Related Research Articles
Hemiparesis, or unilateral paresis, is weakness of one entire side of the body. Hemiplegia is, in its most severe form, complete paralysis of half of the body. Hemiparesis and hemiplegia can be caused by different medical conditions, including congenital causes, trauma, tumors, or stroke.

Complex regional pain syndrome is a severe form of chronic pain, in which pain from a physical trauma outlasts the expected recovery time. The symptoms of types 1 and 2 are the same except type 2 is associated with nerve injury.

Apraxia is a motor disorder caused by damage to the brain, which causes difficulty with motor planning to perform tasks or movements. The nature of the damage determines the disorder's severity, and the absence of sensory loss or paralysis helps to explain the level of difficulty. Children may be born with apraxia; its cause is unknown, and symptoms are usually noticed in the early stages of development. Apraxia occurring later in life, known as acquired apraxia, is typically caused by traumatic brain injury, stroke, dementia, Alzheimer's disease, brain tumor, or other neurodegenerative disorders. The multiple types of apraxia are categorized by the specific ability and/or body part affected.
Spasticity is a feature of altered skeletal muscle performance with a combination of paralysis, increased tendon reflex activity, and hypertonia. It is also colloquially referred to as an unusual "tightness", stiffness, or "pull" of muscles.
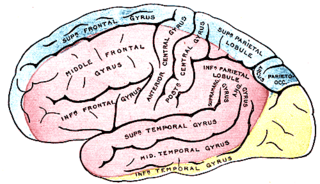
Anosognosia is a condition in which a person with a disability is cognitively unaware of having it due to an underlying physical condition. Anosognosia results from physiological damage to brain structures, typically to the parietal lobe or a diffuse lesion on the fronto-temporal-parietal area in the right hemisphere, and is thus a neuropsychiatric disorder. A deficit of self-awareness, the term was first coined by the neurologist Joseph Babinski in 1914, in order to describe the unawareness of hemiplegia.

Functional electrical stimulation (FES) is a technique that uses low-energy electrical pulses to artificially generate body movements in individuals who have been paralyzed due to injury to the central nervous system. More specifically, FES can be used to generate muscle contraction in otherwise paralyzed limbs to produce functions such as grasping, walking, bladder voiding and standing. This technology was originally used to develop neuroprostheses that were implemented to permanently substitute impaired functions in individuals with spinal cord injury (SCI), head injury, stroke and other neurological disorders. In other words, a person would use the device each time he or she wanted to generate a desired function. FES is sometimes also referred to as neuromuscular electrical stimulation (NMES).
The primary goals of stroke management are to reduce brain injury and promote maximum patient recovery. Rapid detection and appropriate emergency medical care are essential for optimizing health outcomes. When available, patients are admitted to an acute stroke unit for treatment. These units specialize in providing medical and surgical care aimed at stabilizing the patient's medical status. Standardized assessments are also performed to aid in the development of an appropriate care plan. Current research suggests that stroke units may be effective in reducing in-hospital fatality rates and the length of hospital stays.
The Bobath concept is an approach to neurological rehabilitation that is applied in patient assessment and treatment. The goal of applying the Bobath concept is to promote motor learning for efficient motor control in various environments, thereby improving participation and function. This is done through specific patient handling skills to guide patients through the initiation and completing of intended tasks. This approach to neurological rehabilitation is multidisciplinary, primarily involving physiotherapists, occupational therapists, and speech and language therapists. In the United States, the Bobath concept is also known as 'neuro-developmental treatment' (NDT).

Mirror therapy (MT) or mirror visual feedback (MVF) is a therapy for pain or disability that affects one side of the patient more than the other side. It was invented by Vilayanur S. Ramachandran to treat post-amputation patients who had phantom limb pain (PLP). Ramachandran created a visual illusion of two intact limbs by putting the patient's affected limb into a "mirror box," with a mirror down the center.
Monoplegia is paralysis of a single limb, usually an arm. Common symptoms associated with monoplegic patients are weakness, numbness, and pain in the affected limb. Monoplegia is a type of paralysis that falls under hemiplegia. While hemiplegia is paralysis of half of the body, monoplegia is localized to a single limb or to a specific region of the body. Monoplegia of the upper limb is sometimes referred to as brachial monoplegia, and that of the lower limb is called crural monoplegia. Monoplegia in the lower extremities is not as common of an occurrence as in the upper extremities. Monoparesis is a similar, but less severe, condition because one limb is very weak, not paralyzed. For more information, see paresis.
Hypertonia is a term sometimes used synonymously with spasticity and rigidity in the literature surrounding damage to the central nervous system, namely upper motor neuron lesions. Impaired ability of damaged motor neurons to regulate descending pathways gives rise to disordered spinal reflexes, increased excitability of muscle spindles, and decreased synaptic inhibition. These consequences result in abnormally increased muscle tone of symptomatic muscles. Some authors suggest that the current definition for spasticity, the velocity-dependent over-activity of the stretch reflex, is not sufficient as it fails to take into account patients exhibiting increased muscle tone in the absence of stretch reflex over-activity. They instead suggest that "reversible hypertonia" is more appropriate and represents a treatable condition that is responsive to various therapy modalities like drug or physical therapy.

Telerehabilitation (or e-rehabilitation is the delivery of rehabilitation services over telecommunication networks and the internet. Telerehabilitation allows patients to interact with providers remotely and can be used both to assess patients and to deliver therapy. Fields of medicine that utilize telerehabilitation include: physical therapy, occupational therapy, speech-language pathology, audiology, and psychology. Therapy sessions can be individual or community-based. Types of therapy available include motor training exercises, speech therapy, virtual reality, robotic therapy, goal setting, and group exercise.
The Brunnstrom Approach sets out a sequence of stages of recovery from hemiplegia after a stroke. It was developed by the Swedish physical therapist Signe Brunnström, and emphasises the synergic pattern of movement which develops during recovery. This approach encourages development of flexor and extensor synergies during early recovery, with the intention that synergic activation of muscles will, with training, transition into voluntary activation of movements.
Anterior cerebral artery syndrome is a condition whereby the blood supply from the anterior cerebral artery (ACA) is restricted, leading to a reduction of the function of the portions of the brain supplied by that vessel: the medial aspects of the frontal and parietal lobes, basal ganglia, anterior fornix and anterior corpus callosum.
Constraint-induced movement therapy is a form of rehabilitation therapy that improves upper extremity function in stroke and other central nervous system damage patients by increasing the use of their affected upper limb. Due to its high duration of treatment, the therapy has been found to frequently be infeasible when attempts have been made to apply it to clinical situations, and both patients and treating clinicians have reported poor compliance and concerns with patient safety. In the United States, the high duration of the therapy has also made the therapy not able to get reimbursed in most clinical environments.

Balance in biomechanics, is an ability to maintain the line of gravity of a body within the base of support with minimal postural sway. Sway is the horizontal movement of the centre of gravity even when a person is standing still. A certain amount of sway is essential and inevitable due to small perturbations within the body or from external triggers. An increase in sway is not necessarily an indicator of dysfunctional balance so much as it is an indicator of decreased sensorimotor control.
The National Institutes of Health Stroke Scale, or NIH Stroke Scale (NIHSS), is a tool used by healthcare providers to objectively quantify the impairment caused by a stroke and aid planning post-acute care disposition, though was intended to assess differences in interventions in clinical trials. The NIHSS was designed for the National Institute of Neurological Disorders and Stroke (NINDS) Recombinant Tissue Plasminogen Activator (rt-PA) for Acute Stroke Trial and was first published by neurologist Dr. Patrick Lyden and colleagues in 2001. Prior to the NIHSS, during the late 1980s, several stroke-deficit rating scales were in use.
The Berg Balance Scale is a widely used clinical test of a person's static and dynamic balance abilities, named after Katherine Berg, one of the developers. For functional balance tests, the BBS is generally considered to be the gold standard.
Video game rehabilitation is a process of using common video game consoles and methodology to target and improve physical and mental weaknesses through therapeutic processes. Video games are becoming an integral part of occupational therapy practice in acute, rehabilitation, and community settings. The design for video games in rehabilitation is focused on a number of fundamental principles, such as reward, goals, challenge, and meaningful play. 'Meaningful play' emerges from the relationship between player action and system outcome, apparent to the player through, visual, physical and aural feedback. Platforms that feature motion control, notably the Nintendo Wii, Microsoft's Xbox Kinect, Sony's Eye Toy, and virtual reality have all been effective in this field of research. Methodologies have been applied to all age groups, from toddlers to the elderly. It has been used in a variety of cases ranging from stroke rehabilitation, cerebral palsy and other neurological impairments, to tendinitis and multiple sclerosis. Researchers have promoted such technology based on the personalization of gaming systems to patients, allowing for further engagement and interaction. Additionally, gaming consoles have the ability to capture real-time data and provide instant feedback to the patients using the systems. Currently, several researchers have performed case studies to demonstrate the benefits of this technology. Repeat trials and experiments have shown that outcomes are easily replicated among various groups worldwide. Additionally, the outcomes have increased interest in the field, growing experiments beyond simple case studies to experiments with a larger participant base.
Stephen J. Page is an American biomedical researcher, author, clinician, and science educator who is known for his research on motor recovery and care after stroke. Page has developed stroke interventions such as modified constraint-induced movement therapy, and applications of mental practice in neurorehabilitation, including the first application of mental practice to stroke survivors to increase neuroplasticity. Page has also authored works about topics such as electrical stimulation, myoelectrics, outcome measurement, and neuromodulation. He has held professorial positions at academic institutions such as The Ohio State University Medical Center and The University of Cincinnati College of Medicine.
References
- ↑ Fugl-Meyer, Axel (1975). "The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance". Scandinavian Journal of Rehabilitation Medicine. 7 (1): 13–31. doi: 10.2340/1650197771331 . PMID 1135616.
- 1 2 "Stroke Assessment Scales Overview". The Internet Stroke Center. Retrieved 6 October 2016.
- ↑ Page, Stephen; Fulk, George (2012). "Clinically Important Differences for the Upper-Extremity Fugl-Meyer Scale in People With Minimal to Moderate Impairment Due to Chronic Stroke". Physical Therapy. 92 (6): 791–798. doi: 10.2522/ptj.20110009 . PMID 22282773.
- 1 2 3 4 Sanford, Julie; Moreland, Julie (1993). "Reliability of the Fugl-Meyer Assessment for Testing Motor Performance in Patients Following Stroke" (PDF). Rehabilitation Measures Database. 73 (7): 447–54. doi:10.1093/ptj/73.7.447. PMID 8316578.
- ↑ van der Lee (March 2001). "The responsiveness of the Action Research Arm test and the Fugl-Meyer Assessment scale in chronic stroke patients". Journal of Rehabilitation Medicine. 33 (3): 110–3. doi: 10.1080/165019701750165916 . PMID 11482350.
- ↑ KN, Arya (October 2011). "Estimating the minimal clinically important difference of an upper extremity recovery measure in subacute stroke patients". Topics in Stroke Rehabilitation. 18: 599–610. doi:10.1310/tsr18s01-599. PMID 22120029. S2CID 25782966.
- ↑ Pandiyan, S; KN, Arya (2016). "Minimal clinically important difference of the lower-extremity fugl-meyer assessment in chronic-stroke". Topics in Stroke Rehabilitation. 23 (4): 233–9. doi:10.1179/1945511915Y.0000000003. PMID 27086865. S2CID 206854192.
- ↑ Twitchell, Thomas (December 1951). "The Restoration of Motor Functioning Following Hemiplegia in Man". Brain. 74 (4): 443–480. doi:10.1093/brain/74.4.443. PMID 14895765.
- ↑ Brunnstrom, Signe (1970). Movement Therapy in Hemiplegia: A neurophysiological approach . Harper and Row. ISBN 978-0-06-140547-1 . Retrieved 6 October 2016.
Movement Therapy in Hemiplegia Brunnstrom.
- ↑ Gladstone, David; Danells, Cynthia (2002). "The Fugl-Meyer Assessment of Motor Recovery after Stroke: A Critical Review of Its Measurement Properties". Neurorehabilitation and Neural Repair. 16 (3): 232–240. doi:10.1177/154596802401105171. PMID 12234086. S2CID 5759799.
- 1 2 Crow, JL (2014). "Are the hierarchical properties of the Fugl-Meyer assessment scale the same in acute stroke and chronic stroke?". Physical Therapy. 94 (7): 977–86. doi: 10.2522/ptj.20130170 . PMID 24677254.
- ↑ "Fugl Meyer Assessment - UE" (PDF). University of Gothenburg. Retrieved 6 October 2016.
- ↑ "Rehab Measures: Fugl-Meyer Assessment of Motor Recovery after Stroke". Rehab Measures. Archived from the original on 24 September 2016. Retrieved 6 October 2016.
- ↑ Barnes, Michael (2005-03-10). Recovery after stroke. Cambridge University Press. p. 325. ISBN 978-0-521-82236-7 . Retrieved 6 October 2016.
- ↑ Mao, Hui-Fen (2002). "Analysis and Comparison of the Psychometric Properties of Three Balance Measures for Stroke Patients". Stroke. 33 (4): 1022–1027. doi: 10.1161/01.str.0000012516.63191.c5 . PMID 11935055.