Related Research Articles
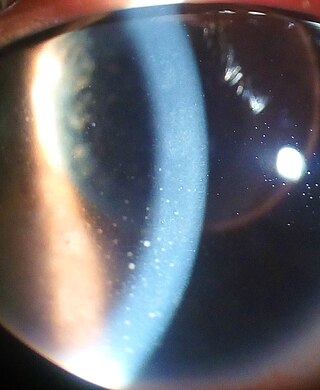
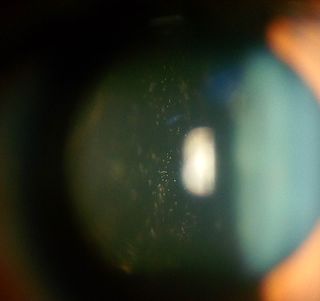
Uveitis is inflammation of the uvea, the pigmented layer of the eye between the inner retina and the outer fibrous layer composed of the sclera and cornea. The uvea consists of the middle layer of pigmented vascular structures of the eye and includes the iris, ciliary body, and choroid. Uveitis is described anatomically, by the part of the eye affected, as anterior, intermediate or posterior, or panuveitic if all parts are involved. Anterior uveitis (iridocyclitis) is the most common, with the incidence of uveitis overall affecting approximately 1:4500, most commonly those between the ages of 20-60. Symptoms include eye pain, eye redness, floaters and blurred vision, and ophthalmic examination may show dilated ciliary blood vessels and the presence of cells in the anterior chamber. Uveitis may arise spontaneously, have a genetic component, or be associated with an autoimmune disease or infection. While the eye is a relatively protected environment, its immune mechanisms may be overcome resulting in inflammation and tissue destruction associated with T-cell activation.
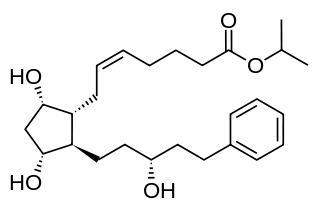
Latanoprost, sold under the brand name Xalatan among others, is a medication used to treat increased pressure inside the eye. This includes ocular hypertension and open angle glaucoma. It is applied as eye drops to the eyes. Onset of effects is usually within four hours, and they last for up to a day.
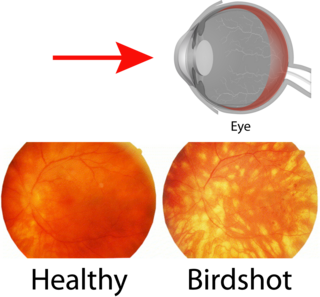
Birdshot chorioretinopathy, now commonly named birdshot uveitis or HLA-A29 uveitis, is a rare form of bilateral posterior uveitis affecting both eyes. It causes severe, progressive inflammation of both the choroid and retina.
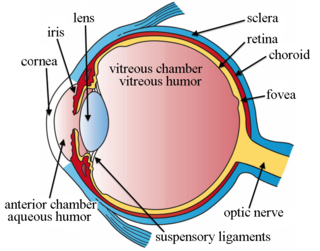
Intravitreal is a route of administration of a drug, or other substance, in which the substance is delivered into the vitreous humor of the eye. "Intravitreal" literally means "inside an eye". Intravitreal injections were first introduced in 1911 when Ohm gave an injection of air into the vitreous humor to repair a detached retina. In the mid-1940s, intravitreal injections became a standard way to administer drugs to treat endophthalmitis and cytomegalovirus retinitis.

Primary central nervous system lymphoma (PCNSL), also termed primary diffuse large B-cell lymphoma of the central nervous system (DLBCL-CNS), is a primary intracranial tumor appearing mostly in patients with severe immunodeficiency. It is a subtype and one of the most aggressive of the diffuse large B-cell lymphomas.
Intermediate uveitis is a form of uveitis localized to the vitreous and peripheral retina. Primary sites of inflammation include the vitreous of which other such entities as pars planitis, posterior cyclitis, and hyalitis are encompassed. Intermediate uveitis may either be an isolated eye disease or associated with the development of a systemic disease such as multiple sclerosis or sarcoidosis. As such, intermediate uveitis may be the first expression of a systemic condition. Infectious causes of intermediate uveitis include Epstein–Barr virus infection, Lyme disease, HTLV-1 virus infection, cat scratch disease, and hepatitis C.

Epiretinal membrane or macular pucker is a disease of the eye in response to changes in the vitreous humor or more rarely, diabetes. Sometimes, as a result of immune system response to protect the retina, cells converge in the macular area as the vitreous ages and pulls away in posterior vitreous detachment (PVD).

Intraocular hemorrhage is bleeding inside the eye. Bleeding can occur from any structure of the eye where there is vasculature or blood flow, including the anterior chamber, vitreous cavity, retina, choroid, suprachoroidal space, or optic disc.
Proliferative vitreoretinopathy (PVR) is a disease that develops as a complication of rhegmatogenous retinal detachment. PVR occurs in about 8–10% of patients undergoing primary retinal detachment surgery and prevents the successful surgical repair of rhegmatogenous retinal detachment. PVR can be treated with surgery to reattach the detached retina but the visual outcome of the surgery is very poor. A number of studies have explored various possible adjunctive agents for the prevention and treatment of PVR, such as methotrexate, although none have yet been licensed for clinical use.

Orbital lymphoma is a common type of non-Hodgkin lymphoma that occurs near or on the eye. Common symptoms include decreased vision and uveitis. Orbital lymphoma can be diagnosed via a biopsy of the eye and is usually treated with radiotherapy or in combination with chemotherapy.

Toxoplasma chorioretinitis, more simply known as ocular toxoplasmosis, is possibly the most common cause of infections in the back of the eye worldwide. The causitive agent is Toxoplasma gondii, and in the United States, most cases are acquired congenitally. The most common symptom is decreased visual acuity in one eye. The diagnosis is made by examination of the eye, using ophthalmoscopy. Sometimes serologic testing is used to rule out the disease, but due to high rates of false positives, serologies are not diagnostic of toxoplasmic retinitis.
Multiple evanescent white dot syndrome (MEWDS) is an uncommon inflammatory condition of the retina that typically affects otherwise healthy young females in the second to fourth decades of life.

Serpiginous choroiditis, also known as geographic helicoid peripapillary choroidopathy (GHPC), is a rare, chronic, progressive, and recurrent bilateral inflammatory disease involving the retinal pigment epithelium (RPE), the choriocapillaries, and the choroid. It affects adult men and women equally in the second to seventh decades of life.
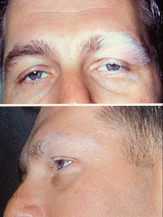
Vogt–Koyanagi–Harada disease (VKH) is a multisystem disease of presumed autoimmune cause that affects melanin-pigmented tissues. The most significant manifestation is bilateral, diffuse uveitis, which affects the eyes. VKH may variably also involve the inner ear, with effects on hearing, the skin, and the meninges of the central nervous system.
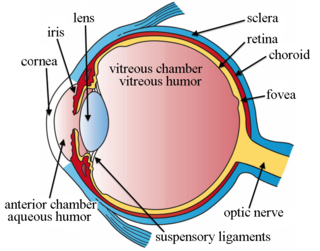
Intravitreal injection is the method of administration of drugs into the eye by injection with a fine needle. The medication will be directly applied into the vitreous humor. It is used to treat various eye diseases, such as age-related macular degeneration (AMD), diabetic retinopathy, and infections inside the eye such as endophthalmitis. As compared to topical administration, this method is beneficial for a more localized delivery of medications to the targeted site, as the needle can directly pass through the anatomical eye barrier and dynamic barrier. It could also minimize adverse drug effects on other body tissues via the systemic circulation, which could be a possible risk for intravenous injection of medications. Although there are risks of infections or other complications, with suitable precautions throughout the injection process, chances for these complications could be lowered.
Sickle cell retinopathy can be defined as retinal changes due to blood vessel damage in the eye of a person with a background of sickle cell disease. It can likely progress to loss of vision in late stages due to vitreous hemorrhage or retinal detachment. Sickle cell disease is a structural red blood cell disorder leading to consequences in multiple systems. It is characterized by chronic red blood cell destruction, vascular injury, and tissue ischemia causing damage to the brain, eyes, heart, lungs, kidneys, spleen, and musculoskeletal system.

Secondary glaucoma is a collection of progressive optic nerve disorders associated with a rise in intraocular pressure (IOP) which results in the loss of vision. In clinical settings, it is defined as the occurrence of IOP above 21 mmHg requiring the prescription of IOP-managing drugs. It can be broadly divided into two subtypes: secondary open-angle glaucoma and secondary angle-closure glaucoma, depending on the closure of the angle between the cornea and the iris. Principal causes of secondary glaucoma include optic nerve trauma or damage, eye disease, surgery, neovascularization, tumours and use of steroid and sulfa drugs. Risk factors for secondary glaucoma include uveitis, cataract surgery and also intraocular tumours. Common treatments are designed according to the type and the underlying causative condition, in addition to the consequent rise in IOP. These include drug therapy, the use of miotics, surgery or laser therapy.
Schwartz–Matsuo syndrome is a human eye disease characterised by rhegmatogenous retinal detachment, elevated intraocular pressure (IOP) and open angle of anterior chamber.

Uveitic glaucoma is most commonly a progression stage of noninfectious anterior uveitis or iritis.
Panuveitis also known as Diffuse uveitis or Total uveitis is an eye disease affecting the internal structures of the eye. In this inflammation occurs throughout the uveal tract, with no specific areas of predominant inflammation. In most cases, along with the uvea, the retina, vitreous humor, optic nerve or lens are also involved.
References
- ↑ Shen, DF; Herbort, CP; Tuaillon, N; Buggage, RR; Egwuagu, CE; Chan, CC (Oct 2001). "Detection of Toxoplasma gondii DNA in primary intraocular B-cell lymphoma". Modern Pathology. 14 (10): 995–9. doi: 10.1038/modpathol.3880424 . PMID 11598169.
- ↑ Cassoux, N; Merle-Beral, H; Leblond, V; Bodaghi, B; Miléa, D; Gerber, S; Fardeau, C; Reux, I; Xuan, KH; Chan, CC; LeHoang, P (Dec 2000). "Ocular and central nervous system lymphoma: clinical features and diagnosis". Ocular Immunology and Inflammation. 8 (4): 243–50. doi:10.1076/ocii.8.4.243.6463. PMID 11262654. S2CID 39345449.
- ↑ Shen, DF; Zhuang, Z; LeHoang, P; Böni, R; Zheng, S; Nussenblatt, RB; Chan, CC (Sep 1998). "Utility of microdissection and polymerase chain reaction for the detection of immunoglobulin gene rearrangement and translocation in primary intraocular lymphoma". Ophthalmology. 105 (9): 1664–9. doi: 10.1016/S0161-6420(98)99036-4 . PMID 9754175.
- ↑ Coupland, Sarah E.; Anastassiou, Gerasimos; Bornfeld, Norbert; Hummel, Michael; Stein, Harald (March 2005). "Primary intraocular lymphoma of T-cell type: report of a case and review of the literature". Graefe's Archive for Clinical and Experimental Ophthalmology. 243 (3): 189–197. doi:10.1007/s00417-004-0890-2. PMID 15806372. S2CID 24772799.
- ↑ Gonzales, John A.; Chan, Chi-Chao (August 2007). "Biopsy techniques and yields in diagnosing primary intraocular lymphoma". International Ophthalmology. 27 (4): 241–250. doi:10.1007/s10792-007-9065-6. PMC 2048742 . PMID 17440686.
- ↑ Anthony, Casey L.; Bavinger, J. Clay; Shantha, Jessica G.; O’Keefe, Ghazala D.; Pearce, William A.; Voloschin, Alfredo; Grossniklaus, Hans E.; Yeh, Steven (2021-12-04). "Clinical outcomes following intravitreal methotrexate for primary vitreoretinal lymphoma". International Journal of Retina and Vitreous. 7 (1): 72. doi:10.1186/s40942-021-00346-0. ISSN 2056-9920. PMC 8645085 . PMID 34863313.