A spinal nerve is a mixed nerve, which carries motor, sensory, and autonomic signals between the spinal cord and the body. In the human body there are 31 pairs of spinal nerves, one on each side of the vertebral column. These are grouped into the corresponding cervical, thoracic, lumbar, sacral and coccygeal regions of the spine. There are eight pairs of cervical nerves, twelve pairs of thoracic nerves, five pairs of lumbar nerves, five pairs of sacral nerves, and one pair of coccygeal nerves. The spinal nerves are part of the peripheral nervous system.

The lumbar vertebrae are located between the thoracic vertebrae and pelvis. They form the lower part of the human back in humans, and the tail end of the back in quadrupeds. In humans, there are five lumbar vertebrae. The term is used to describe the anatomy of humans and quadrupeds, such as horses, pigs, or cattle. These bones are found in particular cuts of meat, including tenderloin or sirloin steak.

Lumbar spinal stenosis (LSS) is a medical condition in which the spinal canal narrows and compresses the nerves and blood vessels at the level of the lumbar vertebrae. Spinal stenosis may also affect the cervical or thoracic region, in which case it is known as cervical spinal stenosis or thoracic spinal stenosis. Lumbar spinal stenosis can cause pain in the low back or buttocks, abnormal sensations, and the absence of sensation (numbness) in the legs, thighs, feet, or buttocks, or loss of bladder and bowel control.

Spondylosis is the degeneration of the vertebral column from any cause. In the more narrow sense it refers to spinal osteoarthritis, the age-related degeneration of the spinal column, which is the most common cause of spondylosis. The degenerative process in osteoarthritis chiefly affects the vertebral bodies, the neural foramina and the facet joints. If severe, it may cause pressure on the spinal cord or nerve roots with subsequent sensory or motor disturbances, such as pain, paresthesia, imbalance, and muscle weakness in the limbs.

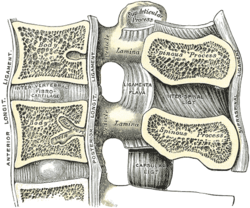
Degenerative disc disease (DDD) is a medical condition typically brought on by the normal aging process in which there are anatomic changes and possibly a loss of function of one or more intervertebral discs of the spine. DDD can take place with or without symptoms, but is typically identified once symptoms arise. The root cause is thought to be loss of soluble proteins within the fluid contained in the disc with resultant reduction of the oncotic pressure, which in turn causes loss of fluid volume. Normal downward forces cause the affected disc to lose height, and the distance between vertebrae is reduced. The anulus fibrosus, the tough outer layers of a disc, also weakens. This loss of height causes laxity of the longitudinal ligaments, which may allow anterior, posterior, or lateral shifting of the vertebral bodies, causing facet joint malalignment and arthritis; scoliosis; cervical hyperlordosis; thoracic hyperkyphosis; lumbar hyperlordosis; narrowing of the space available for the spinal tract within the vertebra ; or narrowing of the space through which a spinal nerve exits with resultant inflammation and impingement of a spinal nerve, causing a radiculopathy.

A retrolisthesis is a posterior displacement of one vertebral body with respect to the subjacent vertebra to a degree less than a luxation (dislocation). Retrolistheses are most easily diagnosed on lateral x-ray views of the spine. Views where care has been taken to expose for a true lateral view without any rotation offer the best diagnostic quality.

Spondylolisthesis is the displacement of one spinal vertebra compared to another. While some medical dictionaries define spondylolisthesis specifically as the forward or anterior displacement of a vertebra over the vertebra inferior to it, it is often defined in medical textbooks as displacement in any direction. Spondylolisthesis is graded based upon the degree of slippage of one vertebral body relative to the subsequent adjacent vertebral body. Spondylolisthesis is classified as one of the six major etiologies: degenerative, traumatic, dysplastic, isthmic, pathologic, or post-surgical. Spondylolisthesis most commonly occurs in the lumbar spine, primarily at the L5-S1 level, with the L5 vertebral body anteriorly translating over the S1 vertebral body.

The iliopsoas muscle refers to the joined psoas major and the iliacus muscles. The two muscles are separate in the abdomen, but usually merge in the thigh. They are usually given the common name iliopsoas. The iliopsoas muscle joins to the femur at the lesser trochanter. It acts as the strongest flexor of the hip.

The human back, also called the dorsum, is the large posterior area of the human body, rising from the top of the buttocks to the back of the neck. It is the surface of the body opposite from the chest and the abdomen. The vertebral column runs the length of the back and creates a central area of recession. The breadth of the back is created by the shoulders at the top and the pelvis at the bottom.

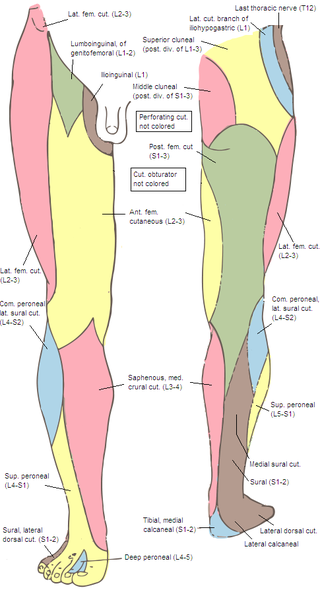
The lumbar nerves are the five pairs of spinal nerves emerging from the lumbar vertebrae. They are divided into posterior and anterior divisions.

Iliocostalis muscle is the muscle immediately lateral to the longissimus that is the nearest to the furrow that separates the epaxial muscles from the hypaxial. It lies very deep to the fleshy portion of the serratus posterior muscle. It laterally flexes the vertebral column to the same side.
A nerve root is the initial segment of a nerve leaving the central nervous system. Nerve roots can be classified as:

A spinal disc herniation is an injury to the intervertebral disc between two spinal vertebrae, usually caused by excessive strain or trauma to the spine. It may result in back pain, pain or sensation in different parts of the body, and physical disability. The most conclusive diagnostic tool for disc herniation is MRI, and treatment may range from painkillers to surgery. Protection from disc herniation is best provided by core strength and an awareness of body mechanics including good posture.

The ventral ramus is the anterior division of a spinal nerve. The ventral rami supply the antero-lateral parts of the trunk and the limbs. They are mainly larger than the dorsal rami.
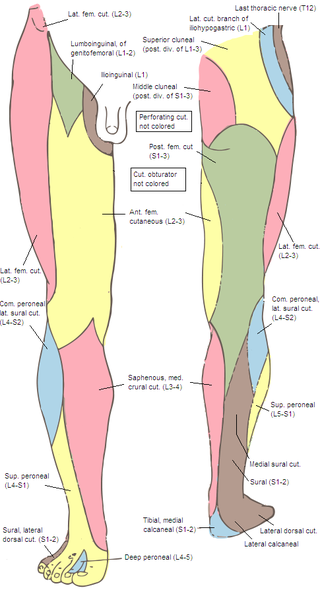
The superior cluneal nerves are pure sensory nerves that innervate the skin of the upper part of the buttocks. They are the terminal ends of the L1-L3 spinal nerve dorsal rami lateral branches. They are one of three different types of cluneal nerves. They travel inferiorly through multiple layers of muscles, then traverse osteofibrous tunnels between the thoracolumbar fascia and iliac crest.

Posterior ramus syndrome, also referred to as thoracolumbar junction syndrome, Maigne syndrome and dorsal ramus syndrome is caused by the unexplained activation of the primary division of a posterior ramus of a spinal nerve. This nerve irritation causes referred pain in a well described tri-branched pattern. The diagnosis is made clinically with the variable presence of four criteria.

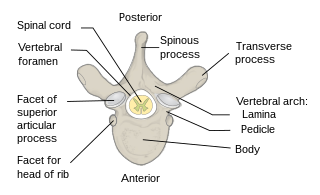
The spinal cord is a long, thin, tubular structure made up of nervous tissue that extends from the medulla oblongata in the brainstem to the lumbar region of the vertebral column (backbone) of vertebrate animals. The center of the spinal cord is hollow and contains a structure called the central canal, which contains cerebrospinal fluid. The spinal cord is also covered by meninges and enclosed by the neural arches. Together, the brain and spinal cord make up the central nervous system.

Spinal stenosis is an abnormal narrowing of the spinal canal or neural foramen that results in pressure on the spinal cord or nerve roots. Symptoms may include pain, numbness, or weakness in the arms or legs. Symptoms are typically gradual in onset and improve with leaning forward. Severe symptoms may include loss of bladder control, loss of bowel control, or sexual dysfunction.

The vertebral column, also known as the spinal column, spine or backbone, is the core part of the axial skeleton in vertebrate animals. The vertebral column is the defining and eponymous characteristic of the vertebrate endoskeleton, where the notochord found in all chordates has been replaced by a segmented series of mineralized irregular bones called vertebrae, separated by fibrocartilaginous intervertebral discs. The dorsal portion of the vertebral column houses the spinal canal, an elongated cavity formed by alignment of the vertebral neural arches that encloses and protects the spinal cord, with spinal nerves exiting via the intervertebral foramina to innervate each body segments.
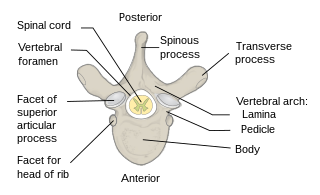
Each vertebra is an irregular bone with a complex structure composed of bone and some hyaline cartilage, that make up the vertebral column or spine, of vertebrates. The proportions of the vertebrae differ according to their spinal segment and the particular species.
9. Shin-Tsu Chang, Chuan-Ching Liu, Wan-Hua Yang. Single-photon emission computed tomography/computed tomography (hybrid imaging) in the diagnosis of unilateral facet joint arthritis after internal fixation for atlas fracture. HSOA Journal of Medicine: Study & Research 2019; 2: 010.
10. Zhu Wei Lim, Shih-Chuan Tsai, Yi-Ching Lin, Yuan-Yang Cheng, Shin-Tsu Chang. A worthwhile measurement of early vigilance and therapeutic monitor in axial spondyloarthritis: a literature review of quantitative sacroiliac scintigraphy. European Medical Journal (EMJ) Rheumatology 2021 July 15; 8[1]:129-139.