Related Research Articles

Hyperprolactinaemia is the presence of abnormally high levels of prolactin in the blood. Normal levels average to about 13 ng/mL in women, and 5 ng/mL in men, with an upper normal limit of serum prolactin levels being 15–25 ng/mL for both. When the fasting levels of prolactin in blood exceed this upper limit, hyperprolactinemia is indicated.

Mastitis is inflammation of the breast or udder, usually associated with breastfeeding. Symptoms typically include local pain and redness. There is often an associated fever and general soreness. Onset is typically fairly rapid and usually occurs within the first few months of delivery. Complications can include abscess formation.
Anovulation is when the ovaries do not release an oocyte during a menstrual cycle. Therefore, ovulation does not take place. However, a woman who does not ovulate at each menstrual cycle is not necessarily going through menopause. Chronic anovulation is a common cause of infertility.
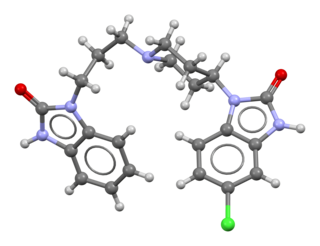
Domperidone, sold under the brand name Motilium among others, is a dopamine antagonist medication which is used to treat nausea and vomiting and certain gastrointestinal problems like gastroparesis. It raises the level of prolactin in the human body and is used to induce and promote breast milk production off label. It may be taken by mouth or rectally.

Corynebacterium is a genus of Gram-positive bacteria and most are aerobic. They are bacilli (rod-shaped), and in some phases of life they are, more specifically, club-shaped, which inspired the genus name.
Witch's milk or neonatal milk is milk secreted from the breasts of some newborn human infants of either sex. Neonatal milk secretion is considered a normal physiological occurrence and no treatment or testing is necessary. It is thought to be caused by a combination of the effects of maternal hormones before birth, prolactin, and growth hormone passed through breastfeeding and the postnatal pituitary and thyroid hormone surge in the infant.

Cabergoline, sold under the brand name Dostinex among others, is a dopaminergic medication used in the treatment of high prolactin levels, prolactinomas, Parkinson's disease, and for other indications. It is taken by mouth.

Invasive carcinoma of no special type, invasive breast carcinoma of no special type (IBC-NST), invasive ductal carcinoma (IDC), infiltrating ductal carcinoma (IDC) or invasive ductal carcinoma, not otherwise specified (NOS) is a disease. For international audiences this article will use "invasive carcinoma NST" because it is the preferred term of the World Health Organization (WHO).

Trichobacteriosis axillaris is a superficial bacterial colonization of the hair shafts in sweat gland–bearing areas, such as the armpits and the groin. It is a trivial disease of worldwide occurrence that is believed to be caused by the genus Corynebacteria.

Breast hypertrophy is a rare medical condition of the breast connective tissues in which the breasts become excessively large. The condition is often divided based on the severity into two types, macromastia and gigantomastia. Hypertrophy of the breast tissues may be caused by increased histologic sensitivity to certain hormones such as female sex hormones, prolactin, and growth factors. Breast hypertrophy is a benign progressive enlargement, which can occur in both breasts (bilateral) or only in one breast (unilateral). It was first scientifically described in 1648.

Fibrocystic breast changes is a condition of the breasts where there may be pain, breast cysts, and breast masses. The breasts may be described as "lumpy" or "doughy". Symptoms may worsen during certain parts of the menstrual cycle due to hormonal stimulation. These are normal breast changes, not associated with cancer.
Lactation suppression refers to the act of suppressing lactation by medication or other non pharmaceutical means. The breasts may become painful when engorged with milk if breastfeeding is ceased abruptly, or if never started. This may occur if a woman never initiates breastfeeding, or if she is weaning from breastfeeding abruptly. Historically women who did not plan to breastfeed were given diethylstilbestrol and other medications after birth to suppress lactation. However, its use was discontinued, and there are no medications currently approved for lactation suppression in the US and the UK. Dopamine agonists are routinely prescribed to women following a stillbirth in the UK under the NHS.
The term nonpuerperal mastitis describes inflammatory lesions of the breast (mastitis) that occur unrelated to pregnancy and breastfeeding.
Also called Zuska's disease, subareolar abscess is a subcutaneous abscess of the breast tissue beneath the areola of the nipple. It is a frequently aseptic inflammation and has been associated with squamous metaplasia of lactiferous ducts.
Silicone granulomas are a skin condition that occur as a reaction to liquid silicones, and are characterized by the formation of nodules.

Generalized granuloma annulare is a skin condition of unknown cause, tending to affect women in the fifth and sixth decades, presenting as a diffuse but symmetrical, papular or annular eruption of more than ten skin lesions, and often hundreds.
Galactorrhea hyperprolactinemia is increased blood prolactin levels associated with galactorrhea. It may be caused by such things as certain medications, pituitary disorders and thyroid disorders. The condition can occur in males as well as females. Relatively common etiologies include prolactinoma, medication effect, kidney failure, granulomatous diseases of the pituitary gland, and disorders which interfere with the hypothalamic inhibition of prolactin release. Ectopic (non-pituitary) production of prolactin may also occur. Galactorrhea hyperprolactinemia is listed as a “rare disease” by the Office of Rare Diseases of the National Institutes of Health. This means that it affects less than 200,000 people in the United States population.

Gynecomastia is the abnormal non-cancerous enlargement of one or both breasts in males due to the growth of breast tissue as a result of a hormone imbalance between estrogens and androgens. Gynecomastia can cause significant psychological distress or unease.

Mammoplasia is the normal or spontaneous enlargement of human breasts. Mammoplasia occurs normally during puberty and pregnancy in women, as well as during certain periods of the menstrual cycle. When it occurs in males, it is called gynecomastia and is considered to be pathological. When it occurs in females and is extremely excessive, it is called macromastia and is similarly considered to be pathological. Mammoplasia may be due to breast engorgement, which is temporary enlargement of the breasts caused by the production and storage of breast milk in association with lactation and/or galactorrhea. Mastodynia frequently co-occurs with mammoplasia.
The side effects of cyproterone acetate (CPA), a steroidal antiandrogen and progestin, including its frequent and rare side effects, have been studied and characterized. It is generally well-tolerated and has a mild side-effect profile, regardless of dosage, when it used as a progestin or antiandrogen in combination with an estrogen such as ethinylestradiol or estradiol valerate in women. Side effects of CPA include hypogonadism and associated symptoms such as demasculinization, sexual dysfunction, infertility, and osteoporosis; breast changes such as breast tenderness, enlargement, and gynecomastia; emotional changes such as fatigue and depression; and other side effects such as vitamin B12 deficiency, weak glucocorticoid effects, and elevated liver enzymes. Weight gain can occur with CPA when it is used at high doses. Some of the side effects of CPA can be improved or fully prevented if it is combined with an estrogen to prevent estrogen deficiency. Few quantitative data are available on many of the potential side effects of CPA. Pooled tolerability data for CPA is not available in the literature.
References
- ↑ Garcia-Rodiguez JA, Pattullo A (2013). "Idiopathic granulomatous mastitis: a mimicking disease in a pregnant woman: a case report". BMC Research Notes. 6 (95): 95. doi: 10.1186/1756-0500-6-95 . PMC 3606122 . PMID 23497626.
- ↑ El-Charnoubi, W. A.; Foged Henriksen, T; Joergen Elberg, J (2011). "Cutaneous silicone granuloma mimicking breast cancer after ruptured breast implant". Case Reports in Dermatological Medicine. 2011: 129138. doi: 10.1155/2011/129138 . PMC 3505939 . PMID 23198167.
- ↑ Symmers, W. S. (1968). "Silicone mastitis in "topless" waitresses and some other varieties of foreign-body mastitis". British Medical Journal. 3 (5609): 19–22. doi:10.1136/bmj.3.5609.8-a. PMC 1989508 . PMID 5690841.
- 1 2 3 4 5 6 7 Lin CH, Hsu CW, Tsao TY, Chou J (2012). "Idiopathic granulomatous mastitis associated with risperidone-induced hyperprolactinemia". Diagnostic Pathology. 7 (1): 2. doi: 10.1186/1746-1596-7-2 . PMC 3261802 . PMID 22221904.
- 1 2 Bellavia, M.; Damiano, G.; Palumbo, V. D.; Spinelli, G.; Tomasello, G.; Marrazzo, A.; Ficarella, S.; Bruno, A.; Sammartano, A.; Fiorentini, T.; Scio, A.; Maione, C.; Lo Monte, A. I. (2012). "Granulomatous Mastitis during Chronic Antidepressant Therapy: Is It Possible a Conservative Therapeutic Approach?". Journal of Breast Cancer. 15 (3): 371–372. doi:10.4048/jbc.2012.15.3.371. PMC 3468794 . PMID 23091553.
- ↑ Reddy KM, Meyer CE, Nakdjevani A, Shrotria S (2005). "Idiopathic Granulomatous Mastitis in the Male Breast". The Breast Journal. 11 (1): 73. doi: 10.1111/j.1075-122X.2005.21404.x . PMID 15647084. S2CID 46709562.
- ↑ Goldberg, J.; Baute, L.; Storey, L.; Park, P. (2000). "Granulomatous mastitis in pregnancy". Obstetrics and Gynecology. 96 (5 Pt 2): 813–815. doi:10.1016/S0029-7844(00)01051-6. PMID 11094217. S2CID 22262969.
- ↑ Seo HR, Na KY, Yim HE, Kim TH, et al. (2012). "Differential Diagnosis in Idiopathic Granulomatous Mastitis and Tuberculous Mastitis". Journal of Breast Cancer. 15 (1): 111–118. doi:10.4048/jbc.2012.15.1.111. PMC 3318162 . PMID 22493637.
- ↑ Schelfout, K.; Tjalma, W. A.; Cooremans, I. D.; Coeman, D. C.; Colpaert, C. G.; Buytaert, P. M. (2001). "Observations of an idiopathic granulomatous mastitis". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 97 (2): 260–262. doi:10.1016/s0301-2115(00)00546-7. PMID 11451563.
- ↑ Shaaban, H.; Slim, J.; Choo, H. (2012). "Idiopathic granulomatous mastitis as a complication of interferon-alpha therapy". North American Journal of Medical Sciences. 4 (9): 424–426. doi: 10.4103/1947-2714.101005 . PMC 3456487 . PMID 23050257.
- ↑ Ogura, K.; Matsumoto, T.; Aoki, Y.; Kitabatake, T.; Fujisawa, M.; Kojima, K. (2010). "IgG4-related tumour-forming mastitis with histological appearances of granulomatous lobular mastitis: Comparison with other types of tumour-forming mastitis". Histopathology. 57 (1): 39–45. doi:10.1111/j.1365-2559.2010.03581.x. PMID 20653779. S2CID 20439334.
- ↑ Shelly, S.; Boaz, M.; Orbach, H. (2012). "Prolactin and autoimmunity". Autoimmunity Reviews. 11 (6–7): A465–A470. doi:10.1016/j.autrev.2011.11.009. PMID 22155203.
- ↑ Bässler, R. (1997). "Mastitis. Classification, histopathology and clinical aspects". Der Pathologe. 18 (1): 27–36. doi:10.1007/s002920050193. PMID 9157401. S2CID 6107645.
- ↑ Binelli C, Lorimier G, Bertrand G, Parvery F, Bertrand AF, Verriele V (1996). "Granulomatous mastitis and corynebacteria infection. Two case reports". J Gynecol Obstet Biol Reprod (Paris). 25 (1): 27–32. PMID 8901298.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Mathelin C, Riegel P, Chenard MP, Tomasetto C, Brettes JP (2005). "Granulomatous mastitis and corynebacteria: clinical and pathologic correlations". The Breast Journal. 11 (5): 357. doi: 10.1111/j.1075-122x.2005.21562.x . PMID 16174160. S2CID 29677050.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Mathelin C, Riegel P, Chenard MP, Brettes JP (2005). "Association of corynebacteria with granulomatous mastitis". Eur J Obstet Gynecol Reprod Biol. 119 (2): 260–261. doi:10.1016/j.ejogrb.2004.08.003. PMID 15808395.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Tauch A, Fernández-Natal I, Soriano F (2016). "A microbiological and clinical review on Corynebacterium kroppenstedtii". Int J Infect Dis. 48: 33–39. doi: 10.1016/j.ijid.2016.04.023 . PMID 27155209.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Wong SC, Poon RW, Foo CH, Ngan AH, Tse H, Lam VC, Leung TH, Wong CP, Cheng VC, Chen JH, Yuen KY (2018). "Novel selective medium for the isolation of corynebacterium kroppenstedtii from heavily colonised clinical specimens". J. Clin. Pathol. 71 (9): 781–786. doi:10.1136/jclinpath-2017-204834. PMID 29593062. S2CID 4390225.
- ↑ Lai, E. C. H.; Chan, W. C.; Ma, T. K. F.; Tang, A. P. Y.; Poon, C. S. P.; Leong, H. T. (2005). "The Role of Conservative Treatment in Idiopathic Granulomatous Mastitis". The Breast Journal. 11 (6): 454–456. doi: 10.1111/j.1075-122X.2005.00127.x . PMID 16297091. S2CID 20257848.
- ↑ Imoto S, Kitaya T, Kodama T, Hasebe T, Mukai K (1997). "Idiopathic granulomatous mastitis: case report and review of the literature". Japanese Journal of Clinical Oncology (review). 27 (4): 274–277. doi:10.1093/jjco/27.4.274. PMID 9379518.
- ↑ Aldaqal, SM (2004). "Idiopathic granulomatous mastitis. Clinical presentation, radiological features and treatment". Saudi Medical Journal. 25 (12): 1884–1887. PMID 15711659.
- ↑ Krause, A.; Gerber, B.; Rhode, E. (1994). "Puerperal and non-puerperal mastitis". Zentralblatt für Gynäkologie. 116 (8): 488–491. PMID 7941820.
- ↑ Erhan, Y.; Veral, A.; Kara, E.; Ozdemir, N.; Kapkac, M.; Ozdedeli, E.; Yilmaz, R.; Koyuncu, A.; Erhan, Y.; Ozbal, O. (2000). "A clinicopthologic study of a rare clinical entity mimicking breast carcinoma: Idiopathic granulomatous mastitis". The Breast. 9 (1): 52–56. doi: 10.1054/brst.1999.0072 . PMID 14731585.
- ↑ Akbulut, S.; Arikanoglu, Z.; Senol, A.; Sogutcu, N.; Basbug, M.; Yeniaras, E.; Yagmur, Y. (2011). "Is methotrexate an acceptable treatment in the management of idiopathic granulomatous mastitis?". Archives of Gynecology and Obstetrics. 284 (5): 1189–1195. doi:10.1007/s00404-010-1825-2. PMID 21207047. S2CID 5098811.
- ↑ Ayeva-Derman, M.; Perrotin, F.; Lefrancq, T.; Roy, F.; Lansac, J.; Body, G. (1999). "Idiopathic granulomatous mastitis. Review of the literature illustrated by 4 cases". Journal de gynécologie, obstétrique et biologie de la reproduction. 28 (8): 800–807. PMID 10635482.
- ↑ Vingerhoedt, N. M.; Janssen, S.; Mravunac, M.; Wauters, C. A.; Strobbe, L. J. (2008). "Granulomatous lobular mastitis: A benign abnormality that mimics malignancy". Nederlands Tijdschrift voor Geneeskunde. 152 (18): 1052–1056. PMID 18547028.