A hernia is the abnormal exit of tissue or an organ, such as the bowel, through the wall of the cavity in which it normally resides. Hernias come in a number of types. Most commonly they involve the abdomen, specifically the groin. Groin hernias are most commonly of the inguinal type but may also be femoral. Other hernias include hiatus, incisional, and umbilical hernias. Symptoms are present in about 66% of people with groin hernias. This may include pain or discomfort, especially with coughing, exercise or going to the bathroom. Often, it gets worse throughout the day and improves when lying down. A bulging area may appear that becomes larger when bearing down. Groin hernias occur more often on the right than left side. The main concern is strangulation, where the blood supply to part of the bowel is blocked. This usually produces severe pain and tenderness in the area. Hiatus, or hiatal, hernias often result in heartburn but may also cause chest pain or pain with eating.

Skin grafting, a type of graft surgery, involves the transplantation of skin. The transplanted tissue is called a skin graft.
Chin augmentation using surgical implants can alter the underlying structure of the face, providing better balance to the facial features. The specific medical terms mentoplasty and genioplasty are used to refer to the reduction and addition of material to a patient's chin. This can take the form of chin height reduction or chin rounding by osteotomy, or chin augmentation using implants.
In surgery, a sling is an implant that is intended to provide additional support to a particular tissue. It usually consists of a synthetic mesh material in the shape of a narrow ribbon but sometimes a biomaterial or the patients own tissue. The ends are usually attached to a fixed body part such as the skeleton.

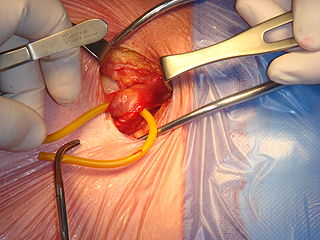
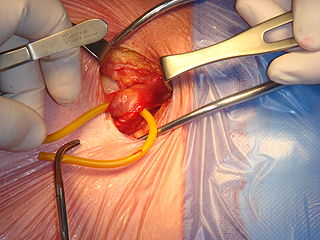
Hernia repair refers to a surgical operation for the correction of a hernia—a bulging of internal organs or tissues through the wall that contains it. It can be of two different types: herniorrhaphy; or hernioplasty. This operation may be performed to correct hernias of the abdomen, groin, diaphragm, brain, or at the site of a previous operation. Hernia repair is often performed as an ambulatory procedure.

An umbilical hernia is a health condition where the abdominal wall behind the navel is damaged. It may cause the navel to bulge outwards—the bulge consisting of abdominal fat from the greater omentum or occasionally parts of the small intestine. The bulge can often be pressed back through the hole in the abdominal wall, and may "pop out" when coughing or otherwise acting to increase intra-abdominal pressure. Treatment is surgical, and surgery may be performed for cosmetic as well as health-related reasons.

Perineal hernia is a hernia involving the perineum. The hernia may contain fluid, fat, any part of the intestine, the rectum, or the bladder. It is known to occur in humans, dogs, and other mammals, and often appears as a sudden swelling to one side of the anus.

A Spigelian is the type of ventral hernia where aponeurotic fascia pushes through a hole in the junction of the linea semilunaris and the arcuate line creating a bulge. It appears in the abdomen lower quadrant between an area of dense fibrous tissue and abdominal wall muscles causing a.
Femoral hernias occur just below the inguinal ligament, when abdominal contents pass through a naturally occurring weakness in the abdominal wall called the femoral canal. Femoral hernias are a relatively uncommon type, accounting for only 3% of all hernias. While femoral hernias can occur in both males and females, almost all develop in women due to the increased width of the female pelvis. Femoral hernias are more common in adults than in children. Those that do occur in children are more likely to be associated with a connective tissue disorder or with conditions that increase intra-abdominal pressure. Seventy percent of pediatric cases of femoral hernias occur in infants under the age of one.
An incisional hernia is a type of hernia caused by an incompletely-healed surgical wound. Since median incisions in the abdomen are frequent for abdominal exploratory surgery, ventral incisional hernias are often also classified as ventral hernias due to their location. Not all ventral hernias are from incisions, as some may be caused by other trauma or congenital problems.

A biomaterial is a substance that has been engineered to interact with biological systems for a medical purpose, either a therapeutic or a diagnostic one. As a science, biomaterials is about fifty years old. The study of biomaterials is called biomaterials science or biomaterials engineering. It has experienced steady and strong growth over its history, with many companies investing large amounts of money into the development of new products. Biomaterials science encompasses elements of medicine, biology, chemistry, tissue engineering and materials science.
Artificial skin is a collagen scaffold that induces regeneration of skin in mammals such as humans. The term was used in the late 1970s and early 1980s to describe a new treatment for massive burns. It was later discovered that treatment of deep skin wounds in adult animals and humans with this scaffold induces regeneration of the dermis. It has been developed commercially under the name IntegraTM and is used in massively burned patients, during plastic surgery of the skin, and in treatment of chronic skin wounds.
Generative Tissue (gTissue) is a living tissue created in a patient by a surgeon, consisting of an extracellular matrix, cells, and supporting vascular supply with generative properties. The 'g' in gTissue is considered a reference to both generated nature of the living tissue, but also to the generative ability of the tissue to be adapted to the dynamic environmental conditions experienced in the host.
Acellular dermis is a type of biomaterial derived from processing human or animal tissues to remove cells and retain portions of the extracellular matrix (ECM). These materials are typically cell-free, distinguishing them from classical allografts and xenografts, can be integrated or incorporated into the body, and have been FDA approved for human use for more than 10 years in a wide range of clinical indications.
Dietmar H. Wittmann, M.D., Ph.D., FACS is an academic surgeon specializing in complex abdominal surgery. He was associated with the following medical schools: University of Hamburg, Germany, University of Düsseldorf, Germany, University of California San Francisco Medical School,USA, Hahnemann Medical School, Philadelphia,USA, Medical College of Wisconsin Milwaukee, USA. In addition to his clinical work, research, publications and teaching and lecturing worldwide, he is mostly known for his work relating to intra-abdominal infections, abdominal compartment syndrome abdominal compartment syndrome and staged abdominal repair STAR. Besides introducing the concept of calculated antimicrobial therapy Wittmann conceptualized the operative strategy of Staged Abdominal Repair (STAR) or the planned open abdomen to reverse the detrimental effects of the abdominal compartment syndrome and to treat imminent intra abdominal complications before they progress to life-threatening conditions. He is the inventor of a fascia prosthesis for temporary abdominal closure, the Artificial Bur Fascia Prosthesis (generic) or Wittmann Patch and Star Patch.
Inguinal hernia surgery is an operation to repair a weakness in the abdominal wall that abnormally allows abdominal contents to slip into a narrow tube called the inguinal canal in the groin region.
The Network of Excellence for Functional Biomaterials (NFB) is a multidisciplinary research centre which hosts over sixty biologists, chemists, scientists, engineers and clinicians. It is based at the National University of Ireland, Galway, and is directed by Professor Abhay Pandit.
Free-flap breast reconstruction is a type of autologous-tissue breast reconstruction applied after mastectomy for breast cancer, without the emplacement of a breast implant prosthesis. As a type of plastic surgery, the free-flap procedure for breast reconstruction employs tissues, harvested from another part of the woman's body, to create a vascularised flap, which is equipped with its own blood vessels. Breast-reconstruction mammoplasty can sometimes be realised with the application of a pedicled flap of tissue that has been harvested from the latissimus dorsi muscle, which is the broadest muscle of the back, to which the pedicle (“foot”) of the tissue flap remains attached until it successfully grafts to the recipient site, the mastectomy wound. Moreover, if the volume of breast-tissue excised was of relatively small mass, breast augmentation procedures, such as autologous-fat grafting, also can be applied to reconstruct the breast lost to mastectomy.

Surgical mesh is a loosely woven sheet which is used as either a permanent or temporary support for organs and other tissues during surgery. Surgical mesh is created from both inorganic and biological materials and is used in a variety of surgeries. Though hernia repair surgery is the most common application, it can also be used for reconstructive work, such as in pelvic organ prolapse.
Tissue engineered heart valves (TEHV) offer a new and advancing proposed treatment of creating a living heart valve for people who are in need of either a full or partial heart valve replacement. Currently, there are over a quarter of a million prosthetic heart valves implanted annually, and the number of patients requiring replacement surgeries is only suspected to rise and even triple over the next fifty years. While current treatments offered such as mechanical valves or biological valves are not deleterious to one's health, they both have their own limitations in that mechanical valves necessitate the lifelong use of anticoagulants while biological valves are susceptible to structural degradation and reoperation. Thus, in situ tissue engineering of heart valves serves as a novel approach that explores the use creating a living heart valve composed of the host's own cells that is capable of growing, adapting, and interacting within the human body's biological system.