Related Research Articles

Respiratory failure results from inadequate gas exchange by the respiratory system, meaning that the arterial oxygen, carbon dioxide, or both cannot be kept at normal levels. A drop in the oxygen carried in the blood is known as hypoxemia; a rise in arterial carbon dioxide levels is called hypercapnia. Respiratory failure is classified as either Type 1 or Type 2, based on whether there is a high carbon dioxide level, and can be acute or chronic. In clinical trials, the definition of respiratory failure usually includes increased respiratory rate, abnormal blood gases, and evidence of increased work of breathing. Respiratory failure causes an altered mental status due to ischemia in the brain.

A cough is a sudden expulsion of air through the large breathing passages which can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three phases: an inhalation, a forced exhalation against a closed glottis, and a violent release of air from the lungs following opening of the glottis, usually accompanied by a distinctive sound.

Eosinophilia is a condition in which the eosinophil count in the peripheral blood exceeds 5×108/L (500/μL). Hypereosinophilia is an elevation in an individual's circulating blood eosinophil count above 1.5 × 109/L (i.e. 1,500/μL). The hypereosinophilic syndrome is a sustained elevation in this count above 1.5 × 109/L (i.e. 1,500/μL) that is also associated with evidence of eosinophil-based tissue injury.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.

Vasculitis is a group of disorders that destroy blood vessels by inflammation. Both arteries and veins are affected. Lymphangitis is sometimes considered a type of vasculitis. Vasculitis is primarily caused by leukocyte migration and resultant damage. Although both occur in vasculitis, inflammation of veins (phlebitis) or arteries (arteritis) on their own are separate entities.

Pulmonary alveolar proteinosis (PAP) is a rare lung disorder characterized by an abnormal accumulation of surfactant-derived lipoprotein compounds within the alveoli of the lung. The accumulated substances interfere with the normal gas exchange and expansion of the lungs, ultimately leading to difficulty breathing and a predisposition to developing lung infections. The causes of PAP may be grouped into primary, secondary, and congenital causes, although the most common cause is a primary autoimmune condition in an individual.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Hypersensitivity pneumonitis (HP) or extrinsic allergic alveolitis (EAA) is a syndrome caused by the repetitive inhalation of antigens from the environment in susceptible or sensitized people. Common antigens include molds, bacteria, bird droppings, bird feathers, agricultural dusts, bioaerosols and chemicals from paints or plastics. People affected by this type of lung inflammation (pneumonitis) are commonly exposed to the antigens by their occupations, hobbies, the environment and animals. The inhaled antigens produce a hypersensitivity immune reaction causing inflammation of the airspaces (alveoli) and small airways (bronchioles) within the lung. Hypersensitivity pneumonitis may eventually lead to interstitial lung disease.

Pneumonitis describes general inflammation of lung tissue. Possible causative agents include radiation therapy of the chest, exposure to medications used during chemo-therapy, the inhalation of debris, aspiration, herbicides or fluorocarbons and some systemic diseases. If unresolved, continued inflammation can result in irreparable damage such as pulmonary fibrosis.
Eosinophilic pneumonia is a disease in which an eosinophil, a type of white blood cell, accumulates in the lungs. These cells cause disruption of the normal air spaces (alveoli) where oxygen is extracted from the atmosphere. Several different kinds of eosinophilic pneumonia exist and can occur in any age group. The most common symptoms include cough, fever, difficulty breathing, and sweating at night. Eosinophilic pneumonia is diagnosed by a combination of characteristic symptoms, findings on a physical examination by a health provider, and the results of blood tests and X-rays. Prognosis is excellent once most eosinophilic pneumonia is recognized and treatment with corticosteroids is begun.

Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles (bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pneumonia.

Löffler's syndrome is a disease in which eosinophils accumulate in the lung in response to a parasitic infection. The parasite can be Ascaris, Strongyloides stercoralis, or Dirofilaria immitis which can enter the body through contact with the soil. The symptoms of Löffler's syndrome include those of a parasitic infection such as abdominal pain and cramping, skin rashes and fatigue. Löffler's syndrome itself will cause difficulty breathing, wheeze, coughing as well as a fever.

Acute interstitial pneumonitis (also known as acute interstitial pneumoniais a rare, severe lung disease that usually affects otherwise healthy individuals. There is no known cause or cure.
Loeffler endocarditis is a form of heart disease characterized by a stiffened, poorly-functioning heart caused by infiltration of the heart by white blood cells known as eosinophils. Restrictive cardiomyopathy is a disease of the heart muscle which results in impaired diastolic filling of the heart ventricles, i.e. the large heart chambers which pump blood into the pulmonary or systemic circulation. Diastole is the part of the cardiac contraction-relaxation cycle in which the heart fills with venous blood after the emptying done during its previous systole.
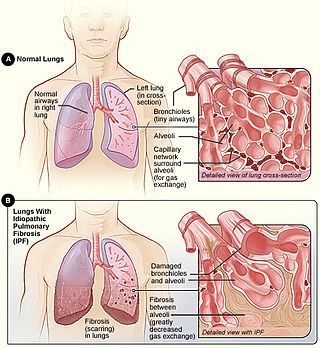
Idiopathic pulmonary fibrosis (IPF), or (formerly) fibrosing alveolitis, is a rare, progressive illness of the respiratory system, characterized by the thickening and stiffening of lung tissue, associated with the formation of scar tissue. It is a type of chronic scarring lung disease characterized by a progressive and irreversible decline in lung function. The tissue in the lungs becomes thick and stiff, which affects the tissue that surrounds the air sacs in the lungs. Symptoms typically include gradual onset of shortness of breath and a dry cough. Other changes may include feeling tired, and abnormally large and dome shaped finger and toenails. Complications may include pulmonary hypertension, heart failure, pneumonia or pulmonary embolism.
Chalicosis is a form of pneumoconiosis affecting the lungs or bronchioles, found mainly among stonecutters. The disease is caused by the inhalation of fine particles of stone. The term is from Greek, χάλιξ, gravel.
Tropical pulmonary eosinophilia, is characterized by cough, bronchospasm, wheezing, abdominal pain, and an enlarged spleen. Occurring most frequently in the Indian subcontinent and Southeast Asia, TPE is a clinical manifestation of lymphatic filariasis, a parasitic infection caused by filarial roundworms that inhabit the lymphatic vessels, lymph nodes, spleen, and bloodstream. Three species of filarial roundworms, all from the Onchocercidae family, cause human lymphatic filariasis: Wuchereria bancrofti, Brugia malayi, and Brugia timori.
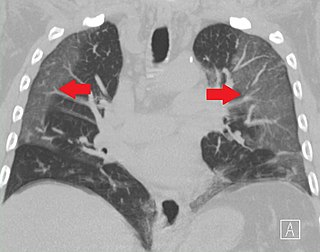
Ground-glass opacity (GGO) is a finding seen on chest x-ray (radiograph) or computed tomography (CT) imaging of the lungs. It is typically defined as an area of hazy opacification (x-ray) or increased attenuation (CT) due to air displacement by fluid, airway collapse, fibrosis, or a neoplastic process. When a substance other than air fills an area of the lung it increases that area's density. On both x-ray and CT, this appears more grey or hazy as opposed to the normally dark-appearing lungs. Although it can sometimes be seen in normal lungs, common pathologic causes include infections, interstitial lung disease, and pulmonary edema.
Eosinophilic myocarditis is inflammation in the heart muscle that is caused by the infiltration and destructive activity of a type of white blood cell, the eosinophil. Typically, the disorder is associated with hypereosinophilia, i.e. an eosinophil blood cell count greater than 1,500 per microliter. It is distinguished from non-eosinophilic myocarditis, which is heart inflammation caused by other types of white blood cells, i.e. lymphocytes and monocytes, as well as the respective descendants of these cells, NK cells and macrophages. This distinction is important because the eosinophil-based disorder is due to a particular set of underlying diseases and its preferred treatments differ from those for non-eosinophilic myocarditis.
Vaping-associated pulmonary injury (VAPI), also known as vaping-associated lung injury (VALI) or e-cigarette, or vaping, product use associated lung injury (E/VALI), is an umbrella term, used to describe lung diseases associated with the use of vaping products that can be severe and life-threatening. Symptoms can initially mimic common pulmonary diagnoses, such as pneumonia, but sufferers typically do not respond to antibiotic therapy. Differential diagnoses have overlapping features with VAPI, including COVID-19. According to a systematic review article, "Initial case reports of vaping-related lung injury date back to 2012, but the ongoing outbreak of EVALI began in the summer of 2019." According to an article in the Radiological Society of North America news published in March 2022, EVALI cases continue to be diagnosed. “EVALI has by no means disappeared,” Dr. Kligerman said. “We continue to see numerous cases, even during the pandemic, many of which are initially misdiagnosed as COVID-19.”
References
- 1 2 3 4 5 6 7 8 De Giacomi, Federica; Vassallo, Robert; Yi, Eunhee S.; Ryu, Jay H. (2018-03-15). "Acute Eosinophilic Pneumonia. Causes, Diagnosis, and Management". American Journal of Respiratory and Critical Care Medicine. 197 (6): 728–736. doi:10.1164/rccm.201710-1967CI. ISSN 1073-449X.
- ↑ Allen, James (April 2006). "Acute Eosinophilic Pneumonia". Seminars in Respiratory and Critical Care Medicine. 27 (2): 142–147. doi:10.1055/s-2006-939517. ISSN 1069-3424.
- 1 2 Cottin, Vincent (May 2023). "Eosinophilic Lung Diseases". Immunology and Allergy Clinics of North America. 43 (2): 289–322. doi:10.1016/j.iac.2023.01.002.
- 1 2 Suzuki, Yuzo; Suda, Takafumi (October 2019). "Eosinophilic pneumonia: A review of the previous literature, causes, diagnosis, and management". Allergology International: Official Journal of the Japanese Society of Allergology. 68 (4): 413–419. doi:10.1016/j.alit.2019.05.006. ISSN 1440-1592. PMID 31253537.