Related Research Articles

Meconium aspiration syndrome (MAS) also known as neonatal aspiration of meconium is a medical condition affecting newborn infants. It describes the spectrum of disorders and pathophysiology of newborns born in meconium-stained amniotic fluid (MSAF) and have meconium within their lungs. Therefore, MAS has a wide range of severity depending on what conditions and complications develop after parturition. Furthermore, the pathophysiology of MAS is multifactorial and extremely complex which is why it is the leading cause of morbidity and mortality in term infants.

Pneumonia is an inflammatory condition of the lung primarily affecting the small air sacs known as alveoli. Symptoms typically include some combination of productive or dry cough, chest pain, fever, and difficulty breathing. The severity of the condition is variable.

Pulmonology, pneumology or pneumonology is a medical specialty that deals with diseases involving the respiratory tract. It is also known as respirology, respiratory medicine, or chest medicine in some countries and areas.

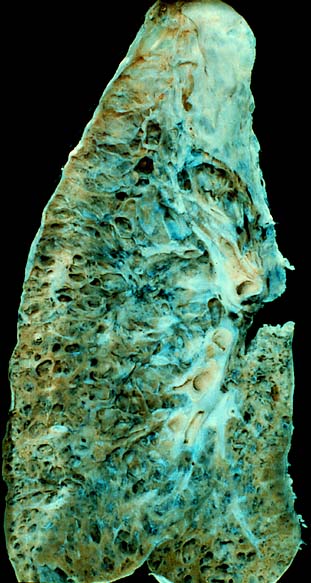
Pulmonary alveolar proteinosis (PAP) is a rare lung disorder characterized by an abnormal accumulation of surfactant-derived lipoprotein compounds within the alveoli of the lung. The accumulated substances interfere with the normal gas exchange and expansion of the lungs, ultimately leading to difficulty breathing and a predisposition to developing lung infections. The causes of PAP may be grouped into primary, secondary, and congenital causes, although the most common cause is a primary autoimmune condition in an individual.
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris, aspiration, herbicides or fluorocarbons and some systemic diseases. If unresolved, continued inflammation can result in irreparable damage such as pulmonary fibrosis.
Eosinophilic pneumonia is a disease in which an eosinophil, a type of white blood cell, accumulates in the lungs. These cells cause disruption of the normal air spaces (alveoli) where oxygen is extracted from the atmosphere. Several different kinds of eosinophilic pneumonia exist and can occur in any age group. The most common symptoms include cough, fever, difficulty breathing, and sweating at night. Eosinophilic pneumonia is diagnosed by a combination of characteristic symptoms, findings on a physical examination by a health provider, and the results of blood tests and X-rays. Prognosis is excellent once most eosinophilic pneumonia is recognized and treatment with corticosteroids is begun.

Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles (bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pneumonia.
Ventilator-associated pneumonia (VAP) is a type of lung infection that occurs in people who are on mechanical ventilation breathing machines in hospitals. As such, VAP typically affects critically ill persons that are in an intensive care unit (ICU) and have been on a mechanical ventilator for at least 48 hours. VAP is a major source of increased illness and death. Persons with VAP have increased lengths of ICU hospitalization and have up to a 20–30% death rate. The diagnosis of VAP varies among hospitals and providers but usually requires a new infiltrate on chest x-ray plus two or more other factors. These factors include temperatures of >38 °C or <36 °C, a white blood cell count of >12 × 109/ml, purulent secretions from the airways in the lung, and/or reduction in gas exchange.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.

A sputum culture is a test to detect and identify bacteria or fungi that infect the lungs or breathing passages. Sputum is a thick fluid produced in the lungs and in the adjacent airways. Normally, fresh morning sample is preferred for the bacteriological examination of sputum. A sample of sputum is collected in a sterile, wide-mouthed, dry, leak-proof and break-resistant plastic-container and sent to the laboratory for testing. Sampling may be performed by sputum being expectorated, induced, or taken via an endotracheal tube with a protected specimen brush in an intensive care setting. For selected organisms such as Cytomegalovirus or "Pneumocystis jiroveci" in specific clinical settings a bronchoalveolar lavage might be taken by an experienced pneumologist. If no bacteria or fungi grow, the culture is negative. If organisms that can cause the infection grow, the culture is positive. The type of bacterium or fungus is identified by microscopy, colony morphology and biochemical tests of bacterial growth.

Alveolar lung diseases, are a group of diseases that mainly affect the alveoli of the lungs.
Exercise-induced pulmonary hemorrhage (EIPH), also known as "bleeding" or a "bleeding attack", refers to the presence of blood in the airways of the lung in association with exercise. EIPH is common in horses undertaking intense exercise, but it has also been reported in human athletes, racing camels and racing greyhounds. Horses that experience EIPH may also be referred to as "bleeders" or as having "broken a blood vessel". In the majority of cases, EIPH is not apparent unless an endoscopic examination of the airways is performed following exercise. This is distinguished from other forms of bleeding from the nostrils, called epistaxis.

Bronchoscopy is an endoscopic technique of visualizing the inside of the airways for diagnostic and therapeutic purposes. An instrument (bronchoscope) is inserted into the airways, usually through the nose or mouth, or occasionally through a tracheostomy. This allows the practitioner to examine the patient's airways for abnormalities such as foreign bodies, bleeding, tumors, or inflammation. Specimens may be taken from inside the lungs. The construction of bronchoscopes ranges from rigid metal tubes with attached lighting devices to flexible optical fiber instruments with realtime video equipment.
Pulmonary hygiene, also referred to as pulmonary toilet, is a set of methods used to clear mucus and secretions from the airways. The word pulmonary refers to the lungs. The word toilet, related to the French toilette, refers to body care and hygiene; this root is used in words such as toiletry that also relate to cleansing.
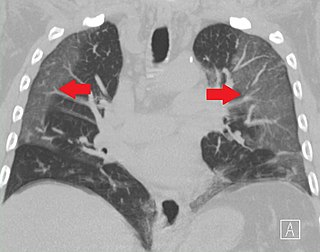
Ground-glass opacity (GGO) is a finding seen on chest x-ray (radiograph) or computed tomography (CT) imaging of the lungs. It is typically defined as an area of hazy opacification (x-ray) or increased attenuation (CT) due to air displacement by fluid, airway collapse, fibrosis, or a neoplastic process. When a substance other than air fills an area of the lung it increases that area's density. On both x-ray and CT, this appears more grey or hazy as opposed to the normally dark-appearing lungs. Although it can sometimes be seen in normal lungs, common pathologic causes include infections, interstitial lung disease, and pulmonary edema.
Indium lung is a rare occupational lung disease caused by exposure to respirable indium in the form of indium tin oxide. It is classified as an interstitial lung disease.

Lipid-laden alveolar macrophages, also known as pulmonary foam cells, are cells found in bronchoalveolar lavage (BAL) specimens that consist of macrophages containing deposits of lipids (fats). The lipid content of the macrophages can be demonstrated using a lipid targeting stain like Oil Red O or Nile red. Increased levels of lipid-laden alveolar macrophages are associated with various respiratory conditions, including chronic smoking, gastroesophageal reflux, lipoid pneumonia, fat embolism, pulmonary alveolar proteinosis and pulmonary aspiration. Lipid-laden alveolar macrophages have been reported in cases of vaping-associated pulmonary injury.
Vaping-associated pulmonary injury (VAPI), also known as vaping-associated lung injury (VALI) or e-cigarette, or vaping, product use associated lung injury (E/VALI), is an umbrella term, used to describe lung diseases associated with the use of vaping products that can be severe and life-threatening. Symptoms can initially mimic common pulmonary diagnoses, such as pneumonia, but sufferers typically do not respond to antibiotic therapy. Differential diagnoses have overlapping features with VAPI, including COVID-19. According to a systematic review article, "Initial case reports of vaping-related lung injury date back to 2012, but the ongoing outbreak of EVALI began in the summer of 2019." According to an article in the Radiological Society of North America news published in March 2022, EVALI cases continue to be diagnosed. “EVALI has by no means disappeared,” Dr. Kligerman said. “We continue to see numerous cases, even during the pandemic, many of which are initially misdiagnosed as COVID-19.”
Whole lung lavage (WLL), also called lung washing, is a medical procedure in which the patient's lungs are washed with saline by filling and draining repeatedly. It is used to treat pulmonary alveolar proteinosis, in which excess lung surfactant proteins prevent the patient from breathing. Some sources consider it a variation of bronchoalveolar lavage.
References
- ↑ Kahn, F.W.; Jones, J.M. (1987). "Diagnosing bacterial respiratory infection by bronchoalveolar lavage". Journal of Infectious Diseases. 155 (5): 826–9. doi:10.1093/infdis/155.5.862. PMID 3559290.
- ↑ Sugeir, S.; de Moraes, A.G. (2019). "6. Bronchoscopy in the Intensive Care Unit". In Demetriades, D.; Inaba, K. (eds.). Atlas of Critical Care Procedures. Springer. p. 50. ISBN 9783319783673.
- 1 2 3 4 5 Warriner, Z.; Lewis, M. (2019). "7. Bronchoalveolar Lavage". In Demetriades, D.; Inaba, K. (eds.). Atlas of Critical Care Procedures. Springer. pp. 57–62. ISBN 9783319783673.
- ↑ Nieto, J.M.S.; Alcaraz, A.C. (1995). "The role of bronchoalveolar lavage in the diagnosis of bacterial pneumonia". European Journal of Clinical Microbiology and Infectious Diseases. 14 (10): 839–50. doi:10.1007/BF01691489. PMC 7102128 . PMID 8605896.
- 1 2 Jonker, M.A.; Sauerhammer, T.M.; Faucher, L.D.; et al. (2012). "Bilateral versus unilateral bronchoalveolar lavage for the diagnosis of ventilator-associated pneumonia". Surgical Infections. 13 (6): 391–5. doi:10.1089/sur.2011.081. PMC 3532003 . PMID 23240724.
- 1 2 Yang, X.J.; Wang, Y.B.; Zhou, Z.W.; et al. (2015). "High-throughput sequencing of 16S rDNA amplicons characterizes bacterial composition in bronchoalveolar lavage fluid in patients with ventilator-associated pneumonia". Drug Design, Development and Therapy. 9: 4883–96. doi: 10.2147/DDDT.S87634 . PMC 4554422 . PMID 26345636.
- ↑ World Health Organization (19 March 2020). "Laboratory testing for coronavirus disease (COVID-19) in suspected human cases: Interim guidance, 19 March 2020". WHO/COVID-19/Laboratory/2020.5. World Health Organization. hdl:10665/331501 . Retrieved 25 March 2020.
- ↑ Centers for Disease Control and Prevention (25 March 2020). "Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Persons for Coronavirus Disease 2019 (COVID-19)". Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. Retrieved 25 March 2020.
- ↑ Meyer, K.C.; Raghu, G.; Baughman, R.P.; et al. (2012). "An official American Thoracic Society clinical practice guideline: The clinical utility of bronchoalveolar lavage cellular analysis in interstitial lung disease" (PDF). American Journal of Respiratory and Critical Care Medicine. 185 (9): 1004–14. doi:10.1164/rccm.201202-0320ST. PMID 22550210.
- ↑ Ramos KJ, Kapnadak SG, Collins BF, Wall R, Bryson-Cahn C, Perchetti GA, Jerome KR, Khot S, Limaye AP, Mathias PC, Greninger AL (2020). "Detection of SARS-CoV-2 by bronchoalveolar lavage after negative nasopharyngeal testing: Stay vigilant for COVID-19". Respiratory Medicine Case Reports. 30: 101120. doi: 10.1016/j.rmcr.2020.101120 . PMC 7298516 . PMID 32566476.
- 1 2 Rodrigo, D.; Rathnapala, A.; Senaratne, W. (2015). "Therapeutic limited bronchoalveolar lavage with fiberoptic bronchoscopy as a bridging procedure prior to total lung lavage in a patient with pulmonary alveolar proteinosis: A case report". Journal of Medical Case Reports. 9. 93. doi: 10.1186/s13256-015-0574-z . PMC 4421915 . PMID 25925248.
- ↑ Henderson, A.J. (1994). "Bronchoalveolar lavage". Archives of Disease in Childhood. 70 (3): 167–9. doi:10.1136/adc.70.3.167. PMC 1029733 . PMID 8135556.
- 1 2 Wang, Y.; Wang, H.; Zhang, C.; et al. (2019). "Lung fluid biomarkers for acute respiratory distress syndrome: A systematic review and meta-analysis". Critical Care. 23 (1). 43. doi: 10.1186/s13054-019-2336-6 . PMC 6373030 . PMID 30755248.
- 1 2 Zhao, H.; Gu, H.; Liu, T.; Ge, J.; Shi, G. (2018). "Analysis of curative effect of adjuvant therapy with bronchoalveolar lavage on COPD patients complicated with pneumonia". Experimental and Therapeutic Medicine. 16 (5): 3799–3804. doi:10.3892/etm.2018.6662. PMC 6176127 . PMID 30344655.
- ↑ Wu, X; Lu, W; Wang, T; Xiao, A; Guo, X; Xu, Y; Li, S; Liu, X; Zeng, H; He, S; Zhang, X (5 October 2023). "Optimization strategy for the early timing of bronchoalveolar lavage treatment for children with severe mycoplasma pneumoniae pneumonia". BMC Infectious Diseases. 23 (1): 661. doi: 10.1186/s12879-023-08619-9 . PMC 10557288 . PMID 37798699.
- ↑ Michaud, G.; Reddy, C.; Ernst, A. (2009). "Whole-lung lavage for pulmonary alveolar proteinosis". Chest. 136 (6): 1678–1681. doi:10.1378/chest.09-2295. PMID 19995769.
- ↑ Cleveland Clinic (6 August 2014). "How 'Lung Washing' Helps You Breathe Again". HealthEssentials. Archived from the original on 14 August 2020. Retrieved 25 March 2020.
- ↑ Danel, C.; Israël-Biet, D.; Costabel, U.; Klech, H. (1992). "Therapeutic applications of bronchoalveolar lavage". European Respiratory Journal. 5 (10): 1173–5. doi: 10.1183/09031936.93.05101173 . PMID 1486961. S2CID 6265382.
- ↑ Wang, Lijun; Xie, Qiuling; Xu, Shanshan; Li, Huajun; Zhang, Liya; Ai, Jingwen; Liu, Quanhua; Chu, Caiting; Zhang, Xi; Zhang, Wenhong; Huang, Lisu (January 2023). "The role of flexible bronchoscopy in children with Mycoplasma pneumoniae pneumonia". Pediatric Research. 93 (1): 198–206. doi:10.1038/s41390-021-01874-z. PMID 35459766. S2CID 248326894.