The gastrointestinal tract is the tract or passageway of the digestive system that leads from the mouth to the anus. The GI tract contains all the major organs of the digestive system, in humans and other animals, including the esophagus, stomach, and intestines. Food taken in through the mouth is digested to extract nutrients and absorb energy, and the waste expelled at the anus as feces. Gastrointestinal is an adjective meaning of or pertaining to the stomach and intestines.

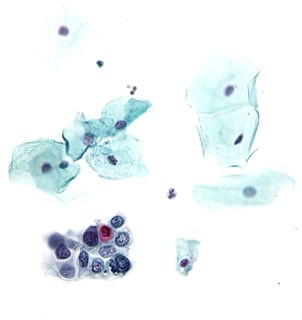
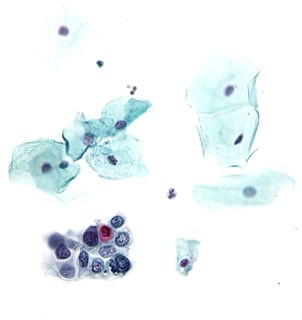
Barrett's esophagus is a condition in which there is an abnormal (metaplastic) change in the mucosal cells lining the lower portion of the esophagus, from stratified squamous epithelium to simple columnar epithelium with interspersed goblet cells that are normally present only in the small intestine and large intestine. This change is considered to be a premalignant condition because it is associated with a high incidence of further transition to esophageal adenocarcinoma, an often-deadly cancer.
Esophageal cancer is cancer arising from the esophagus—the food pipe that runs between the throat and the stomach. Symptoms often include difficulty in swallowing and weight loss. Other symptoms may include pain when swallowing, a hoarse voice, enlarged lymph nodes ("glands") around the collarbone, a dry cough, and possibly coughing up or vomiting blood.

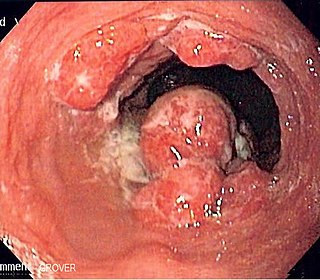
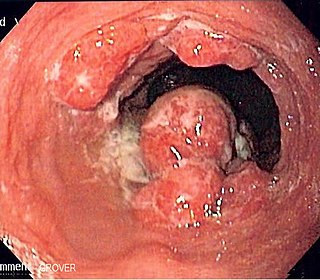
Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Oral leukoplakia is a potentially malignant disorder affecting the oral mucosa. It is defined as “essentially an oral mucosal white lesion that cannot be considered as any other definable lesion.” Oral leukoplakia is a white patch or plaque that develops in the oral cavity and is strongly associated with smoking.Leukoplakia is a firmly attached white patch on a mucous membrane which is associated with increased risk of cancer. The edges of the lesion are typically abrupt and the lesion changes with time. Advanced forms may develop red patches. There are generally no other symptoms. It usually occurs within the mouth, although sometimes mucosa in other parts of the gastrointestinal tract, urinary tract, or genitals may be affected.

Plummer–Vinson syndrome is a rare disease characterized by difficulty swallowing, iron-deficiency anemia, glossitis, cheilosis and esophageal webs. Treatment with iron supplementation and mechanical widening of the esophagus generally provides an excellent outcome.

Gastrointestinal diseases refer to diseases involving the gastrointestinal tract, namely the oesophagus, stomach, small intestine, large intestine and rectum, and the accessory organs of digestion, the liver, gallbladder, and pancreas.

Lugol's iodine, also known as aqueous iodine and strong iodine solution, is a solution of potassium iodide with iodine in water. It is a medication and disinfectant used for a number of purposes. Taken by mouth it is used to treat thyrotoxicosis until surgery can be carried out, protect the thyroid gland from radioactive iodine, and to treat iodine deficiency. When applied to the cervix it is used to help in screening for cervical cancer. As a disinfectant it may be applied to small wounds such as a needle stick injury. A small amount may also be used for emergency disinfection of drinking water.
A precancerous condition is a condition, tumor or lesion involving abnormal cells which are associated with an increased risk of developing into cancer. Clinically, precancerous conditions encompass a variety of abnormal tissues with an increased risk of developing into cancer. Some of the most common precancerous conditions include certain colon polyps, which can progress into colon cancer, monoclonal gammopathy of undetermined significance, which can progress into multiple myeloma or myelodysplastic syndrome. and cervical dysplasia, which can progress into cervical cancer. Bronchial premalignant lesions can progress to squamous cell carcinoma of the lung.
Gastrointestinal cancer refers to malignant conditions of the gastrointestinal tract and accessory organs of digestion, including the esophagus, stomach, biliary system, pancreas, small intestine, large intestine, rectum and anus. The symptoms relate to the organ affected and can include obstruction, abnormal bleeding or other associated problems. The diagnosis often requires endoscopy, followed by biopsy of suspicious tissue. The treatment depends on the location of the tumor, as well as the type of cancer cell and whether it has invaded other tissues or spread elsewhere. These factors also determine the prognosis.

Blood in stool looks different depending on how early it enters the digestive tract—and thus how much digestive action it has been exposed to—and how much there is. The term can refer either to melena, with a black appearance, typically originating from upper gastrointestinal bleeding; or to hematochezia, with a red color, typically originating from lower gastrointestinal bleeding. Evaluation of the blood found in stool depends on its characteristics, in terms of color, quantity and other features, which can point to its source, however, more serious conditions can present with a mixed picture, or with the form of bleeding that is found in another section of the tract. The term "blood in stool" is usually only used to describe visible blood, and not fecal occult blood, which is found only after physical examination and chemical laboratory testing.
Eosinophilic gastroenteritis (EGE) is an eosinophilic gastrointestinal disease (EGID)—a chronic inflammatory condition characterized by gastrointestinal symptoms and infiltration of the esophageal and/or GI mucosa by eosinophils and mast cells 1-8. In EGIDs, accumulation and activation of eosinophils and mast cells causes symptoms in the esophagus, stomach, duodenum, ileum, and colon (EC)6, 9-13. EGE is an umbrella term that includes EG, EoD, or both.

A colorectal polyp is a polyp occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
Epithelial dysplasia, a term becoming increasingly referred to as intraepithelial neoplasia, is the sum of various disturbances of epithelial proliferation and differentiation as seen microscopically. Individual cellular features of dysplasia are called epithelial atypia.
Narrow-band imaging is an imaging technique for endoscopic diagnostic medical tests, where light of specific blue and green wavelengths is used to enhance the detail of certain aspects of the surface of the mucosa. A special filter is electronically activated by a switch in the endoscope leading to the use of ambient light of wavelengths of 415 nm (blue) and 540 nm (green). Because the peak light absorption of hemoglobin occurs at these wavelengths, blood vessels will appear very dark, allowing for their improved visibility and in the improved identification of other surface structures.
Endoscopic mucosal resection is a technique used to remove cancerous or other abnormal lesions found in the digestive tract. It is one method of performing a mucosectomy.

Field cancerization is a biological process in which large areas of cells at a tissue surface or within an organ are affected by carcinogenic alterations. The process arises from exposure to an injurious environment, often over a lengthy period.

The gastrointestinal wall of the gastrointestinal tract is made up of four layers of specialised tissue. From the inner cavity of the gut outwards, these are:
Endoscopic submucosal dissection (ESD) is an advanced surgical procedure using endoscopy to remove gastrointestinal tumors that have not entered the muscle layer. ESD may be done in the esophagus, stomach or colon. Application of endoscopic resection (ER) to gastrointestinal (GI) neoplasms is limited to lesions with no risk of nodal metastasis. Either polypectomy or endoscopic mucosal resection (EMR) is beneficial for patients because of its low level of invasiveness. However, to ensure the curative potential of these treatment modalities, accurate histopathologic assessment of the resected specimens is essential because the depth of invasion and lymphovascular infiltration of the tumor is associated with considerable risk for lymph node metastasis. For accurate assessment of the appropriateness of the therapy, en bloc resection is more desirable than piecemeal resection. For a reliable en bloc resection of GI neoplasms, a new method of ER called endoscopic submucosal dissection (ESD) has been developed.