Coronary artery bypass surgery, also known as coronary artery bypass graft, is a surgical procedure to treat coronary artery disease (CAD), the buildup of plaques in the arteries of the heart. It can relieve chest pain caused by CAD, slow the progression of CAD, and increase life expectancy. It aims to bypass narrowings in heart arteries by using arteries or veins harvested from other parts of the body, thus restoring adequate blood supply to the previously ischemic heart.

Gastric bypass surgery refers to a technique in which the stomach is divided into a small upper pouch and a much larger lower "remnant" pouch and then the small intestine is rearranged to connect to both. Surgeons have developed several different ways to reconnect the intestine, thus leading to several different gastric bypass procedures (GBP). Any GBP leads to a marked reduction in the functional volume of the stomach, accompanied by an altered physiological and physical response to food.

Steatotic liver disease (SLD) a.k.a. fatty liver disease (FLD) or hepatic steatosis, is a condition where excess fat builds up in the liver. Often there are no or few symptoms. Occasionally there may be tiredness or pain in the upper right side of the abdomen. Complications may include cirrhosis, liver cancer, and esophageal varices.

Vertical banded gastroplasty (VBG), also known as stomach stapling, is a form of bariatric surgery for weight control. The VBG procedure involves using a band and staples to create a small stomach pouch. In the bottom of the pouch is an approximate one-centimeter hole through which the pouch contents can flow into the remainder of the stomach and hence on to the remainder of the gastrointestinal tract.
The duodenal switch (DS) procedure, gastric reduction duodenal switch (GRDS), is a weight loss surgery procedure that is composed of a restrictive and a malabsorptive aspect.

A laparoscopic adjustable gastric band, commonly called a lap-band, A band, or LAGB, is an inflatable silicone device placed around the top portion of the stomach to treat obesity, intended to decrease food consumption.

Sleeve gastrectomy or vertical sleeve gastrectomy, is a surgical weight-loss procedure, typically performed laparoscopically, in which approximately 75 - 85% of the stomach is removed, along the greater curvature, which leaves a cylindrical, or "sleeve"-shaped stomach the size of a banana. Weight loss is affected not only through the reduction of the organ's size, but by the removal of the portion of it that produces ghrelin, the hormone that stimulates appetite. Patients can lose 50-70 percent of excess weight over the course of the two years that follow the surgery. The procedure is irreversible, though in some uncommon cases, patients can regain the lost weight, via resumption of poor dietary habits, or dilation of the stomach over time, which can require gastric sleeve revision surgery to either repair the sleeve or convert it to another type of weight loss method that may produce better results, such as a gastric bypass or duodenal switch.
Bariatric surgery is a medical term which describes a variety of procedures that are used to manage obesity and obesity-related conditions. Long term weight loss with bariatric surgery may achieved through alteration of gut hormones, physical reduction of stomach size, reduction of nutrient absorption, or a combination of these. Standard of care procedures include: Roux en-Y bypass, sleeve gastrectomy, and biliopancreatic diversion with duodenal switch, from which weight loss is largely achieved by altering gut hormone levels responsible for hunger and satiety, leading to a new hormonal weight set point. Bariatric surgery is the most effective treatment causing weight loss and reducing complications of obesity.

The American Society for Metabolic & Bariatric Surgery (ASMBS) is a non-profit medical organization dedicated to metabolic and bariatric surgery, and obesity-related diseases and conditions. It was established in 1983, and its stated vision is “to improve the public health and well being of society by lessening the burden of obesity and obesity-related diseases throughout the world.”
Copper deficiency, or hypocupremia, is defined either as insufficient copper to meet the needs of the body, or as a serum copper level below the normal range. Symptoms may include fatigue, decreased red blood cells, early greying of the hair, and neurological problems presenting as numbness, tingling, muscle weakness, and ataxia. The neurodegenerative syndrome of copper deficiency has been recognized for some time in ruminant animals, in which it is commonly known as "swayback". Copper deficiency can manifest in parallel with vitamin B12 and other nutritional deficiencies.
Jejunoileal bypass (JIB) was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel were detached and set to the side.

In general surgery, a Roux-en-Y anastomosis, or Roux-en-Y, is an end-to-side surgical anastomosis of bowel used to reconstruct the gastrointestinal tract. Typically, it is between stomach and small bowel that is distal from the cut end.
Revision weight loss surgery is a surgical procedure that is performed on patients who have already undergone a form of bariatric surgery, and have either had complications from such surgery or have not achieved significant weight loss results from the initial surgery. Procedures are usually performed laparoscopically, though open surgery may be required if prior bariatric surgery has resulted in extensive scarring.

SADI-S is a bariatric surgical technique to address metabolic disorders and to lose weight. It is a variation on the Duodenal Switch surgery, incorporating a vertical sleeve gastrectomy with a gastric bypass technique.
A duodenal-jejunal bypass liner, commonly called an EndoBarrier, is an implantable medical device in the form of a thin flexible 60 cm-long tube that creates a physical barrier between ingested food and the duodenum/proximal jejunum. The duodenal-jejunal bypass liner prevents the interaction of food with enzymes and hormones in the proximal intestine to treat type 2 diabetes and obesity. The duodenal-jejunal bypass liner is delivered endoscopically and has been tested on the morbidly obese as well as obese patients with a BMI less than 40, particularly those with difficult-to-manage type 2 diabetes. Despite a handful of serious adverse events such as gastrointestinal bleeding, abdominal pain, and device migration — all resolved with device removal — initial clinical trials have produced promising results in the treatment's ability to improve weight loss and glucose homeostasis outcomes.
I. Michael Leitman is an American surgeon and medical educator. He is Professor of Surgery and Medical Education and Dean for Graduate Medical Education at the Icahn School of Medicine at Mount Sinai. He previously held the position of Chairman of the Department of Surgery at Mount Sinai Beth Israel in New York City.
Jejunojejunostomy is a surgical technique used in an anastomosis between two portions of the jejunum. It is a type of bypass occurring in the intestine. It may lead to marked reduction in the functional volume of the intestine. This technique is also performed using Laparoscopic surgery. The surgical procedure can lead to complications including infections, hemorrhage, strictures, ulcers, intestinal obstruction, thromboembolism and malnutrition.
Intestinal bypass is a bariatric surgery performed on patients with morbid obesity to create an irreversible weight loss, when implementing harsh restrictions on the diets have failed. Jejunocolic anastomosis was firstly employed. Nonetheless, it led to some unexpected complications such as severe electrolyte imbalance and liver failure. It was then modified to jejunoileal techniques. Viewed as a novel form of treatment for obesity, many intestinal bypass operations were carried out in the 1960s and 1980s. Significant weight loss was observed in patients, but this surgery also resulted in several complications, for instance, nutritional deficiencies and metabolic problems. Due to the presence of surgical alternatives and anti-obesity medications, intestinal bypass is now rarely used.
Tom Pilkington was a professor of medicine at St. George's Hospital, London, who specialised in metabolic medicine. His work on jejuno-ileal bypass operations contributed to the development of the surgical management of severe obesity. He was mentor to Patrick Vallance and Peter Kopelman.
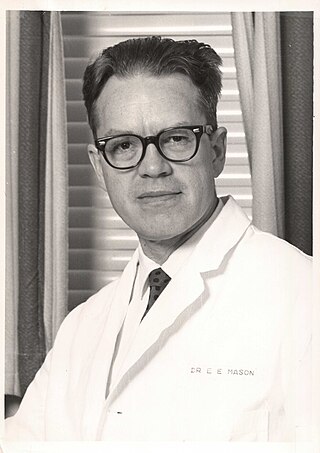
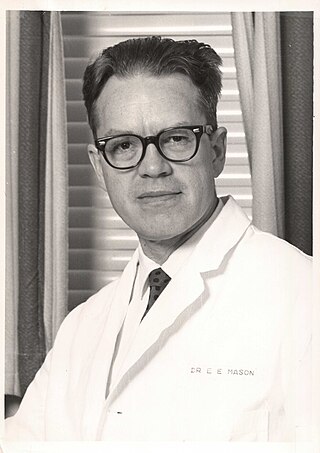
Edward Eaton Mason was an American surgeon, professor, and medical researcher who specialized in obesity surgery. He is known for developing restrictive gastric surgery for morbidly obese patients. Mason introduced the first gastric bypass surgery in 1966 and was the inventor of the first vertical banded gastroplasty surgery in 1980.