Related Research Articles

Nasogastric intubation is a medical process involving the insertion of a plastic tube through the nose, down the oesophagus, and down into the stomach. Orogastric intubation is a similar process involving the insertion of a plastic tube through the mouth. Abraham Louis Levin invented the NG tube. Nasogastric tube is also known as Ryle's tube in Commonwealth countries, after John Alfred Ryle.

A feeding tube is a medical device used to provide nutrition to people who cannot obtain nutrition by mouth, are unable to swallow safely, or need nutritional supplementation. The state of being fed by a feeding tube is called gavage, enteral feeding or tube feeding. Placement may be temporary for the treatment of acute conditions or lifelong in the case of chronic disabilities. A variety of feeding tubes are used in medical practice. They are usually made of polyurethane or silicone. The diameter of a feeding tube is measured in French units. They are classified by the site of insertion and intended use.
Gastric bypass surgery refers to a technique in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass procedures (GBP). Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.

Vertical banded gastroplasty (VBG), also known as stomach stapling, is a form of bariatric surgery for weight control. The VBG procedure involves using a band and staples to create a small stomach pouch. In the bottom of the pouch is an approximate one-centimeter hole through which the pouch contents can flow into the remainder of the stomach and hence on to the remainder of the gastrointestinal tract.
The duodenal switch (DS) procedure, gastric reduction duodenal switch (GRDS), is a weight loss surgery procedure that is composed of a restrictive and a malabsorptive aspect.

A laparoscopic adjustable gastric band, commonly called a lap-band, A band, or LAGB, is an inflatable silicone device placed around the top portion of the stomach to treat obesity, intended to decrease food consumption.
Sleeve gastrectomy or vertical sleeve gastrectomy, is a surgical weight-loss procedure, typically performed laparoscopically, in which approximately 75 - 85% of the stomach is removed, along the greater curvature, which leaves a cylindrical, or "sleeve"-shaped stomach the size of a banana. Weight loss is affected not only through the reduction of the organ's size, but by the removal of the portion of it that produces ghrelin, the hormone that stimulates appetite. Patients can lose 50-70 percent of excess weight over the course of the two years that follow the surgery. The procedure is irreversible, though in some uncommon cases, patients can regain the lost weight, via resumption of deleterious habits, or dilation of the stomach over time, which can require gastric sleeve revision surgery to either repair the sleeve or convert it to another type of weight loss method that may produce better results, such as a gastric bypass or duodenal switch.
Tubal reversal, also called tubal sterilization reversal, tubal ligation reversal, or microsurgical tubal reanastomosis, is a surgical procedure that can restore fertility to women after a tubal ligation. By rejoining the separated segments of the fallopian tube, tubal reversal can give women the chance to become pregnant again. In some cases, however, the separated segments cannot actually be reattached to each other. In some cases the remaining segment of tube needs to be re-implanted into the uterus. In other cases, when the end of the tube has been removed, a procedure called a neofimbrioplasty must be performed to recreate a functional end of the tube which can then act like the missing fimbria and retrieve the egg that has been released during ovulation.
Bariatric surgery is the medical term for a variety of procedures dealing with obesity. Long term weight loss through the standard of care procedures is largely achieved by altering gut hormone levels responsible for hunger and satiety, leading to a new hormonal weight set point. Bariatric surgery is the most effective treatment causing weight loss and reducing complications of obesity.
Gastroparesis, also called delayed gastric emptying, is a medical disorder consisting of weak muscular contractions (peristalsis) of the stomach, resulting in food and liquid remaining in the stomach for a prolonged period of time. Stomach contents thus exit more slowly into the duodenum of the digestive tract. This can result in irregular absorption of nutrients, inadequate nutrition, and poor glycemic control.

Stomach diseases include gastritis, gastroparesis, Crohn's disease and various cancers.
Preoperative fasting is the practice of a surgical patient abstaining from eating or drinking for some time before having an operation. This is intended to prevent stomach contents from getting into the windpipe and lungs while the patient is under general anesthesia. The latest guidelines do not support preoperative fasting, as there is no difference in residual gastric fluid volume, pH or gastric emptying rate following semi-solid meals or drinks, whether in obese or lean individuals.
Management of obesity can include lifestyle changes, medications, or surgery. Although many studies have sought effective interventions, there is currently no evidence-based, well-defined, and efficient intervention to prevent obesity.

Gastric electrical stimulation, also known as implantable gastric stimulation, is the use of specific devices to provide electrical stimulation to the stomach to try to bring about weight loss in those who are overweight or improve gastroparesis.
A gastric balloon, also known as an intragastric balloon (IGB) or a stomach balloon, is an inflatable medical device that is temporarily placed into the stomach to help reduce weight. It is designed to help provide weight loss when diet and exercise have failed and surgery is not wanted or not recommended for the patient.
A duodenal-jejunal bypass liner, commonly called an EndoBarrier, is an implantable medical device in the form of a thin flexible 60 cm-long tube that creates a physical barrier between ingested food and the duodenum/proximal jejunum. The duodenal-jejunal bypass liner prevents the interaction of food with enzymes and hormones in the proximal intestine to treat type 2 diabetes and obesity. The duodenal-jejunal bypass liner is delivered endoscopically and has been tested on the morbidly obese as well as obese patients with a BMI less than 40, particularly those with difficult-to-manage type 2 diabetes. Despite a handful of serious adverse events such as gastrointestinal bleeding, abdominal pain, and device migration — all resolved with device removal — initial clinical trials have produced promising results in the treatment's ability to improve weight loss and glucose homeostasis outcomes.
In medicine, endoscopic sleeve gastroplasty (ESG) is a minimally-invasive, non-surgical (incisionless), endoscopic weight loss procedure that is part of the field of endoscopic bariatric therapies. To perform ESG, a physician sutures a patient’s stomach into a narrower, smaller tube-like configuration. The result is a more restricted stomach that forces patients to feel fuller sooner, eating fewer calories, which facilitates weight loss.
Buried bumper syndrome (BBS) is a condition that affects feeding tubes placed into the stomach through the abdominal wall. Gastrostomy tubes include an internal bumper, which secures the inner portion of the tube inside the stomach, and external bumper, which secures the outer portion of the tube and opposes the abdomen. Buried bumper syndrome occurs when the internal bumper of a gastrostomy tube erodes into the wall of the stomach. The internal bumper may become entirely buried within the fistulous tract. The main causative factor is excessive tightening of the external bumper, leading to increased pressure of the internal bumper on the wall of the stomach. Additional risk factors include: obesity, weight gain, malnutrition, corticosteroid therapy, and poor wound healing.
Gelesis100, sold under the brand name Plenity, is an oral hydrogel used to treat overweight and obesity. It absorbs water and expands in the stomach and small bowel thereby increasing feelings of fullness. Possible side effects include primarily gastrointestinal symptoms, such as diarrhea, abdominal distention, infrequent bowel movements, constipation, abdominal pain, and flatulence. It is contraindicated in pregnancy, chronic malabsorption syndromes, and cholestasis. The US Food and Drug Administration approved it in 2019 as a medical device. Gelesis100 was developed by the company Gelesis.
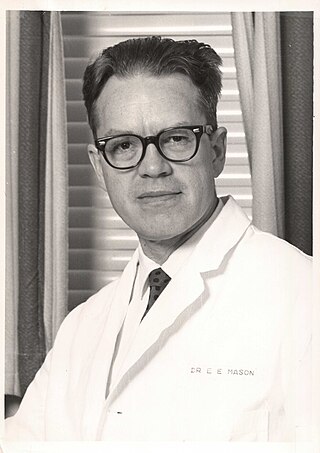
Edward Eaton Mason was an American surgeon, professor, and medical researcher who specialized in obesity surgery. He is known for developing restrictive gastric surgery for morbidly obese patients. Mason introduced the first gastric bypass surgery in 1966 and was the inventor of the first vertical banded gastroplasty surgery in 1980.
References
- 1 2 Sullivan S, Stein R, Jonnalagadda S, Mullady D, Edmundowicz S (2013). "Aspiration therapy leads to weight loss in obese subjects: a pilot study". Gastroenterology. 145 (6): 1245–52.e1–5. doi:10.1053/j.gastro.2013.08.056. PMC 4025911 . PMID 24012983.
- 1 2 Blythe Bernhard (June 15, 2016). "Reverse feeding tube developed in St. Louis is approved to treat obesity". St. Louis Post-Dispatch. Retrieved June 15, 2016.
- 1 2 3 4 FDA release. June 14, 2016
- 1 2 3 4 "Aspire Bariatrics website". Archived from the original on 2016-06-17. Retrieved 2016-06-16.
- ↑ Kumar, N (25 July 2015). "Endoscopic therapy for weight loss: Gastroplasty, duodenal sleeves, intragastric balloons, and aspiration". World Journal of Gastrointestinal Endoscopy. 7 (9): 847–59. doi: 10.4253/wjge.v7.i9.847 . PMC 4515419 . PMID 26240686.