↑ Ramanathan, Sivam (1988). Obstetric Anesthesia. Philadelphia, PA: Lee & Febiger. pp. vii. ISBN 978-0-8121-1118-7.
- 1 2 3 4 Aaronson, Jaime; Goodman, Stephanie (2014). "Obstetric anesthesia: Not just for cesareans and labor". Seminars in Perinatology. 38 (6, October 2014): 378–385. doi:10.1053/j.semperi.2014.07.005. ISSN 0146-0005. PMID 25146107.
- ↑ Gordon, Henry L. Sir James Young Simpson and Chloroform (1811-1870). Ed. Ernest Hart. Pasternoster Square, London: Urwin, 1897. Masters of Medicine. Web. 2017.
- ↑ Whitfield A (2014). "A short history of Obstetric Anaesthesia". Res Medica. 3 (1). doi: 10.2218/resmedica.v3i1.972 . ISSN 2051-7580.
- 1 2 3 4 5 6 7 8 9 Marx, Gertie F.; Bassell, Gerard M. (1980). Obstetric Analgesia and Anaesthesia. The Netherlands: Elsevier/North-Holland Biomedical Press. pp. 1, 5–8, 10, 12–13. ISBN 978-0-444-80137-1.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Ramanathan, Sivam (1988). Obstetric anesthesia. Philadelphia, PA: Lea & Febiger. pp. 3–4. ISBN 978-0-8121-1118-7.
- 1 2 3 Miller, Ronald D.; Pardo, Manuel C. Jr. (2012). Basics of anesthesia (6th ed.). Elsevier/Saunders. pp. 5–6. ISBN 978-81-312-2898-2. OCLC 742301032.
- 1 2 3 Tolmie, John D.; Birch, Alexander (1986). Anesthesia for the uninterested (2nd ed.). Rockville, Md: Aspen Publishers. p. 163. ISBN 978-0871892966.
- ↑ Swayne, J. G. (1875). "Obstetrical Statistics". The British Medical Journal. 2 (777): 635–638. doi:10.1136/bmj.2.777.635. JSTOR 25242218. PMC 2297735 . PMID 20748025.
- ↑ Snow, John (1853). "On the Administration of Chloroform during Parturition". Association Medical Journal. 1 (23): 500–502. doi:10.1136/bmj.s3-1.23.500. JSTOR 25494691. PMC 2449612 . PMID 20740854.
- ↑ Gordon, Henry L. Sir James Young Simpson and Chloroform (1811-1870). Ed. Ernest Hart.
- ↑ Simpson, J. Y. (1853). "The Propriety and Morality of Using Anæsthetics in Instrumental and Natural Parturition". Association Medical Journal. 1 (27): 582–589. JSTOR 25494769.
- ↑ Simpson, J.Y. (January 1959). "Answer to the Religious Objections Advanced against the Employment of Anaesthetic Agents in Midwifery and Surgery". British Journal of Anaesthesia. 31 (1): 35–43. doi: 10.1093/bja/31.1.35 . PMC 5199347 .
- ↑ Beatty, Thomas Edward (1869). "Address In Midwifery, Delivered At The Thirty-Seventh Annual Meeting Of The British Medical Association, Held In Leeds, July 27th, 28th, 29th, And 30th, 1869". The British Medical Journal. 2 (449): 137–143. doi:10.1136/bmj.2.449.137. JSTOR 25217099. S2CID 71208772.
- ↑ Caton, Donald (1 January 2000). "John Snow's Practice of Obstetric Anesthesia". Anesthesiology. 92 (1): 247–252. doi: 10.1097/00000542-200001000-00037 . PMID 10638922. S2CID 8117674.
- ↑ "Obstetrical Society Of London". The British Medical Journal. 1 (105): 15–17. 1859. JSTOR 25192989.
- ↑ Simpson, J. Y. (1848). "Letter in Reply to Dr. Collins, on the Duration of Labour as a Cause of Danger and Mortality to the Mother and Infant". Provincial Medical and Surgical Journal. 12 (22): 601–606. JSTOR 25500540.
- ↑ Camann W, Lim MN, Ong S, Yeh PS (July 2002). "Has medicalisation of childbirth gone too far?". BMJ. 325 (7355): 103–104. doi:10.1136/bmj.325.7355.103. JSTOR 25451822. PMC 1123599 . PMID 12114249.
- ↑ Leavitt JW (1983). ""Science" enters the birthing room: obstetrics in America since the eighteenth century". J Am Hist. 70 (2): 281–304. doi:10.2307/1900205. JSTOR 1900205. PMID 11614690.
- 1 2 Miller, Ronald D.; Pardo, Manuel C. (2011-01-01). Basics of anesthesia . Elsevier/Saunders. pp. 22–23, 337–338. ISBN 978-8131228982. OCLC 742301032.
- 1 2 3 4 H., Davies, N. J.; N., Cashman, Jeremy; B.)., Rushman, G. B. Geoffrey (2005-01-01). Lee's synopsis of anaesthesia. Elsevier/Butterworth Heinemann. pp. 660–662. OCLC 61303532.
{{cite book}}: CS1 maint: multiple names: authors list (link) - 1 2 3 4 5 6 7 8 9 10 Miller, Ronald D.; Pardo, Manuel C. Jr. (2011-01-01). Basics of anesthesia . Elsevier/Saunders. pp. 521–529. ISBN 978-81-312-2898-2. OCLC 742301032.
- ↑ Cluett, ER; Burns, E; Cuthbert, A (16 May 2018). "Immersion in water during labour and birth". The Cochrane Database of Systematic Reviews. 5 (6): CD000111. doi:10.1002/14651858.CD000111.pub4. PMC 6494420 . PMID 29768662.
- ↑ Hodnett, Ellen D.; Gates, Simon; Hofmeyr, G. Justus; Sakala, Carol (2012-10-17). Hodnett, Ellen D (ed.). "Continuous support for women during childbirth". The Cochrane Database of Systematic Reviews. 10: CD003766. doi:10.1002/14651858.CD003766.pub4. ISSN 1469-493X. PMC 4175537 . PMID 23076901.
- ↑ White, Leigh D.; Thang, Christopher; Hodsdon, Anthony; Melhuish, Thomas M.; Barron, Fiona A.; Godsall, M. Guy; Vlok, Ruan (January 2020). "Comparison of Supraglottic Airway Devices With Endotracheal Intubation in Low-Risk Patients for Cesarean Delivery". Anesthesia & Analgesia: 1. doi: 10.1213/ANE.0000000000004618 . PMID 31923002. S2CID 210149430.
- ↑ White, L.D.; Hodsdon, A.; An, G.H.; Thang, C.; Melhuish, T.M.; Vlok, R. (May 2019). "Induction opioids for caesarean section under general anaesthesia: a systematic review and meta-analysis of randomised controlled trials". International Journal of Obstetric Anesthesia. 40: 4–13. doi: 10.1016/j.ijoa.2019.04.007 . hdl: 10072/416502 . PMID 31230994.
- 1 2 3 "American Society of Anesthesiologists - How to Prepare for a Career in Anesthesiology". www.asahq.org. Retrieved 2016-12-08.
- 1 2 Miller, Ronald D.; Pardo, Manuel C. Jr. (2011-01-01). Basics of anesthesia . Elsevier/Saunders. pp. 12–13. ISBN 9788131228982. OCLC 742301032.
- ↑ Miller, Ronald; Pardo, Manuel (2012). Basics of anesthesia . Elsevier/Saunders. pp. 372–373. ISBN 9781437716146. OCLC 742301032.
- ↑ "Why Don't Jehovah's Witnesses Accept Blood Transfusions?" . Retrieved 2016-12-16.
- ↑ "Essential learning: Law and ethics" . Retrieved 2016-12-16.
- ↑ Dixon, J. Lowell; Smalley, MG (27 November 1981). "Jehovah's Witnesses: The Surgical/Ethical Challenge". JAMA. 246 (21): 2471–2472. doi:10.1001/jama.1981.03320210037021. PMID 7299971.
- ↑ "How Can Blood Save Your Life?" . Retrieved 2016-12-16.