The United States Food and Drug Administration is a federal agency of the Department of Health and Human Services. The FDA is responsible for protecting and promoting public health through the control and supervision of food safety, tobacco products, caffeine products, dietary supplements, prescription and over-the-counter pharmaceutical drugs (medications), vaccines, biopharmaceuticals, blood transfusions, medical devices, electromagnetic radiation emitting devices (ERED), cosmetics, animal foods & feed and veterinary products.

The United States Federal Food, Drug, and Cosmetic Act is a set of laws passed by the United States Congress in 1938 giving authority to the U.S. Food and Drug Administration (FDA) to oversee the safety of food, drugs, medical devices, and cosmetics. The FDA's principal representative with members of congress during its drafting was Charles W. Crawford. A principal author of this law was Royal S. Copeland, a three-term U.S. senator from New York. In 1968, the Electronic Product Radiation Control provisions were added to the FD&C. Also in that year the FDA formed the Drug Efficacy Study Implementation (DESI) to incorporate into FD&C regulations the recommendations from a National Academy of Sciences investigation of effectiveness of previously marketed drugs. The act has been amended many times, most recently to add requirements about bioterrorism preparations.
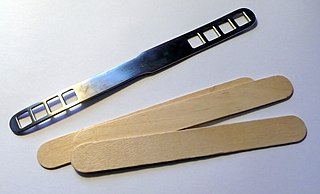
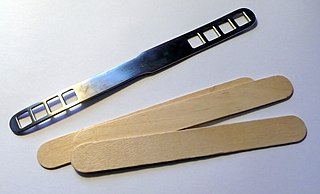
A medical device is any device intended to be used for medical purposes. Significant potential for hazards are inherent when using a device for medical purposes and thus medical devices must be proved safe and effective with reasonable assurance before regulating governments allow marketing of the device in their country. As a general rule, as the associated risk of the device increases the amount of testing required to establish safety and efficacy also increases. Further, as associated risk increases the potential benefit to the patient must also increase.
A drug recall removes a prescription or over-the-counter drug from the market. Drug recalls in the United States are made by the FDA or the creators of the drug when certain criteria are met. When a drug recall is made, the drug is removed from the market and potential legal action can be taken depending on the severity of the drug recall.
The Center for Biologics Evaluation and Research (CBER) is one of six main centers for the U.S. Food and Drug Administration (FDA), which is a part of the U.S. Department of Health and Human Services. The current Director of CBER is Peter Marks, M.D., PhD. CBER is responsible for assuring the safety, purity, potency, and effectiveness of biologics and related products. Not all biologics are regulated by CBER. Monoclonal antibodies and other therapeutic proteins are regulated by the FDA Center for Drug Evaluation and Research (CDER).
Title 21 is the portion of the Code of Federal Regulations that governs food and drugs within the United States for the Food and Drug Administration (FDA), the Drug Enforcement Administration (DEA), and the Office of National Drug Control Policy (ONDCP).

Diana M. Zuckerman is an American health policy analyst who focuses on the implications of policies for public health and patients' health. She specializes in national health policy, particularly in women's health and the safety and effectiveness of medical products. She is the President of the National Center for Health Research and the Cancer Prevention and Treatment Fund.

The Center for Drug Evaluation and Research is a division of the U.S. Food and Drug Administration (FDA) that monitors most drugs as defined in the Food, Drug, and Cosmetic Act. Some biological products are also legally considered drugs, but they are covered by the Center for Biologics Evaluation and Research. The center reviews applications for brand name, generic, and over the counter pharmaceuticals, manages US current Good Manufacturing Practice (cGMP) regulations for pharmaceutical manufacturing, determines which medications require a medical prescription, monitors advertising of approved medications, and collects and analyzes safety data about pharmaceuticals that are already on the market.

President of the United States George W. Bush signed the Food and Drug Administration Amendments Act of 2007 (FDAAA) on September 27, 2007. This law reviewed, expanded, and reaffirmed several existing pieces of legislation regulating the FDA. These changes allow the FDA to perform more comprehensive reviews of potential new drugs and devices. It was sponsored by Reps. Joe Barton and Frank Pallone and passed unanimously by the Senate.
The following outline is provided as an overview of and topical guide to clinical research:

The United States Food and Drug Administration Modernization Act of 1997 (FDAMA) amended the Federal Food, Drug, and Cosmetic Act. This act is related to the regulation of food, drugs, devices, and biological products by the FDA. These changes were made in order to recognize the changes in the way the FDA would be operating in the 21st century. The main focus of this is the acknowledgment in the advancement of technological, trade, and public health complexities.
A Humanitarian Device Exemption is an approval process provided by the United States Food and Drug Administration allowing a medical device to be marketed without requiring evidence of effectiveness. The FDA calls a device approved in this manner a "Humanitarian Use Device" (HUD).

Jeffrey Shuren is the Director of the Center for Devices and Radiological Health (CDRH) at the United States Food and Drug Administration (FDA) as of September 2009. According to Shuren,
Our center experts and programs help get safe and effective technology to patients and health care professionals on a daily basis. Rapid technological advances enable us to approve such innovations as a diagnostic test for the H1N1 influenza virus, an expandable prosthetic rib for children with abnormal growth conditions, and a test that can help detect ovarian cancer.

The National Center for Health Research is a Washington, D.C.-based non-profit organization founded in 1999. NCHR provides health-related services such as free information and training based on research findings; educating policy makers and working with the media. The President of the organisation is Diana Zuckerman. The primary program is The Cancer Prevention and Treatment Fund, which utilises an online health hotline.
The Food and Drug Administration is a federal agency of the United States, formed in 1930.

The Medical Device Regulation Act or Medical Device Amendments of 1976 was introduced by the 94th Congress of the United States. Congressman Paul G. Rogers and Senator Edward M. Kennedy were the chairperson sponsors of the medical device amendments. The Title 21 amendments were signed into law on May 28, 1976, by the 38th President of the United States Gerald R. Ford.

Safe Medical Device Amendments of 1990 or Safe Medical Devices Act sanctioned progressive reporting and tracking rules for medical devices classified by the Medical Device Regulation Act. The Act mandates reporting requirements by medical device manufacturers regarding adverse safety events and product effectiveness of devices classified as substantially equivalent to Class III medical devices. The United States Statute established the Health and Human Services Office of International Relations and a U.S. Food and Drug Administration office for regulatory activities concerning healthcare products which are considered a combinational biological, device, or drug product. The Act of Congress transferred the electronic product radiation control provisions established by the Radiation Control for Health and Safety Act.
Due to the many regulations in the industry, the design of medical devices presents significant challenges from both engineering and legal perspectives.

Between 1966 and 1973, a series of reorganizations occurred of the United States Public Health Service (PHS) within the Department of Health, Education and Welfare (HEW). The reorganization by 1968 replaced PHS's old bureau structure with two new operating agencies: the Health Services and Mental Health Administration (HSMHA) and the Consumer Protection and Environmental Health Service (CPEHS). The goal of the reorganizations was to coordinate the previously fragmented divisions to provide a holistic approach to large, overarching problems.
The Environmental Health Divisions was a unit of the U.S. Public Health Service (PHS) that focused on environmental health, existing in various forms from 1913 until 1970. It is the primary direct predecessor of the U.S. Environmental Protection Agency. It had several other names earlier in its history, including the Office of Stream Pollution Investigations and Division of Sanitary Engineering Services.