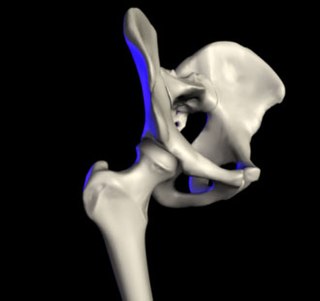
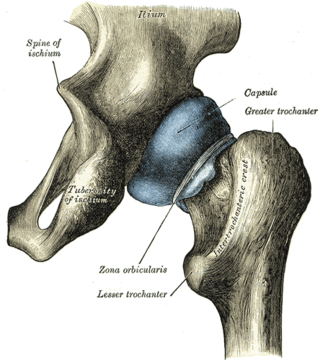
The acetabulum also called the cotyloid cavity, is a concave surface of the pelvis. The head of the femur meets with the pelvis at the acetabulum, forming the hip joint.

Arthroscopy is a minimally invasive surgical procedure on a joint in which an examination and sometimes treatment of damage is performed using an arthroscope, an endoscope that is inserted into the joint through a small incision. Arthroscopic procedures can be performed during ACL reconstruction.

Orthopedic surgery or orthopedics is the branch of surgery concerned with conditions involving the musculoskeletal system. Orthopedic surgeons use both surgical and nonsurgical means to treat musculoskeletal trauma, spine diseases, sports injuries, degenerative diseases, infections, tumors, and congenital disorders.

Osteoarthritis (OA) is a type of degenerative joint disease that results from breakdown of joint cartilage and underlying bone. It is believed to be the fourth leading cause of disability in the world, affecting 1 in 7 adults in the United States alone. The most common symptoms are joint pain and stiffness. Usually the symptoms progress slowly over years. Other symptoms may include joint swelling, decreased range of motion, and, when the back is affected, weakness or numbness of the arms and legs. The most commonly involved joints are the two near the ends of the fingers and the joint at the base of the thumbs, the knee and hip joints, and the joints of the neck and lower back. The symptoms can interfere with work and normal daily activities. Unlike some other types of arthritis, only the joints, not internal organs, are affected.
An osteotomy is a surgical operation whereby a bone is cut to shorten or lengthen it or to change its alignment. It is sometimes performed to correct a hallux valgus, or to straighten a bone that has healed crookedly following a fracture. It is also used to correct a coxa vara, genu valgum, and genu varum. The operation is done under a general anaesthetic.

Hip replacement is a surgical procedure in which the hip joint is replaced by a prosthetic implant, that is, a hip prosthesis. Hip replacement surgery can be performed as a total replacement or a hemi/semi(half) replacement. Such joint replacement orthopaedic surgery is generally conducted to relieve arthritis pain or in some hip fractures. A total hip replacement consists of replacing both the acetabulum and the femoral head while hemiarthroplasty generally only replaces the femoral head. Hip replacement is one of the most common orthopaedic operations, though patient satisfaction varies widely. Approximately 58% of total hip replacements are estimated to last 25 years. The average cost of a total hip replacement in 2012 was $40,364 in the United States, and about $7,700 to $12,000 in most European countries.
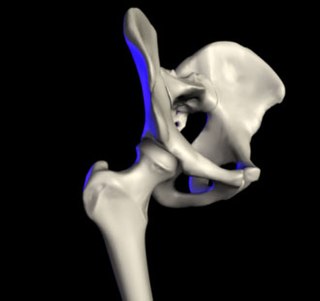
In vertebrate anatomy, the hip, or coxa(pl.: coxae) in medical terminology, refers to either an anatomical region or a joint on the outer (lateral) side of the pelvis.

A SLAP tear or SLAP lesion is an injury to the superior glenoid labrum that initiates in the back of the labrum and stretches toward the front into the attachment point of the long head of the biceps tendon. SLAP is an acronym for "Superior Labrum Anterior and Posterior". SLAP lesions are commonly seen in overhead throwing athletes but middle-aged labor workers can also be affected, and they can be caused by chronic overuse or an acute stretch injury of the shoulder.
Articular cartilage, most notably that which is found in the knee joint, is generally characterized by very low friction, high wear resistance, and poor regenerative qualities. It is responsible for much of the compressive resistance and load bearing qualities of the knee joint and, without it, walking is painful to impossible. Osteoarthritis is a common condition of cartilage failure that can lead to limited range of motion, bone damage and invariably, pain. Due to a combination of acute stress and chronic fatigue, osteoarthritis directly manifests itself in a wearing away of the articular surface and, in extreme cases, bone can be exposed in the joint. Some additional examples of cartilage failure mechanisms include cellular matrix linkage rupture, chondrocyte protein synthesis inhibition, and chondrocyte apoptosis. There are several different repair options available for cartilage damage or failure.
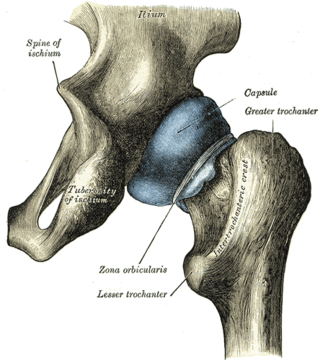
The zona orbicularis or annular ligament is a ligament on the neck of the femur formed by the circular fibers of the articular capsule of the hip joint. It is also known as the orbicular zone, ring ligament, and zonular band.

The acetabular labrum is a fibrocartilaginous ring which surrounds the circumference of the acetabulum of the hip, deepening the acetabulum. The labrum is attached onto the bony rim and transverse acetabular ligament. It is triangular in cross-section.

Extracorporeal shockwave therapy (ESWT) is a non-invasive, out-patient alternative to surgery for those with many joint and tendon disorders. ESWT sends acoustic shock waves into bone or soft tissue, in effect reinjuring the area on a cellular level and breaking up the scarring that has penetrated tendons and ligaments. The controlled reinjuring of tissue allows the body to regenerate blood vessels and bone cells. The resulting revascularization leads to faster healing and often a return to pre-injury activity levels. ESWT is mostly used for kidney stones removal, in physical therapy and orthopedics.

Hip dysplasia is an abnormality of the hip joint where the socket portion does not fully cover the ball portion, resulting in an increased risk for joint dislocation. Hip dysplasia may occur at birth or develop in early life. Regardless, it does not typically produce symptoms in babies less than a year old. Occasionally one leg may be shorter than the other. The left hip is more often affected than the right. Complications without treatment can include arthritis, limping, and low back pain. Females are affected more often than males. Risk factors for hip dysplasia include female sex, family history, certain swaddling practices, and breech presentation whether an infant is delivered vaginally or by cesarean section. If one identical twin is affected, there is a 40% risk the other will also be affected. Screening all babies for the condition by physical examination is recommended. Ultrasonography may also be useful.

Knee pain is pain in or around the knee.

Hip arthroscopy refers to the viewing of the interior of the acetabulofemoral (hip) joint through an arthroscope and the treatment of hip pathology through a minimally invasive approach. This technique is sometimes used to help in the treatment of various joint disorders and has gained popularity because of the small incisions used and shorter recovery times when compared with conventional surgical techniques. Hip arthroscopy was not feasible until recently, new technology in both the tools used and the ability to distract the hip joint has led to a recent surge in the ability to do hip arthroscopy and the popularity of it.
Osteoplasty is the branch of surgery concerned with bone repair or bone grafting. It is the surgical alteration or reshaping of bone. It may be used to relieve pain associated with metastatic bone disease. Percutaneous osteoplasty involves the use of bone cement to reduce pain and improve mobility. Resection osteoplasty is used in joint preserving surgery on the hip and thigh bones.
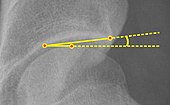
Radiographic systems to classify osteoarthritis vary by which joint is being investigated. In osteoarthritis, the choice of treatment is based on pain and decreased function, but radiography can be useful before surgery in order to prepare for the procedure.

Pain in the hip is the experience of pain in the muscles or joints in the hip/ pelvic region, a condition commonly arising from any of a number of factors. Sometimes it is closely associated with lower back pain.

Labral reconstruction is a type of hip arthroscopy in which the patient's native labrum is partially or completely removed and reconstructed using either autograft or allograft tissue. Originally described in 2009 using the ligamentum teres capitis, arthroscopic labral reconstruction using a variety of graft tissue has demonstrated promising short and mid-term clinical outcomes. Most importantly, labral reconstruction has demonstrated utility when the patient's native labral tissue is far too damaged for debridement or repair.

Ultrasound-guided hip joint injection is a joint injection in the hip, assisted by medical ultrasound. Hip and groin pain often presents a diagnostic and therapeutic challenge. The differential diagnosis is extensive, comprising intra-articular and extra-articular pathology and referred pain from lumbar spine, knee and elsewhere in the pelvis. Various ultrasound-guided techniques have been described in the hip and groin region for diagnostic and therapeutic purposes. Ultrasound has many advantages over other imaging modalities, including portability, lack of ionizing radiation and real-time visualization of soft tissues and neurovascular structures. Many studies have demonstrated the safety, accuracy and efficacy of ultrasound-guided techniques, although there is lack of standardization regarding the injectates used and long-term benefit remains uncertain.