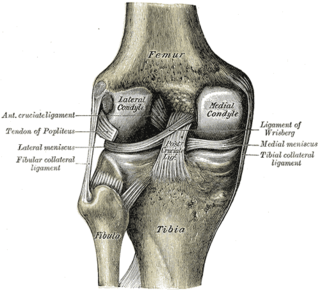
In humans and other primates, the knee joins the thigh with the leg and consists of two joints: one between the femur and tibia, and one between the femur and patella. It is the largest joint in the human body. The knee is a modified hinge joint, which permits flexion and extension as well as slight internal and external rotation. The knee is vulnerable to injury and to the development of osteoarthritis.

Orthopedic surgery or orthopedics is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors, and congenital disorders.
An osteotomy is a surgical operation whereby a bone is cut to shorten or lengthen it or to change its alignment. It is sometimes performed to correct a hallux valgus, or to straighten a bone that has healed crookedly following a fracture. It is also used to correct a coxa vara, genu valgum, and genu varum. The operation is done under a general anaesthetic.

Genu varum is a varus deformity marked by (outward) bowing at the knee, which means that the lower leg is angled inward (medially) in relation to the thigh's axis, giving the limb overall the appearance of an archer's bow. Usually medial angulation of both lower limb bones is involved.

Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant, that is, a hip prosthesis. Hip replacement surgery can be performed as a total replacement or a hemi/semi(half) replacement. Such joint replacement orthopaedic surgery is generally conducted to relieve arthritis pain or in some hip fractures. A total hip replacement consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is one of the most common orthopaedic operations, though patient satisfaction varies widely. Approximately 58% of total hip replacements are estimated to last 25 years. The average cost of a total hip replacement in 2012 was $40,364 in the United States, and about $7,700 to $12,000 in most European countries.
Arthroplasty is an orthopedic surgical procedure where the articular surface of a musculoskeletal joint is replaced, remodeled, or realigned by osteotomy or some other procedure. It is an elective procedure that is done to relieve pain and restore function to the joint after damage by arthritis or some other type of trauma.
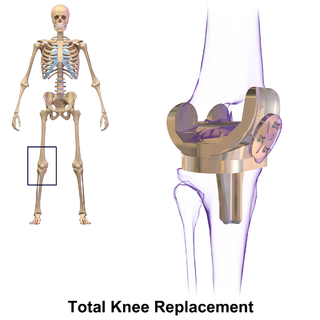
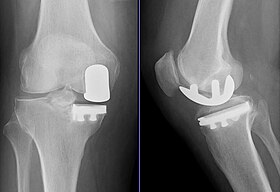
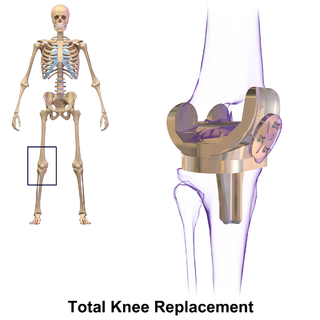
Knee replacement, also known as knee arthroplasty, is a surgical procedure to replace the weight-bearing surfaces of the knee joint to relieve pain and disability, most commonly offered when joint pain is not diminished by conservative sources. It may also be performed for other knee diseases, such as rheumatoid arthritis. In patients with severe deformity from advanced rheumatoid arthritis, trauma, or long-standing osteoarthritis, the surgery may be more complicated and carry higher risk. Osteoporosis does not typically cause knee pain, deformity, or inflammation, and is not a reason to perform knee replacement.

Joint replacement is a procedure of orthopedic surgery known also as arthroplasty, in which an arthritic or dysfunctional joint surface is replaced with an orthopedic prosthesis. Joint replacement is considered as a treatment when severe joint pain or dysfunction is not alleviated by less-invasive therapies. Joint replacement surgery is often indicated from various joint diseases, including osteoarthritis and rheumatoid arthritis.
A meniscus transplant or meniscal transplant is a transplant of the meniscus of the knee, which separates the thigh bone (femur) from the lower leg bone (tibia). The worn or damaged meniscus is removed and is replaced with a new one from a donor. The meniscus to be transplanted is taken from a cadaver, and, as such, is known as an allograft. Meniscal transplantation is technically difficult, as it must be sized accurately for each person, positioned properly and secured to the tibial plateau. As of 2012, only a few surgeons have significant volume of experience in meniscus transplantation worldwide.
Protrusio acetabuli is an uncommon defect of the acetabulum, the socket that receives the femoral head to make the hip joint. The hip bone of the pelvic bone/girdle is composed of three bones, the ilium, the ischium and the pubis. In protrusio deformity, there is medial displacement of the femoral head in that the medial aspect of the femoral cortex is medial to the ilioischial line. The socket is too deep and may protrude into the pelvis.

Hip resurfacing has been developed as a surgical alternative to total hip replacement (THR). The procedure consists of placing a cap, which is hollow and shaped like a mushroom, over the head of the femur while a matching metal cup is placed in the acetabulum, replacing the articulating surfaces of the person's hip joint and removing very little bone compared to a THR. When the person moves the hip, the movement of the joint induces synovial fluid to flow between the hard metal bearing surfaces lubricating them when the components are placed in the correct position. The surgeon's level of experience with hip resurfacing is most important; therefore, the selection of the right surgeon is crucial for a successful outcome. Health-related quality of life measures are markedly improved and the person's satisfaction is favorable after hip resurfacing arthroplasty.

A tear of a meniscus is a rupturing of one or more of the fibrocartilage strips in the knee called menisci. When doctors and patients refer to "torn cartilage" in the knee, they actually may be referring to an injury to a meniscus at the top of one of the tibiae. Menisci can be torn during innocuous activities such as walking or squatting. They can also be torn by traumatic force encountered in sports or other forms of physical exertion. The traumatic action is most often a twisting movement at the knee while the leg is bent. In older adults, the meniscus can be damaged following prolonged 'wear and tear'. Especially acute injuries can lead to displaced tears which can cause mechanical symptoms such as clicking, catching, or locking during motion of the joint. The joint will be in pain when in use, but when there is no load, the pain goes away.
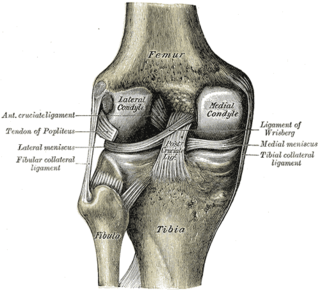
Spontaneous osteonecrosis of the knee is the result of vascular arterial insufficiency to the medial femoral condyle of the knee resulting in necrosis and destruction of bone. It is often unilateral and can be associated with a meniscal tear.
"Professor" Derek McMinn is a British orthopaedic surgeon and inventor who practised in Birmingham, United Kingdom at the BMI Edgbaston Hospital until his suspension in 2020. McMinn is currently under police investigation for allegedly keeping the body parts of thousands of patients over a 25-year period.

Medial knee injuries are the most common type of knee injury. The medial ligament complex of the knee consists of:

Trapeziometacarpal osteoarthritis (TMC OA) is, also known as osteoarthritis at the base of the thumb, thumb carpometacarpal osteoarthritis, basilar (or basal) joint arthritis, or as rhizarthrosis. This joint is formed by the trapezium bone of the wrist and the metacarpal bone of the thumb. This is one of the joints where most humans develop osteoarthritis with age. Osteoarthritis is age-related loss of the smooth surface of the bone where it moves against another bone (cartilage of the joint). In reaction to the loss of cartilage, the bones thicken at the joint surface, resulting in subchondral sclerosis. Also, bony outgrowths, called osteophytes (also known as “bone spurs”), are formed at the joint margins.
High tibial osteotomy is an orthopaedic surgical procedure which aims to correct a varus deformation with compartmental osteoarthritis. Since the inception of the procedure, advancements to technique, fixation devices, and a better understanding of patient selection has allowed HTO to become more popular in younger, more active patients hoping to combat arthritis. The idea behind the procedure is to realign the weight-bearing line of the knee. By realigning the knee, the force produced from weight-bearing is shifted from the arthritic, medial compartment to the healthy, lateral compartment. This decrease in force or load in the diseased part of the knee joint decreases knee pain and can delay the development or progression of osteoarthritis in the medial compartment.
The following outline is provided as an overview of and topical guide to trauma and orthopaedics:
Simitri Stable in Stride is a three part modular surgical implant used during surgery performed on dogs to stabilize the stifle joint (knee) after rupture of the cranial cruciate ligament (CrCL) which is analogous to the anterior cruciate ligament (ACL) in humans.
Justin Peter Cobb is a British professor of orthopaedic surgery at Imperial College London, known for introducing medical robotics into orthopaedic surgery. He is a member of the Royal Medical Household and was royal orthopaedic surgeon to the Queen. He is on the staff at King Edward VII's Hospital (KEVII) and is civilian advisor in orthopaedics to the Royal Air Force (RAF). His research has also included themes relating to designing new devices such as for ceramic hip resurfacing, 3D printing in orthopaedics, and training in surgical skills. He is a director of the MSk laboratory based in the Sir Michael Uren Hub.