In aphasia, a person may be unable to comprehend or unable to formulate language because of damage to specific brain regions. The major causes are stroke and head trauma; prevalence is hard to determine but aphasia due to stroke is estimated to be 0.1–0.4% in the Global North. Aphasia can also be the result of brain tumors, epilepsy, autoimmune neurological diseases, brain infections, or neurodegenerative diseases.

Expressive aphasia, also known as Broca's aphasia, is a type of aphasia characterized by partial loss of the ability to produce language, although comprehension generally remains intact. A person with expressive aphasia will exhibit effortful speech. Speech generally includes important content words but leaves out function words that have more grammatical significance than physical meaning, such as prepositions and articles. This is known as "telegraphic speech". The person's intended message may still be understood, but their sentence will not be grammatically correct. In very severe forms of expressive aphasia, a person may only speak using single word utterances. Typically, comprehension is mildly to moderately impaired in expressive aphasia due to difficulty understanding complex grammar.

Wernicke's aphasia, also known as receptive aphasia, sensory aphasia, fluent aphasia, or posterior aphasia, is a type of aphasia in which individuals have difficulty understanding written and spoken language. Patients with Wernicke's aphasia demonstrate fluent speech, which is characterized by typical speech rate, intact syntactic abilities and effortless speech output. Writing often reflects speech in that it tends to lack content or meaning. In most cases, motor deficits do not occur in individuals with Wernicke's aphasia. Therefore, they may produce a large amount of speech without much meaning. Individuals with Wernicke's aphasia are typically unaware of their errors in speech and do not realize their speech may lack meaning. They typically remain unaware of even their most profound language deficits.

Apraxia is a motor disorder caused by damage to the brain, which causes difficulty with motor planning to perform tasks or movements. The nature of the damage determines the disorder's severity, and the absence of sensory loss or paralysis helps to explain the level of difficulty. Children may be born with apraxia; its cause is unknown, and symptoms are usually noticed in the early stages of development. Apraxia occurring later in life, known as acquired apraxia, is typically caused by traumatic brain injury, stroke, dementia, Alzheimer's disease, brain tumor, or other neurodegenerative disorders. The multiple types of apraxia are categorized by the specific ability and/or body part affected.

Agnosia is the inability to process sensory information. Often there is a loss of ability to recognize objects, persons, sounds, shapes, or smells while the specific sense is not defective nor is there any significant memory loss. It is usually associated with brain injury or neurological illness, particularly after damage to the occipitotemporal border, which is part of the ventral stream. Agnosia only affects a single modality, such as vision or hearing. More recently, a top-down interruption is considered to cause the disturbance of handling perceptual information.
Alien hand syndrome (AHS) or Dr. Strangelove syndrome is a category of conditions in which a person experiences their limbs acting seemingly on their own, without conscious control over the actions. There are a variety of clinical conditions that fall under this category, which most commonly affects the left hand. There are many similar terms for the various forms of the condition, but they are often used inappropriately. The affected person may sometimes reach for objects and manipulate them without wanting to do so, even to the point of having to use the controllable hand to restrain the alien hand. Under normal circumstances however, given that intent and action can be assumed to be deeply mutually entangled, the occurrence of alien hand syndrome can be usefully conceptualized as a phenomenon reflecting a functional "disentanglement" between thought and action.

Cognitive neuropsychology is a branch of cognitive psychology that aims to understand how the structure and function of the brain relates to specific psychological processes. Cognitive psychology is the science that looks at how mental processes are responsible for the cognitive abilities to store and produce new memories, produce language, recognize people and objects, as well as our ability to reason and problem solve. Cognitive neuropsychology places a particular emphasis on studying the cognitive effects of brain injury or neurological illness with a view to inferring models of normal cognitive functioning. Evidence is based on case studies of individual brain damaged patients who show deficits in brain areas and from patients who exhibit double dissociations. Double dissociations involve two patients and two tasks. One patient is impaired at one task but normal on the other, while the other patient is normal on the first task and impaired on the other. For example, patient A would be poor at reading printed words while still being normal at understanding spoken words, while the patient B would be normal at understanding written words and be poor at understanding spoken words. Scientists can interpret this information to explain how there is a single cognitive module for word comprehension. From studies like these, researchers infer that different areas of the brain are highly specialised. Cognitive neuropsychology can be distinguished from cognitive neuroscience, which is also interested in brain-damaged patients, but is particularly focused on uncovering the neural mechanisms underlying cognitive processes.

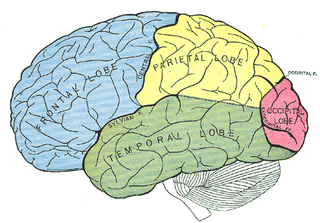
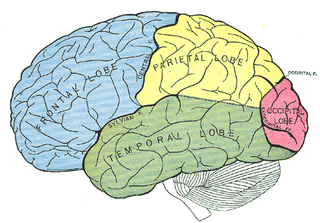
The parietal lobe is one of the four major lobes of the cerebral cortex in the brain of mammals. The parietal lobe is positioned above the temporal lobe and behind the frontal lobe and central sulcus.
Bálint's syndrome is an uncommon and incompletely understood triad of severe neuropsychological impairments: inability to perceive the visual field as a whole (simultanagnosia), difficulty in fixating the eyes, and inability to move the hand to a specific object by using vision. It was named in 1909 for the Austro-Hungarian neurologist and psychiatrist Rezső Bálint who first identified it.

In cognitive science and neuropsychology, executive functions are a set of cognitive processes that are necessary for the cognitive control of behavior: selecting and successfully monitoring behaviors that facilitate the attainment of chosen goals. Executive functions include basic cognitive processes such as attentional control, cognitive inhibition, inhibitory control, working memory, and cognitive flexibility. Higher-order executive functions require the simultaneous use of multiple basic executive functions and include planning and fluid intelligence.
Autotopagnosia from the Greek a and gnosis, meaning "without knowledge", topos meaning "place", and auto meaning "oneself", autotopagnosia virtually translates to the "lack of knowledge about one's own space," and is clinically described as such.
Hugo Karl Liepmann was a German neurologist and psychiatrist born in Berlin, into a Jewish family.
Ideomotor Apraxia, often IMA, is a neurological disorder characterized by the inability to correctly imitate hand gestures and voluntarily mime tool use, e.g. pretend to brush one's hair. The ability to spontaneously use tools, such as brushing one's hair in the morning without being instructed to do so, may remain intact, but is often lost. The general concept of apraxia and the classification of ideomotor apraxia were developed in Germany in the late 19th and early 20th centuries by the work of Hugo Liepmann, Adolph Kussmaul, Arnold Pick, Paul Flechsig, Hermann Munk, Carl Nothnagel, Theodor Meynert, and linguist Heymann Steinthal, among others. Ideomotor apraxia was classified as "ideo-kinetic apraxia" by Liepmann due to the apparent dissociation of the idea of the action with its execution. The classifications of the various subtypes are not well defined at present, however, owing to issues of diagnosis and pathophysiology. Ideomotor apraxia is hypothesized to result from a disruption of the system that relates stored tool use and gesture information with the state of the body to produce the proper motor output. This system is thought to be related to the areas of the brain most often seen to be damaged when ideomotor apraxia is present: the left parietal lobe and the premotor cortex. Little can be done at present to reverse the motor deficit seen in ideomotor apraxia, although the extent of dysfunction it induces is not entirely clear.
Body schema is an organism's internal model of its own body, including the position of its limbs. The neurologist Sir Henry Head originally defined it as a postural model of the body that actively organizes and modifies 'the impressions produced by incoming sensory impulses in such a way that the final sensation of body position, or of locality, rises into consciousness charged with a relation to something that has happened before'. As a postural model that keeps track of limb position, it plays an important role in control of action.
Deep dyslexia is a form of dyslexia that disrupts reading processes. Deep dyslexia may occur as a result of a head injury, stroke, disease, or operation. This injury results in the occurrence of semantic errors during reading and the impairment of nonword reading.
Apraxia of speech (AOS), also called verbal apraxia, is a speech sound disorder affecting an individual's ability to translate conscious speech plans into motor plans, which results in limited and difficult speech ability. By the definition of apraxia, AOS affects volitional movement pattern. However, AOS usually also affects automatic speech.
Constructional apraxia is a neurological disorder in which people are unable to perform tasks or movements even though they understand the task, are willing to complete it, and have the physical ability to perform the movements. It is characterized by an inability or difficulty to build, assemble, or draw objects. Constructional apraxia may be caused by lesions in the parietal lobe following stroke or it may serve as an indicator for Alzheimer's disease.
In psychology, confabulation is a memory error consisting of the production of fabricated, distorted, or misinterpreted memories about oneself or the world. It is generally associated with certain types of brain damage or a specific subset of dementias. While still an area of ongoing research, the basal forebrain is implicated in the phenomenon of confabulation. People who confabulate present with incorrect memories ranging from subtle inaccuracies to surreal fabrications, and may include confusion or distortion in the temporal framing of memories. In general, they are very confident about their recollections, even when challenged with contradictory evidence.
Executive functions are a cognitive apparatus that controls and manages cognitive processes. Norman and Shallice (1980) proposed a model on executive functioning of attentional control that specifies how thought and action schemata become activated or suppressed for routine and non-routine circumstances. Schemas, or scripts, specify an individual's series of actions or thoughts under the influence of environmental conditions. Every stimulus condition turns on the activation of a response or schema. The initiation of appropriate schema under routine, well-learned situations is monitored by contention scheduling which laterally inhibits competing schemas for the control of cognitive apparatus. Under unique, non-routine procedures controls schema activation. The SAS is an executive monitoring system that oversees and controls contention scheduling by influencing schema activation probabilities and allowing for general strategies to be applied to novel problems or situations during automatic attentional processes.
Body part as object (BPO) mime gestures occurs when an individual substitutes a part of their body - usually arms, fingers, or hands - to be part of an object they are miming. Miming uses representational gestures, meaning they are used to convey a message to others without the use of speech. A commonly used example of BPO miming is demonstrated by an individual using their finger to represent a toothbrush while acting out brushing their teeth.