Related Research Articles

Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. CBT focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include the treatment of many mental health conditions, including anxiety, substance use disorders, marital problems, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.
Borderline personality disorder (BPD), also known as emotionally unstable personality disorder (EUPD), is a personality disorder characterized by a long-term pattern of unstable interpersonal relationships, distorted sense of self, and strong emotional reactions. Those affected often engage in self-harm and other dangerous behaviors, often due to their difficulty with returning their emotional level to a healthy or normal baseline. They may also struggle with a feeling of emptiness, fear of abandonment, and detachment from reality. Symptoms of BPD may be triggered by events considered normal to others. BPD typically begins by early adulthood and occurs across a variety of situations. Substance use disorders, depression, and eating disorders are commonly associated with BPD. Some 8 to 10% of people affected by the disorder may die by suicide. The disorder is often stigmatized in both the media and the psychiatric field and as a result is often underdiagnosed.

Psychology is an academic and applied discipline involving the scientific study of human mental functions and behavior. Occasionally, in addition or opposition to employing the scientific method, it also relies on symbolic interpretation and critical analysis, although these traditions have tended to be less pronounced than in other social sciences, such as sociology. Psychologists study phenomena such as perception, cognition, emotion, personality, behavior, and interpersonal relationships. Some, especially depth psychologists, also study the unconscious mind.
Binge eating is a pattern of disordered eating which consists of episodes of uncontrollable eating. It is a common symptom of eating disorders such as binge eating disorder and bulimia nervosa. During such binges, a person rapidly consumes an excessive quantity of food. A diagnosis of binge eating is associated with feelings of loss of control. Binge eating disorder is also linked with being overweight and obesity.
Drug rehabilitation is the process of medical or psychotherapeutic treatment for dependency on psychoactive substances such as alcohol, prescription drugs, and street drugs such as cannabis, cocaine, heroin or amphetamines. The general intent is to enable the patient to confront substance dependence, if present, and stop substance misuse to avoid the psychological, legal, financial, social, and physical consequences that can be caused.

Dialectical behavior therapy (DBT) is an evidence-based psychotherapy that began with efforts to treat personality disorders and interpersonal conflicts. There is evidence that DBT can be useful in treating mood disorders, suicidal ideation, and for change in behavioral patterns such as self-harm and substance use. DBT evolved into a process in which the therapist and client work with acceptance and change-oriented strategies, and ultimately balance and synthesize them, in a manner comparable to the philosophical dialectical process of thesis and antithesis, followed by synthesis.

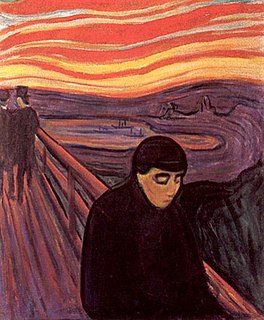
Art therapy is a distinct discipline that incorporates creative methods of expression through visual art media. Art therapy, as a creative arts therapy profession, originated in the fields of art and psychotherapy and may vary in definition.

Emotional reasoning is a cognitive process by which an individual concludes that their emotional reaction proves something is true, despite contrary empirical evidence. Emotional reasoning creates an 'emotional truth', which may be in direct conflict with the inverse 'perceptional truth'. It can create feelings of anxiety, fear, and apprehension in existing stressful situations, and as such, is often associated with or triggered by panic disorder or anxiety disorder. For example, even though a spouse has shown only devotion, a person using emotional reasoning might conclude, "I know my spouse is being unfaithful because I feel jealous."
Marsha M. Linehan is an American psychologist and author. She is the creator of dialectical behavior therapy (DBT), a type of psychotherapy that combines behavioral science with concepts like acceptance and mindfulness.
Self-compassion is extending compassion to one's self in instances of perceived inadequacy, failure, or general suffering. Kristin Neff has defined self-compassion as being composed of three main elements – self-kindness, common humanity, and mindfulness.
Trauma Systems Therapy (TST) is a mental health treatment model for children and adolescents who have been exposed to trauma, defined as experiencing, witnessing, or confronting "an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others". TST focuses on the child's emotional and behavioral needs as well as the environments where the child lives. The treatment model includes four components that are fully described in a published manual. A clinical trial showed that TST is effective in improving the mental health and well-being of children who have been traumatized. TST has also been successfully replicated.
The mainstay of management of borderline personality disorder is various forms of psychotherapy with medications being found to be of little use.
Schema therapy was developed by Jeffrey E. Young for use in treatment of personality disorders and chronic DSM Axis I disorders, such as when patients fail to respond or relapse after having been through other therapies. Schema therapy is an integrative psychotherapy combining theory and techniques from previously existing therapies, including cognitive behavioral therapy, psychoanalytic object relations theory, attachment theory, and Gestalt therapy.
Anorexia nervosa, often referred to simply as anorexia, is an eating disorder characterized by low weight, food restriction, body image disturbance, fear of gaining weight, and an overpowering desire to be thin. Anorexia is a term of Greek origin: an- and orexis, translating literally to "a loss of appetite"; the adjective nervosa indicating the functional and non-organic nature of the disorder. Anorexia nervosa was coined by Gull in 1873 but, despite literal translation, the symptom of hunger is frequently present and the pathological control of this instinct is a source of satisfaction for the patients.
PTSD or post-traumatic stress disorder, is a psychiatric disorder characterised by intrusive thoughts and memories, dreams or flashbacks of the event; avoidance of people, places and activities that remind the individual of the event; ongoing negative beliefs about oneself or the world, mood changes and persistent feelings of anger, guilt or fear; alterations in arousal such as increased irritability, angry outbursts, being hypervigilant, or having difficulty with concentration and sleep.
Cognitive emotional behavioral therapy (CEBT) is an extended version of cognitive behavioral therapy (CBT) aimed at helping individuals to evaluate the basis of their emotional distress and thus reduce the need for associated dysfunctional coping behaviors. This psychotherapeutic intervention draws on a range of models and techniques including dialectical behavior therapy (DBT), mindfulness meditation, acceptance and commitment therapy (ACT), and experiential exercises.
Occupational therapy is used to manage the issues caused by seasonal affective disorder (SAD). Occupational therapists assist with the management of SAD through the incorporation of a variety of healthcare disciplines into therapeutic practice. Potential patients with SAD are assessed, treated and evaluated primarily using treatments such as drug therapies, light therapies, and psychological therapies. Therapists are often involved in designing an individualised treatment plan that most effectively meets the client's goals and needs around their responsiveness to a variety of treatments.
Mode deactivation therapy (MDT) is a psychotherapeutic approach that addresses dysfunctional emotions, maladaptive behaviors and cognitive processes and contents through a number of goal-oriented, explicit systematic procedures. The name refers to the process of mode deactivation that is based on the concept of cognitive modes as introduced by Aaron T. Beck. The MDT methodology was developed by Jack A. Apsche by combining the unique validation–clarification–redirection (VCR) process step with elements from acceptance and commitment therapy (ACT), dialectical behavior therapy (DBT), and mindfulness to bring about durable behavior change.
Dynamic deconstructive psychotherapy (DDP) is a manual-based treatment for borderline personality disorder.
Distress tolerance is an emerging construct in psychology that has been conceptualized in several different ways. Broadly, however, it refers to an individual's "perceived capacity to withstand negative emotional and/or other aversive states, and the behavioral act of withstanding distressing internal states elicited by some type of stressor." Some definitions of distress tolerance have also specified that the endurance of these negative events occur in contexts in which methods to escape the distressor exist.
References
- 1 2 3 4 5 Bishop Jr., E. R. (2008). Low Self-directedness, Affect Regulation, and Dialectical Behavior Therapy: Reaching the Difficult Patient with an Eating Disorder. Presented at The Ben Franklin Institute, Summit for Clinical Excellence, Las Vegas, NV, June 5, 2008.
- ↑ Bishop, J. R. (2009). The Path to Coherence: Resolving the Mind Body Problem in Eating Disorders. Personal papers, Denver, CO.
- 1 2 3 Weiner, K. L. (2008). Psychopharmacology in Treating Eating Disorders. Presented at The Ben Franklin Institute, Summit for Clinical Excellence, Las Vegas, NV, June 5, 2008.
- ↑ Linehan, M. (1993). Cognitive-Behavioral Treatment of Borderline Personality Disorder, Skills Training Manual for Treating Borderline Personality Disorder. New York: The Guildford Press.
- ↑ Mentalization-Based Treatment for Borderline Personality Disorder: A Practical Guide . (n.d.). Retrieved March 30, 2009, from UCL PSYCHOANALYSIS UNIT : "UCL (Psychoanalysis Unit) Peter Fonagy's Homepage". Archived from the original on 2007-12-31. Retrieved 2007-05-07..
- ↑ Cloninger, C. S. (2006). The science of well-being: an integrated approach to mental health and its disorders. World Psychiatry, 5 (2): 71-76.
- ↑ Cloninger, C. S. (1993). A psychobiological model of temperament and character. Archives of General Psychiatry, 50 (12), 975-90.
- ↑ Siegel, D. J. (1999). The Developing Mind: How Relationships and the Brain Interact to Shape Who We Are. New York: Guilford.
- ↑ WebMD. (n.d.). Retrieved March 26, 2009, from Cognitive Behavioral Therapy for Eating Disorders: http://www.webmd.com/mental-health/cognitive-behavioral-therapy-for-eating-disorders.