Related Research Articles

Charcot–Marie–Tooth disease (CMT) is a hereditary motor and sensory neuropathy of the peripheral nervous system characterized by progressive loss of muscle tissue and touch sensation across various parts of the body. This disease is the most commonly inherited neurological disorder, affecting about one in 2,500 people. It is named after those who classically described it: the Frenchman Jean-Martin Charcot (1825–1893), his pupil Pierre Marie (1853–1940), and the Briton Howard Henry Tooth (1856–1925).

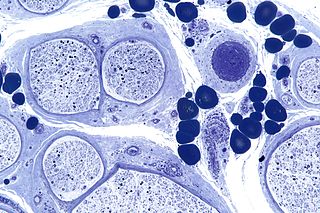
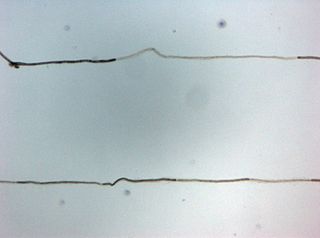
In vertebrates, most neuronal cell axons are encased in myelin. Simply put, myelin insulates axons and increases the rate at which electrical impulses are passed along the axon. The myelinated axon can be likened to an electrical wire with insulating material (myelin) around it. However, unlike the plastic covering on an electrical wire, myelin does not form a single long sheath over the entire length of the axon. Rather, myelin ensheaths the axon in segments: in general, each axon is encased in multiple long myelin sheaths separated by short gaps called nodes of Ranvier.
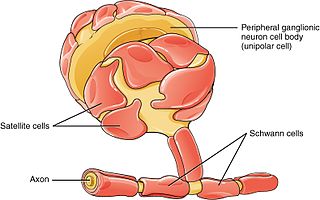
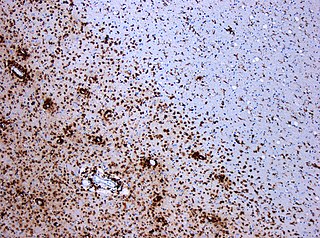
Schwann cells or neurolemmocytes are the principal glia of the peripheral nervous system (PNS). Glial cells function to support neurons and in the PNS, also include satellite cells, olfactory ensheathing cells, enteric glia and glia that reside at sensory nerve endings, such as the Pacinian corpuscle. The two types of Schwann cells are myelinating and nonmyelinating. Myelinating Schwann cells wrap around axons of motor and sensory neurons to form the myelin sheath. The Schwann cell promoter is present in the downstream region of the human dystrophin gene that gives shortened transcript that are again synthesized in a tissue-specific manner.
Peripheral neuropathy, often shortened to neuropathy, is a general term describing damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathy affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.
A demyelinating disease refers to any disease affecting the nervous system where the myelin sheath surrounding neurons is damaged. This damage disrupts the transmission of signals through the affected nerves, resulting in a decrease in their conduction ability. Consequently, this reduction in conduction can lead to deficiencies in sensation, movement, cognition, or other functions depending on the nerves affected.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.

Neuritis is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
Sulfatide, also known as 3-O-sulfogalactosylceramide, SM4, or sulfated galactocerebroside, is a class of sulfolipids, specifically a class of sulfoglycolipids, which are glycolipids that contain a sulfate group. Sulfatide is synthesized primarily starting in the endoplasmic reticulum and ending in the Golgi apparatus where ceramide is converted to galactocerebroside and later sulfated to make sulfatide. Of all of the galactolipids that are found in the myelin sheath, one fifth of them are sulfatide. Sulfatide is primarily found on the extracellular leaflet of the myelin plasma membrane produced by the oligodendrocytes in the central nervous system and in the Schwann cells in the peripheral nervous system. However, sulfatide is also present on the extracellular leaflet of the plasma membrane of many cells in eukaryotic organisms.

Myelin-associated glycoprotein is a type 1 transmembrane protein glycoprotein localized in periaxonal Schwann cell and oligodendrocyte membranes, where it plays a role in glial-axonal interactions. MAG is a member of the SIGLEC family of proteins and is a functional ligand of the NOGO-66 receptor, NgR. MAG is believed to be involved in myelination during nerve regeneration in the PNS and is vital for the long-term survival of the myelinated axons following myelinogenesis. In the CNS MAG is one of three main myelin-associated inhibitors of axonal regeneration after injury, making it an important protein for future research on neurogenesis in the CNS.

Nerve injury is an injury to nervous tissue. There is no single classification system that can describe all the many variations of nerve injuries. In 1941, Seddon introduced a classification of nerve injuries based on three main types of nerve fiber injury and whether there is continuity of the nerve. Usually, however, peripheral nerve injuries are classified in five stages, based on the extent of damage to both the nerve and the surrounding connective tissue, since supporting glial cells may be involved.
Neuroregeneration involves the regrowth or repair of nervous tissues, cells or cell products. Neuroregenerative mechanisms may include generation of new neurons, glia, axons, myelin, or synapses. Neuroregeneration differs between the peripheral nervous system (PNS) and the central nervous system (CNS) by the functional mechanisms involved, especially in the extent and speed of repair. When an axon is damaged, the distal segment undergoes Wallerian degeneration, losing its myelin sheath. The proximal segment can either die by apoptosis or undergo the chromatolytic reaction, which is an attempt at repair. In the CNS, synaptic stripping occurs as glial foot processes invade the dead synapse.

Myelin protein zero is a single membrane glycoprotein which in humans is encoded by the MPZ gene. P0 is a major structural component of the myelin sheath in the peripheral nervous system (PNS). Myelin protein zero is expressed by Schwann cells and accounts for over 50% of all proteins in the peripheral nervous system, making it the most common protein expressed in the PNS. Mutations in myelin protein zero can cause myelin deficiency and are associated with neuropathies like Charcot–Marie–Tooth disease and Dejerine–Sottas disease.
Nerve tissue is a biological molecule related to the function and maintenance of normal nervous tissue. An example would include, for example, the generation of myelin which insulates and protects nerves. These are typically calcium-binding proteins.
Guillain–Barré syndrome (GBS) is a rapid-onset muscle weakness caused by the immune system damaging the peripheral nervous system. Typically, both sides of the body are involved, and the initial symptoms are changes in sensation or pain often in the back along with muscle weakness, beginning in the feet and hands, often spreading to the arms and upper body. The symptoms may develop over hours to a few weeks. During the acute phase, the disorder can be life-threatening, with about 15% of people developing weakness of the breathing muscles and, therefore, requiring mechanical ventilation. Some are affected by changes in the function of the autonomic nervous system, which can lead to dangerous abnormalities in heart rate and blood pressure.
Antiganglioside antibodies that react to self-gangliosides are found in autoimmune neuropathies. These antibodies were first found to react with cerebellar cells. These antibodies show highest association with certain forms of Guillain–Barré syndrome.

Gap junction beta-1 protein (GJB1), also known as connexin 32 (Cx32), is a transmembrane protein that in humans is encoded by the GJB1 gene. Gap junction beta-1 protein is a member of the gap junction connexin family of proteins that regulates and controls the transfer of communication signals across cell membranes, primarily in the liver and peripheral nervous system. However, the protein is expressed in multiple organs, including in oligodendrocytes in the central nervous system.
Progressive inflammatory neuropathy is a disease that was identified in a report, released on January 31, 2008, by the Centers for Disease Control and Prevention. The first known outbreak of this neuropathy occurred in southeastern Minnesota in the United States. The disease was reported among pig slaughterhouse workers who appeared at various care facilities in the area reporting similar neurological symptoms. The disease was later identified at pork processing plants in Indiana and Nebraska as well. The condition is characterized by acute paralysis, pain, fatigue, numbness, and weakness, especially in extremities. It was initially believed that workers might have contracted the disease through inhaling aerosols from pig brains blown through a compressed-air hose and that this exposure to pig neural tissue induced an autoimmune response that might have produced their mysterious peripheral neuropathy. These suspicions were confirmed in reports and investigations conducted at the Mayo Clinic in Rochester, Minnesota.
Peripheral mononeuropathy is a nerve related disease where a single nerve, that is used to transport messages from the brain to the peripheral body, is diseased or damaged. Peripheral neuropathy is a general term that indicates any disorder of the peripheral nervous system. The name of the disorder itself can be broken down in order to understand this better; peripheral: in regard to peripheral neuropathy, refers to outside of the brain and spinal cord; neuro: means nerve related; -pathy; means disease. Peripheral mononeuropathy is a disorder that links to Peripheral Neuropathy, as it only effects a single peripheral nerve rather than several damaged or diseased nerves throughout the body. Healthy peripheral nerves are able to “carry messages from the brain and spinal cord to muscles, organs, and other body tissues”.
References
- 1 2 3 4 5 6 7 8 9 10 Dalakas, M. C. (2010). "Pathogenesis and Treatment of Anti-MAG Neuropathy". Current Treatment Options in Neurology. 12 (2): 71–83. doi:10.1007/s11940-010-0065-x. PMID 20842571. S2CID 22100604.
- ↑ Launay, M.; Delmont, E.; Benaim, C.; Sacconi, S.; Butori, C.; Desnuelle, C. (2009). "Anti-MAG paraproteinemic demyelinating polyneuropathy: A clinical, biological, electrophysiological and anatomopathological descriptive study of a 13-patients' cohort". Revue Neurologique. 165 (12): 1071–1079. doi:10.1016/j.neurol.2009.04.008. PMID 19487003.
- ↑ Gajos, A.; Kielis, W.; Szadkowska, I.; Chmielowska, E.; Niewodniczy, A.; Bogucki, A. (2007). "Acquired peripheral neuropathies associated with monoclonal gammopathy". Neurologia I Neurochirurgia Polska. 41 (2): 169–175. PMID 17530580.
- 1 2 Neuroscience. (2008). Sunderland (Mass.): Sinauer.
- 1 2 3 4 Quarles, R. H. (2007). "Myelin-associated glycoprotein (MAG): past, present and beyond". Journal of Neurochemistry. 100 (6): 1431–1448. doi:10.1111/j.1471-4159.2006.04319.x. PMID 17241126. S2CID 1544418.
- ↑ Garces-Sanchez, M.; Dyck, P. J.; Kyle, R. A.; Zeldenrust, S.; Wu, Y.; Ladha, S. S.; et al. (2008). "Antibodies to myelin-associated glycoprotein (anti-MAG) in IgM amyloidosis may influence expression of neuropathy in rare patients". Muscle & Nerve. 37 (4): 490–495. doi:10.1002/mus.20955. PMID 18236455. S2CID 606665.
- ↑ Kawagashira, Y.; Kondo, N.; Atsuta, N.; Iijima, M.; Koike, H.; Katsuno, M.; et al. (2010). "IgM MGUS Anti-MAG Neuropathy With Predominant Muscle Weakness and Extensive Muscle Atrophy". Muscle & Nerve. 42 (3): 433–435. doi:10.1002/mus.21741. PMID 20665518. S2CID 8611510.
- ↑ Kuijf, M. L.; Eurelings, M.; Tio-Gillen, A. P.; van Doorn, P. A.; den Berg, L. H.; Hooijkaas, H.; et al. (2009). "Detection of anti-MAG antibodies in polyneuropathy associated with IgM monoclonal gammopathy". Neurology. 73 (9): 688–695. doi:10.1212/wnl.0b013e3181b59a80. PMID 19720975. S2CID 22996467.
- ↑ Leger, J. M., Chassande, B., Bombelli, F., Viala, K., Musset, L., & Neil, J. (2009). Polyneuropathy associated with monoclonal gammapathy: treatment perspectives. Bulletin De L Academie Nationale De Médecine, 193(5), 1099-1110.
- ↑ Benedetti, L.; Briani, C.; Franciotta, D.; Carpo, M.; Padua, L.; Zara, G.; et al. (2008). "Long-Term Effect of Rituximab in Anti-MAG Polyneuropathy. [Editorial Material]". Neurology. 71 (21): 1742–1744. doi:10.1212/01.wnl.0000335268.70325.33. PMID 19015493. S2CID 28723175.
- ↑ Broglio, L.; Lauria, G. (2005). "Worsening after rituximab treatment in anti-MAG neuropathy. [Letter]". Muscle & Nerve. 32 (3): 378–379. doi:10.1002/mus.20386. PMID 15986418. S2CID 30592290.
- ↑ Léger, JM; Viala, K; Nicolas, G; Créange, A; Vallat, JM; Pouget, J; Clavelou, P; Vial, C; Steck, A; Musset, L; Marin, B (2013). "Placebo-controlled trial of rituximab in IgM anti-myelin-associated glycoprotein neuropathy". Neurology. 80 (24): 2217–25. doi:10.1212/WNL.0b013e318296e92b. PMC 3721095 . PMID 23667063.
- ↑ Lunn, M (2008). "What's new in paraproteinemic demyelinating neuropathy in 2007-2008?". Journal of the Peripheral Nervous System. 13 (4): 264–266. doi:10.1111/j.1529-8027.2008.00191.x. PMID 19192065. S2CID 34972889.