Related Research Articles

Retinopathy is any damage to the retina of the eyes, which may cause vision impairment. Retinopathy often refers to retinal vascular disease, or damage to the retina caused by abnormal blood flow. Age-related macular degeneration is technically included under the umbrella term retinopathy but is often discussed as a separate entity. Retinopathy, or retinal vascular disease, can be broadly categorized into proliferative and non-proliferative types. Frequently, retinopathy is an ocular manifestation of systemic disease as seen in diabetes or hypertension. Diabetes is the most common cause of retinopathy in the U.S. as of 2008. Diabetic retinopathy is the leading cause of blindness in working-aged people. It accounts for about 5% of blindness worldwide and is designated a priority eye disease by the World Health Organization.
In medicine, comorbidity—from Latin morbus ("sickness"), co ("together"), -ity —is the presence of one or more additional conditions often co-occurring with a primary condition. Comorbidity describes the effect of all other conditions an individual patient might have other than the primary condition of interest, and can be physiological or psychological. In the context of mental health, comorbidity often refers to disorders that are often coexistent with each other, such as depression and anxiety disorders. The concept of multimorbidity is related to comorbidity but presents a different meaning and approach.

An electronic health record (EHR) is the systematized collection of patient and population electronically stored health information in a digital format. These records can be shared across different health care settings. Records are shared through network-connected, enterprise-wide information systems or other information networks and exchanges. EHRs may include a range of data, including demographics, medical history, medication and allergies, immunization status, laboratory test results, radiology images, vital signs, personal statistics like age and weight, and billing information.
Glycated hemoglobin is a form of hemoglobin (Hb) that is chemically linked to a sugar. Most monosaccharides, including glucose, galactose and fructose, spontaneously bond with hemoglobin when present in the bloodstream. However, glucose is only 21% as likely to do so as galactose and 13% as likely to do so as fructose, which may explain why glucose is used as the primary metabolic fuel in humans.
eHealth describes healthcare services which are supported by digital processes, communication or technology such as electronic prescribing, Telehealth, or Electronic Health Records (EHRs). The use of electronic processes in healthcare dated back to at least the 1990s. Usage of the term varies as it covers not just "Internet medicine" as it was conceived during that time, but also "virtually everything related to computers and medicine". A study in 2005 found 51 unique definitions. Some argue that it is interchangeable with health informatics with a broad definition covering electronic/digital processes in health while others use it in the narrower sense of healthcare practice using the Internet. It can also include health applications and links on mobile phones, referred to as mHealth or m-Health. Key components of eHealth include electronic health records (EHRs), telemedicine, health information exchange, mobile health applications, wearable devices, and online health information. These technologies enable healthcare providers, patients, and other stakeholders to access, manage, and exchange health information more effectively, leading to improved communication, decision-making, and overall healthcare outcomes.
Disease management is defined as "a system of coordinated healthcare interventions and communications for populations with conditions in which patient self-care efforts are significant."

The Healthcare Effectiveness Data and Information Set (HEDIS) is a widely used set of performance measures in the managed care industry, developed and maintained by the National Committee for Quality Assurance (NCQA).

A primary care physician (PCP) is a physician who provides both the first contact for a person with an undiagnosed health concern as well as continuing care of varied medical conditions, not limited by cause, organ system, or diagnosis. The term is primarily used in the United States. In the past, the equivalent term was 'general practitioner' in the US; however in the United Kingdom and other countries the term general practitioner is still used. With the advent of nurses as PCPs, the term PCP has also been expanded to denote primary care providers.
Public health surveillance is, according to the World Health Organization (WHO), "the continuous, systematic collection, analysis and interpretation of health-related data needed for the planning, implementation, and evaluation of public health practice." Public health surveillance may be used to track emerging health-related issues at an early stage and find active solutions in a timely manner. Surveillance systems are generally called upon to provide information regarding when and where health problems are occurring and who is affected.
The term diabetes includes several different metabolic disorders that all, if left untreated, result in abnormally high concentrations of a sugar called glucose in the blood. Diabetes mellitus type 1 results when the pancreas no longer produces significant amounts of the hormone insulin, usually owing to the autoimmune destruction of the insulin-producing beta cells of the pancreas. Diabetes mellitus type 2, in contrast, is now thought to result from autoimmune attacks on the pancreas and/or insulin resistance. The pancreas of a person with type 2 diabetes may be producing normal or even abnormally large amounts of insulin. Other forms of diabetes mellitus, such as the various forms of maturity-onset diabetes of the young, may represent some combination of insufficient insulin production and insulin resistance. Some degree of insulin resistance may also be present in a person with type 1 diabetes.
In the healthcare industry, pay for performance (P4P), also known as "value-based purchasing", is a payment model that offers financial incentives to physicians, hospitals, medical groups, and other healthcare providers for meeting certain performance measures. Clinical outcomes, such as longer survival, are difficult to measure, so pay for performance systems usually evaluate process quality and efficiency, such as measuring blood pressure, lowering blood pressure, or counseling patients to stop smoking. This model also penalizes health care providers for poor outcomes, medical errors, or increased costs. Integrated delivery systems where insurers and providers share in the cost are intended to help align incentives for value-based care.
Patient safety is a discipline that emphasizes safety in health care through the prevention, reduction, reporting and analysis of error and other types of unnecessary harm that often lead to adverse patient events. The frequency and magnitude of avoidable adverse events, often known as patient safety incidents, experienced by patients was not well known until the 1990s, when multiple countries reported significant numbers of patients harmed and killed by medical errors. Recognizing that healthcare errors impact 1 in every 10 patients around the world, the World Health Organization (WHO) calls patient safety an endemic concern. Indeed, patient safety has emerged as a distinct healthcare discipline supported by an immature yet developing scientific framework. There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety with mobile health apps being a growing area of research.
The medical home, also known as the patient-centered medical home (PCMH), is a team-based health care delivery model led by a health care provider to provide comprehensive and continuous medical care to patients with a goal to obtain maximal health outcomes. It is described in the "Joint Principles" as "an approach to providing comprehensive primary care for children, youth and adults."
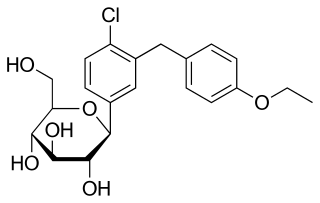
Dapagliflozin, sold under the brand names Farxiga (US) and Forxiga (EU) among others, is a medication used to treat type 2 diabetes. It is also used to treat adults with heart failure and chronic kidney disease.
Unwarranted variation in health care service delivery refers to medical practice pattern variation that cannot be explained by illness, medical need, or the dictates of evidence-based medicine. It is one of the causes of low value care often ignored by health systems.

The Brooklyn Hospital Center is a 464-licensed-bed, full-service community teaching hospital located in Downtown Brooklyn, New York City. The hospital was founded in 1845. It is affiliated with the Mount Sinai Health System, and serves a diverse population from a wide range of ethnic backgrounds.
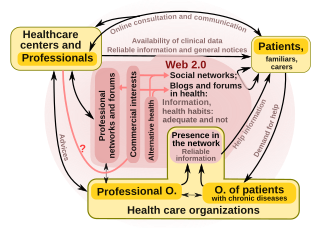
"Health 2.0" is a term introduced in the mid-2000s, as the subset of health care technologies mirroring the wider Web 2.0 movement. It has been defined variously as including social media, user-generated content, and cloud-based and mobile technologies. Some Health 2.0 proponents see these technologies as empowering patients to have greater control over their own health care and diminishing medical paternalism. Critics of the technologies have expressed concerns about possible misinformation and violations of patient privacy.
Health information technology (HIT) is health technology, particularly information technology, applied to health and health care. It supports health information management across computerized systems and the secure exchange of health information between consumers, providers, payers, and quality monitors. Based on a 2008 report on a small series of studies conducted at four sites that provide ambulatory care – three U.S. medical centers and one in the Netherlands, the use of electronic health records (EHRs) was viewed as the most promising tool for improving the overall quality, safety and efficiency of the health delivery system.

Remote patient monitoring (RPM) is a technology to enable monitoring of patients outside of conventional clinical settings, such as in the home or in a remote area, which may increase access to care and decrease healthcare delivery costs. RPM involves the constant remote care of patients by their physicians, often to track physical symptoms, chronic conditions, or post-hospitalization rehab.
Digital health is a discipline that includes digital care programs, technologies with health, healthcare, living, and society to enhance the efficiency of healthcare delivery and to make medicine more personalized and precise. It uses information and communication technologies to facilitate understanding of health problems and challenges faced by people receiving medical treatment and social prescribing in more personalised and precise ways. The definitions of digital health and its remits overlap in many ways with those of health and medical informatics.
References
- ↑ McNeil, JJ; Piccenna, L; Ronaldson, K; et al. (2010). "The Value of Patient-Centered Registries in Phase IV Drug Surveillance". Pharm Med. 24 (5): 281–288. doi:10.1007/bf03256826. S2CID 19091146. Archived from the original on 2012-07-07. Retrieved 2011-06-17.
- ↑ "ACP Observer, September 2005 - Patient registries: a key step to quality improvement". Archived from the original on 2012-07-31.
- ↑ DesRoches, Catherine M.; Campbell, Eric G.; Rao, Sowmya R.; Donelan, Karen; Ferris, Timothy G.; Jha, Ashish; Kaushal, Rainu; Levy, Douglas E.; Rosenbaum, Sara; Shields, Alexandra E.; Blumenthal, David (3 July 2008). "Electronic Health Records in Ambulatory Care — A National Survey of Physicians". New England Journal of Medicine. 359 (1): 50–60. doi: 10.1056/NEJMsa0802005 . PMID 18565855.
- ↑ "Chronic Diseases and Health Promotion". Archived from the original on 2011-07-26. Retrieved 2008-07-09.
- ↑ "The High Concentration of U.S. Health Care Expenditures: Research in Action, Issue 19, Chart 1". Archived from the original on 2008-07-09. Retrieved 2008-06-26.
- ↑ "DAGC.ORG - Diabetes Statistics - United States".
- ↑ Association, American Diabetes (1 January 2003). "Standards of Medical Care for Patients With Diabetes Mellitus". Diabetes Care. 26 (suppl 1): s33–s50. doi: 10.2337/diacare.26.2007.S33 . PMID 12502618 – via care.diabetesjournals.org.
- ↑ The NYC Hemoglobin A1C Registry (NYCAR) : Diabetes Prevention and Control Program : NYC DOHMH Archived June 9, 2007, at the Wayback Machine
- ↑ Hannan, Edward L.; Racz, Michael J.; Walford, Gary; Jones, Robert H.; Ryan, Thomas J.; Bennett, Edward; Culliford, Alfred T.; Isom, O. Wayne; Gold, Jeffrey P.; Rose, Eric A. (26 May 2005). "Long-Term Outcomes of Coronary-Artery Bypass Grafting versus Stent Implantation". New England Journal of Medicine. 352 (21): 2174–2183. doi: 10.1056/NEJMoa040316 . PMID 15917382.
- ↑ "JAMA – The Latest Medical Research, Reviews, and Guidelines". jama.ama-assn.org.
- ↑ "Cervical cancer screening guideline: October 2006. - National Guideline Clearinghouse". www.guideline.gov. Archived from the original on 2008-09-28. Retrieved 2008-06-26.
- ↑ McNeil, JJ; Piccenna, L; Ronaldson, K; et al. (2010). "The value of patient-centred registries in phase IV drug surveillance". Pharm Med. 24 (5): 281–288. doi:10.1007/bf03256826. S2CID 19091146. Archived from the original on 2012-07-07. Retrieved 2011-06-17.
- ↑ "RWD / RWE Guide - RemedyBytes". 2023-02-21. Retrieved 2023-03-16.
- ↑ Larsson, Stefan; Lawyer, Peter; Silverstein, Martin B. (November 2010). "From Concept to Reality: Putting Value-Based Health Care into Practice in Sweden". Boston Consulting Group. Retrieved 2011-07-06.
- ↑ "American Joint Replacement Registry - Improving orthopaedic care through data". ajrr.net. Archived from the original on 2016-02-08. Retrieved 2016-02-03.
- ↑ Meier, Barry (2008-07-29). "A call for a warning system on artificial joints". The New York Times .
- ↑ Cohen, Joshua T.; Neumann, Peter J.; Weinstein, Milton C. (14 February 2008). "Does Preventive Care Save Money? Health Economics and the Presidential Candidates". New England Journal of Medicine. 358 (7): 661–663. doi: 10.1056/NEJMp0708558 . PMID 18272889.
- ↑ "Chronic Disease - Overview". Archived from the original on 2011-07-26. Retrieved 2008-07-09.
- ↑ Doran, Tim; Fullwood, Catherine; Gravelle, Hugh; Reeves, David; Kontopantelis, Evangelos; Hiroeh, Urara; Roland, Martin (27 July 2006). "Pay-for-Performance Programs in Family Practices in the United Kingdom". New England Journal of Medicine. 355 (4): 375–384. doi: 10.1056/NEJMsa055505 . PMID 16870916. S2CID 22548030.
- ↑ "Overview". www.cms.hhs.gov. 11 October 2017. Archived from the original on 18 March 2023. Retrieved 26 June 2008.
- ↑ "NCQA > 404error". www.ncqa.org.
- ↑ "NCQA > 404error". www.ncqa.org.
- ↑ Newton, K. M.; Wagner, E. H.; Ramsey, S. D.; McCulloch, D.; Evans, R.; Sandhu, N.; Davis, C. (1999). "Redirecting". Journal of Clinical Epidemiology. 52 (3): 199–207. doi:10.1016/S0895-4356(98)00161-9. PMID 10210237.
- ↑ "Home".
- ↑ "Home".
- ↑ "Invitae - Patient Insights Network". www.patientcrossroads.com.
- ↑ "Gaucher Disease - The ICGG Gaucher Registry". www.gauchercare.com. Archived from the original on 2014-08-26. Retrieved 2014-08-25.
- ↑ "Home page - Vasotens Registry". VASOTENS.
- ↑ "TREAT-NMD : List of registries by disease". www.treat-nmd.eu. Retrieved 2018-06-13.