Related Research Articles

Tripura is a state in Northeast India. The third-smallest state in the country, it covers 10,491 km2 (4,051 sq mi); and the seventh-least populous state with a population of 3.67 million. It is bordered by Assam and Mizoram to the east and by Bangladesh to the north, south and west. Tripura is divided into 8 districts and 23 sub-divisions, where Agartala is the capital and the largest city in the state. Tripura has 19 different tribal communities with a majority Bengali population. Bengali, English and Kokborok are the state's official languages.

The Kerala model refers to the practices adopted by the Indian state of Kerala to further human development. It is characterised by results showing strong social indicators when compared to the rest of the country such as high literacy and life expectancy rates, highly improved access to healthcare, and low infant mortality and birth rates. Despite having a lower per capita income, the state is sometimes compared to developed countries. These achievements along with the factors responsible for such achievements have been considered characteristic results of the Kerala model. Academic literature discusses the primary factors underlying the success of the Kerala model as its decentralization efforts, the political mobilization of the poor, and the active involvement of civil society organizations in the planning and implementation of development policies.
A public hospital, or government hospital, is a hospital which is government owned and is fully funded by the government and operates solely off the money that is collected from taxpayers to fund healthcare initiatives. In almost all the developed countries but the United States of America, and in most of the developing countries, this type of hospital provides medical care free of charge to patients, covering expenses and wages by government reimbursement.

Health care in Saudi Arabia is a national health care system in which the government provides free universal healthcare coverage through a number of government agencies. There is also a growing role and increased participation from the private sector in the provision of health care services. Saudi Arabia has been ranked among the 26 best countries in providing high quality healthcare.

NHS Scotland, sometimes styled NHSScotland, is the publicly funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.

The Ministry of Health and Family Welfare, also known by its abbreviation MoHFW, is an Indian government ministry charged with health policy in India. It is also responsible for all government programs relating to family planning in India.

The Healthcare in Kazakhstan is a post-Soviet healthcare system under reform. The World Health Organization (WHO), in 2000, ranked the Kazakhstan's healthcare system as the 64th in overall performance, and 135th by overall level of health.
Healthcare in Finland consists of a highly decentralized three-level publicly funded healthcare system and a much smaller private sector. Although the Ministry of Social Affairs and Health has the highest decision-making authority, specific healthcare precincts are responsible for providing healthcare to their residents as of 2023.

Bolpur Subdivision is an administrative subdivision of Birbhum district in the state of West Bengal, India.
An Accredited Social Health Activist (ASHA) is a community health worker employed by the Ministry of Health and Family Welfare (MoHFW) as a part of India's National Rural Health Mission (NRHM). The mission began in 2005; full implementation was targeted for 2012. The idea behind the Accredited Social Health Activist (ASHA) was to connect marginalized communities to the health care system. The target was to have an "ASHA in every village" in India. In July 2013, the number of ASHAs was reported to be 870,089. In 2018, this number became 939,978. The ideal number of ASHAs envisaged was 1,022,265.

A landlocked sub-Saharan country, Burkina Faso is among the poorest countries in the world—44 percent of its population lives below the international poverty line of US$1.90 per day —and it ranks 185th out of 188 countries on UNDP's 2016 Human Development Index .Rapid population growth, gender inequality, and low levels of educational attainment contribute to food insecurity and poverty in Burkina Faso. The total population is just over 20 million with the estimated population growth rate is 3.1 percent per year and seven out of 10 Burkinabe are younger than 30. Total health care expenditures were an estimated 5% of GDP. Total expenditure on health per capita is 82 in 2014.
Diamond Harbour II is a community development block that forms an administrative division in the Diamond Harbour subdivision of the South 24 Parganas district in the Indian state of West Bengal.
Examples of health care systems of the world, sorted by continent, are as follows.
The public healthcare system in India evolved due to a number of influences since 1947, including British influence from the colonial period. The need for an efficient and effective public health system in India is large. Public health system across nations is a conglomeration of all organized activities that prevent disease, prolong life and promote health and efficiency of its people. Indian healthcare system has been historically dominated by provisioning of medical care and neglected public health. 11.9% of all maternal deaths and 18% of all infant mortality in the world occurs in India, ranking it the highest in the world. 36.6 out of 1000 children are dead by the time they reach the age of 5. 62% of children are immunized. Communicable disease is the cause of death for 53% of all deaths in India.
Healthcare in West Bengal features a universal health care system run by the state and the federal governments. The Constitution of India charges every state with "raising of the level of nutrition and the standard of living of its people and the improvement of public health as among its primary duties". Ministry of Health & Family Welfare of the Government of West Bengal is responsible for administering and funding the public hospital system in the state. The entire state population is covered by a health insurance, either provided by their employer or the Employees’ State Insurance. Other categories of people are covered under the state’s public health insurance scheme. As of 2021, the total public healthcare budget of the state is ₹16,368 crore (US$2.0 billion), out of which ₹10,922 crore (US$1.4 billion) was earmarked for public hospitals, ₹2,000 crore (US$250 million) was to be spent on the public health insurance program and ₹5,246 crore (US$660 million) is to be spent on primary health services. An additional ₹1,000 crore (US$130 million), outside the official health budget, was to be spent on health insurance coverage for the current and retired employees of the state government. Healthcare forms roughly 4.5% of the state's entire budget which critics say should be increased to at least 8% in line with the National Health Policy.
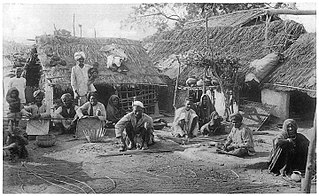
Achieving Universal Health Care has been a key goal of the Indian Government since the Constitution was drafted. The Government has since launched several programs and policies to realize ‘Health for All’ in the nation. These measures are in line with the sustainable development goals set by the United Nations. Health disparities generated through the Hindu caste system have been a major roadblock in realizing these goals. The Dalit (untouchables) community occupies the lowest stratum of the Hindu caste system. Historically, they have performed menial jobs like- manual scavenging, skinning animal hide, and sanitation. The Indian constitution officially recognizes the Dalit community as ‘Scheduled Castes’ and bans caste-based discrimination of any form. However, caste and its far-reaching effects are still prominent in several domains including healthcare. Dalits and Adivasis have the lowest healthcare utilization and outcome percentage. Their living conditions and occupations put them at high risk for disease exposure. This, clubbed with discrimination from healthcare workers and lack of awareness makes them the most disadvantaged groups in society.
Education in Tripura, a state in Northeast India, is provided by both the public sector and the private sector. On 8 September 2013, the literacy rate of Tripura was declared to be 94.65%, which is the highest among all states of India.

India has a multi-payer universal health care model that is paid for by a combination of public and private health insurance funds along with the element of almost entirely tax-funded public hospitals. The public hospital system is essentially free for all Indian residents except for small, often symbolic co-payments in some services.

Women's health in India can be examined in terms of multiple indicators, which vary by geography, socioeconomic standing and culture. To adequately improve the health of women in India multiple dimensions of wellbeing must be analysed in relation to global health averages and also in comparison to men in India. Health is an important factor that contributes to human wellbeing and economic growth.

Voluntary Health Services, popularly known as the VHS Hospital, is a multispecialty tertiary care referral hospital in the south Indian state of Tamil Nadu, reportedly serving the economically weaker sections of the society. It was founded in 1958 by Krishnaswami Srinivas Sanjivi, an Indian physician, social worker and a winner of Padma Shri and Padma Bhushan awards and is run by a charitable non governmental organization of the same name. The hospital is situated along Rajiv Gandhi Salai at Taramani, in Chennai.
References
- 1 2 "Economic review of Tripura 2010–11" (PDF). Directorate of Economics and Statistics, Planning (Statistics) Department, Government of Tripura. p. 251. Archived from the original (PDF) on 24 January 2013. Retrieved 20 April 2012.
- 1 2 3 "Economic review of Tripura 2010–11" (PDF). Directorate of Economics and Statistics, Planning (Statistics) Department, Government of Tripura. pp. 254–5. Archived from the original (PDF) on 24 January 2013. Retrieved 20 April 2012.
- 1 2 "Economic review of Tripura 2010–11" (PDF). Directorate of Economics and Statistics, Planning (Statistics) Department, Government of Tripura. pp. 259–60. Archived from the original (PDF) on 24 January 2013. Retrieved 20 April 2012.
- 1 2 3 International Institute for Population Sciences and Macro International (September 2007). "National Family Health Survey (NFHS-3), 2005–06" (PDF). Ministry of Health and Family Welfare, Government of India. p. 438. Retrieved 5 October 2012.