Diagnosis
| | This section is empty. You can help by adding to it. (September 2017) |
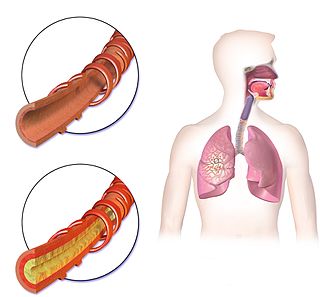
Bronchorrhea is the production of more than 100 mL per day of watery sputum. [1] Chronic bronchitis is a common cause, but it may also be caused by asthma, [2] pulmonary contusion, [3] bronchiectasis, tuberculosis, cancer, scorpion stings, severe hypothermia and poisoning by organophosphates and other poisons. Massive bronchorrhea may occur in either bronchioloalveolar carcinoma, or in metastatic cancer that is growing in a bronchioloalveolar pattern. [1] [4] [5] It commonly occurs in the setting of chest wall trauma, in which setting it can cause lobar atelectasis. [6]
| | This section is empty. You can help by adding to it. (September 2017) |
Treatment options for bronchorrhea vary depending on the inciting cause; they include:

A cough is a sudden expulsion of air through the large breathing passages which can help clear them of fluids, irritants, foreign particles and microbes. As a protective reflex, coughing can be repetitive with the cough reflex following three phases: an inhalation, a forced exhalation against a closed glottis, and a violent release of air from the lungs following opening of the glottis, usually accompanied by a distinctive sound.
Hemoptysis or haemoptysis is the discharge of blood or blood-stained mucus through the mouth coming from the bronchi, larynx, trachea, or lungs. It does not necessarily involve coughing. In other words, it is the airway bleeding. This can occur with lung cancer, infections such as tuberculosis, bronchitis, or pneumonia, and certain cardiovascular conditions. Hemoptysis is considered massive at 300 mL. In such cases, there are always severe injuries. The primary danger comes from choking, rather than blood loss.
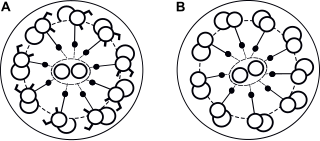
Primary ciliary dyskinesia (PCD) is a rare, autosomal recessive genetic ciliopathy, that causes defects in the action of cilia lining the upper and lower respiratory tract, sinuses, Eustachian tube, middle ear, Fallopian tube, and flagella of sperm cells. The alternative name of "immotile ciliary syndrome" is no longer favored as the cilia do have movement, but are merely inefficient or unsynchronized. When accompanied by situs inversus the condition is known as Kartagener syndrome.

Gefitinib, sold under the brand name Iressa, is a medication used for certain breast, lung and other cancers. Gefitinib is an EGFR inhibitor, like erlotinib, which interrupts signaling through the epidermal growth factor receptor (EGFR) in target cells. Therefore, it is only effective in cancers with mutated and overactive EGFR, but resistances to gefitinib can arise through other mutations. It is marketed by AstraZeneca and Teva.

Neuroendocrine tumors (NETs) are neoplasms that arise from cells of the endocrine (hormonal) and nervous systems. They most commonly occur in the intestine, where they are often called carcinoid tumors, but they are also found in the pancreas, lung, and the rest of the body.

KRAS is a gene that provides instructions for making a protein called K-Ras, a part of the RAS/MAPK pathway. The protein relays signals from outside the cell to the cell's nucleus. These signals instruct the cell to grow and divide (proliferate) or to mature and take on specialized functions (differentiate). It is called KRAS because it was first identified as a viral oncogene in the KirstenRAt Sarcoma virus. The oncogene identified was derived from a cellular genome, so KRAS, when found in a cellular genome, is called a proto-oncogene.

Adenocarcinoma in situ (AIS) of the lung —previously included in the category of "bronchioloalveolar carcinoma" (BAC)—is a subtype of lung adenocarcinoma. It tends to arise in the distal bronchioles or alveoli and is defined by a non-invasive growth pattern. This small solitary tumor exhibits pure alveolar distribution and lacks any invasion of the surrounding normal lung. If completely removed by surgery, the prognosis is excellent with up to 100% 5-year survival.
Carcinosis, or carcinomatosis, is disseminated cancer, forms of metastasis, whether used generally or in specific patterns of spread.
Malignant pleural effusion is a condition in which cancer causes an abnormal amount of fluid to collect between the thin layers of tissue (pleura) lining the outside of the lung and the wall of the chest cavity. Lung cancer and breast cancer account for about 50-65% of malignant pleural effusions. Other common causes include pleural mesothelioma and lymphoma.

Afatinib, sold under the brand name Gilotrif among others, is a medication which is used to treat non-small cell lung carcinoma (NSCLC). It belongs to the tyrosine kinase inhibitor family of medications. It is taken by mouth.
Atypical adenomatous hyperplasia is a subtype of pneumocytic hyperplasia in the lung. It can be a precursor lesion of in situ adenocarcinoma of the lung. In prostate tissue biopsy, it can be confused for adenocarcinoma of the prostate. The needle biopsy rate is less than 1%.

Combined small cell lung carcinoma is a form of multiphasic lung cancer that is diagnosed by a pathologist when a malignant tumor, arising from transformed cells originating in lung tissue, contains a component of;small cell lung carcinoma (SCLC), admixed with one components of any histological variant of non-small cell lung carcinoma (NSCLC) in any relative proportion.
Treatment of lung cancer refers to the use of medical therapies, such as surgery, radiation, chemotherapy, immunotherapy, percutaneous ablation, and palliative care, alone or in combination, in an attempt to cure or lessen the adverse impact of malignant neoplasms originating in lung tissue.

Fetal adenocarcinoma (FA) of the lung is a rare subtype of pulmonary adenocarcinoma that exhibits tissue architecture and cell characteristics that resemble fetal lung tissue upon microscopic examination. It is currently considered a variant of solid adenocarcinoma with mucin production.
Large cell lung carcinoma with rhabdoid phenotype (LCLC-RP) is a rare histological form of lung cancer, currently classified as a variant of large cell lung carcinoma (LCLC). In order for a LCLC to be subclassified as the rhabdoid phenotype variant, at least 10% of the malignant tumor cells must contain distinctive structures composed of tangled intermediate filaments that displace the cell nucleus outward toward the cell membrane. The whorled eosinophilic inclusions in LCLC-RP cells give it a microscopic resemblance to malignant cells found in rhabdomyosarcoma (RMS), a rare neoplasm arising from transformed skeletal muscle. Despite their microscopic similarities, LCLC-RP is not associated with rhabdomyosarcoma.
Targeted therapy of lung cancer refers to using agents specifically designed to selectively target molecular pathways responsible for, or that substantially drive, the malignant phenotype of lung cancer cells, and as a consequence of this (relative) selectivity, cause fewer toxic effects on normal cells.
Mucinous cystadenocarcinoma of the lung (MCACL) is a very rare malignant mucus-producing neoplasm arising from the uncontrolled growth of transformed epithelial cells originating in lung tissue.
Acinar adenocarcinoma is a histological subtype of gland-forming cancer that is diagnosed when cuboidal and/or columnar shaped malignant cells in the neoplastic tissue form acini and tubules. It is a common form of cancer occurring in the lung and prostate gland.

Giant-cell carcinoma of the lung (GCCL) is a rare histological form of large-cell lung carcinoma, a subtype of undifferentiated lung cancer, traditionally classified within the non-small-cell lung carcinomas (NSCLC).

A lung cavity or pulmonary cavity is an abnormal, thick-walled, air-filled space within the lung. Cavities in the lung can be caused by infections, cancer, autoimmune conditions, trauma, congenital defects, or pulmonary embolism. The most common cause of a single lung cavity is lung cancer. Bacterial, mycobacterial, and fungal infections are common causes of lung cavities. Globally, tuberculosis is likely the most common infectious cause of lung cavities. Less commonly, parasitic infections can cause cavities. Viral infections almost never cause cavities. The terms cavity and cyst are frequently used interchangeably; however, a cavity is thick walled, while a cyst is thin walled. The distinction is important because cystic lesions are unlikely to be cancer, while cavitary lesions are often caused by cancer.
{{cite book}}: CS1 maint: multiple names: authors list (link)