Orthopedic surgery or orthopedics is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors, and congenital disorders.

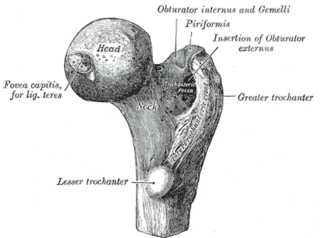
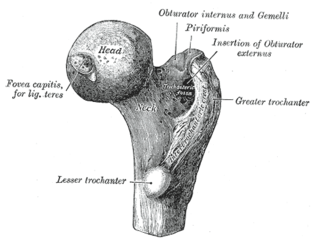
Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant, that is, a hip prosthesis. Hip replacement surgery can be performed as a total replacement or a hemi (half) replacement. Such joint replacement orthopaedic surgery is generally conducted to relieve arthritis pain or in some hip fractures. A total hip replacement consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is one of the most common orthopaedic operations, though patient satisfaction varies widely. Approximately 58% of total hip replacements are estimated to last 25 years. The average cost of a total hip replacement in 2012 was $40,364 in the United States, and about $7,700 to $12,000 in most European countries.
Arthroplasty is an orthopedic surgical procedure where the articular surface of a musculoskeletal joint is replaced, remodeled, or realigned by osteotomy or some other procedure. It is an elective procedure that is done to relieve pain and restore function to the joint after damage by arthritis or some other type of trauma.
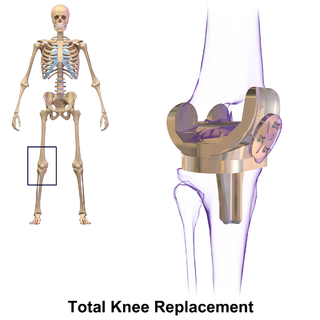
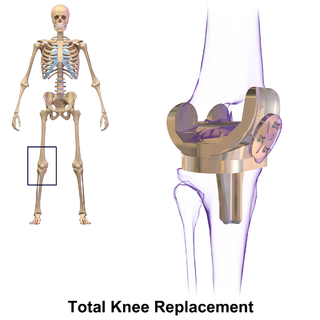
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources. It may also be performed for other knee diseases, such as rheumatoid arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation, and is not a reason to perform knee replacement.

Computer-assisted orthopedic surgery or computer-assisted orthopaedic surgery is a discipline where computer technology is applied pre-, intra- and/or post-operatively to improve the outcome of orthopedic surgical procedures. Although records show that it has been implemented since the 1990s, CAOS is still an active research discipline which brings together orthopedic practitioners with traditionally technical disciplines, such as engineering, computer science and robotics.

Replacement arthroplasty, or joint replacement surgery, is a procedure of orthopedic surgery in which an arthritic or dysfunctional joint surface is replaced with an orthopedic prosthesis. Joint replacement is considered as a treatment when severe joint pain or dysfunction is not alleviated by less-invasive therapies. It is a form of arthroplasty, and is often indicated from various joint diseases, including osteoarthritis and rheumatoid arthritis.
A femoral head ostectomy is a surgical operation to remove the head and neck from the femur. It is performed to alleviate pain, and is a salvage procedure, reserved for condition where pain can not be alleviated in any other way. It is common in veterinary surgery. Other names are excision arthroplasty of the femoral head and neck, Girdlestone's operation, Girdlestone procedure, and femoral head and neck ostectomy.
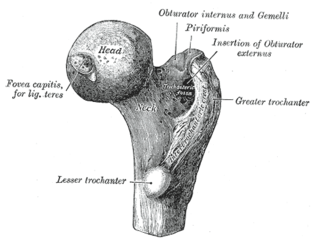
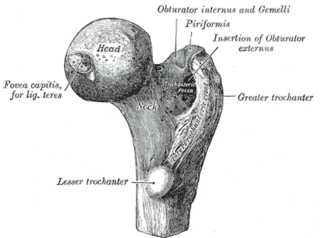
The femoral neck is a flattened pyramidal process of bone, connecting the femoral head with the femoral shaft, and forming with the latter a wide angle opening medialward.
Artificial disc replacement (ADR), or total disc replacement (TDR), is a type of arthroplasty. It is a surgical procedure in which degenerated intervertebral discs in the spinal column are replaced with artificial disc implants in the lumbar (lower) or cervical (upper) spine. The procedure is used to treat chronic, severe low back pain and cervical pain resulting from degenerative disc disease. Disc replacement is also an alternative intervention for symptomatic disc herniation with associated arm and hand, or leg symptoms.

Unicompartmental knee arthroplasty (UKA) is a surgical procedure used to relieve arthritis in one of the knee compartments in which the damaged parts of the knee are replaced. UKA surgery may reduce post-operative pain and have a shorter recovery period than a total knee replacement procedure, particularly in people over 75 years of age. Moreover, UKAs may require a smaller incision, less tissue damage, and faster recovery times.
Minimally invasive hip resurfacing (MIS) is a total or partial hip surgery that can be carried out through an incision of less than 10 cm without imparting great forces on the anatomy or compromising component positioning.
Femoral neck targeting is the process of calculating the centre of the femoral neck during hip resurfacing surgery. This can be done by hand or using electronic aides.
Ankle replacement, or ankle arthroplasty, is a surgical procedure to replace the damaged articular surfaces of the human ankle joint with prosthetic components. This procedure is becoming the treatment of choice for patients requiring arthroplasty, replacing the conventional use of arthrodesis, i.e. fusion of the bones. The restoration of range of motion is the key feature in favor of ankle replacement with respect to arthrodesis. However, clinical evidence of the superiority of the former has only been demonstrated for particular isolated implant designs.
"Professor" Derek McMinn is a British orthopaedic surgeon and inventor who practised in Birmingham, United Kingdom at the BMI Edgbaston Hospital. McMinn developed one of the successful modern metal-on-metal hip resurfacing and the instrumentation and surgical technique to implant it. Hip resurfacing is a bone-conserving, less invasive alternative to total hip replacement (THR) for young patients, markedly improves the health-related quality of life measures and currently makes up around a twentieth of all hip arthroplasty procedures performed in the United Kingdom. McMinn is also the inventor of several other prostheses for the hip and knee.
Metallosis is the medical condition involving deposition and build-up of metal debris in the soft tissues of the body.
Limb-sparing techniques, also known as limb-saving or limb-salvage techniques, are performed in order to preserve the look and function of limbs. Limb-sparing techniques are used to preserve limbs affected by trauma, arthritis, cancers such as high-grade bone sarcomas, and vascular conditions such as diabetic foot ulcers. As the techniques for chemotherapy, radiation, and diagnostic modalities improve, there has been a trend toward limb-sparing procedures to avoid amputation, which has been associated with a lower 5-year survival rate and cost-effectiveness compared to limb salvage in the long-run. There are many different types of limb-sparing techniques, including arthrodesis, arthroplasty, endoprosthetic reconstruction, various types of implants, rotationplasty, osseointegration limb replacement, fasciotomy, and revascularization.

William H. Harris, is an American orthopaedic surgeon, Founder and Director Emeritus of the Massachusetts General Hospital Harris Orthopaedics Laboratory, and creator of the Advances in Arthroplasty course held annually since 1970.

Reverse shoulder replacement is a type of shoulder replacement in which the normal ball and socket relationship of glenohumeral joint is reversed, creating a more stable joint with a fixed fulcrum. This form of shoulder replacement is utilized in situations in which conventional shoulder replacement surgery would lead to poor outcomes and high failure rates.
Justin Peter Cobb is a British professor of orthopaedic surgery at Imperial College London, known for introducing medical robotics into orthopaedic surgery. He is a member of the Royal Medical Household and was royal orthopaedic surgeon to the Queen. He is on the staff at King Edward VII's Hospital (KEVII) and is civilian advisor in orthopaedics to the Royal Air Force (RAF). His research has also included themes relating to designing new devices such as for ceramic hip resurfacing, 3D printing in orthopaedics, and training in surgical skills. He is a director of the MSk laboratory based in the Sir Michael Uren Hub.