An aura is a perceptual disturbance experienced by some with epilepsy or migraine. An epileptic aura is a seizure.

In the field of neurology, temporal lobe epilepsy is an enduring brain disorder that causes unprovoked seizures from the temporal lobe. Temporal lobe epilepsy is the most common type of focal onset epilepsy among adults. Seizure symptoms and behavior distinguish seizures arising from the medial temporal lobe from seizures arising from the lateral (neocortical) temporal lobe. Memory and psychiatric comorbidities may occur. Diagnosis relies on electroencephalographic (EEG) and neuroimaging studies. Anticonvulsant medications, epilepsy surgery and dietary treatments may improve seizure control.
Anterior temporal lobectomy is the complete or partial removal of the anterior portion of the temporal lobe of the brain. The exact boundaries for removal can vary slightly in practice and between neurosurgeons. It is a treatment option for temporal lobe epilepsy for those in whom anticonvulsant medications do not control epileptic seizures, and who have frequent seizures, and who additionally qualify based on a WADA test to localize the dominant hemisphere for language module.
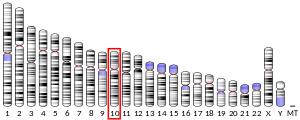
Glucose transporter 1, also known as solute carrier family 2, facilitated glucose transporter member 1 (SLC2A1), is a uniporter protein that in humans is encoded by the SLC2A1 gene. GLUT1 facilitates the transport of glucose across the plasma membranes of mammalian cells. This gene encodes a facilitative glucose transporter that is highly expressed in erythrocytes and endothelial cells, including cells of the blood–brain barrier. The encoded protein is found primarily in the cell membrane and on the cell surface, where it can also function as a receptor for human T-cell leukemia virus (HTLV) I and II. GLUT1 accounts for 2 percent of the protein in the plasma membrane of erythrocytes. Mutations in this gene can cause GLUT1 deficiency syndrome 1, GLUT1 deficiency syndrome 2, idiopathic generalized epilepsy 12, dystonia 9, and stomatin-deficient cryohydrocytosis.
Generalized epilepsy with febrile seizures plus (GEFS+) is a syndromic autosomal dominant disorder where affected individuals can exhibit numerous epilepsy phenotypes. GEFS+ can persist beyond early childhood. GEFS+ is also now believed to encompass three other epilepsy disorders: severe myoclonic epilepsy of infancy (SMEI), which is also known as Dravet's syndrome, borderline SMEI (SMEB), and intractable epilepsy of childhood (IEC). There are at least six types of GEFS+, delineated by their causative gene. Known causative gene mutations are in the sodium channel α subunit genes SCN1A, an associated β subunit SCN1B, and in a GABAA receptor γ subunit gene, in GABRG2 and there is another gene related with calcium channel the PCDH19 which is also known as Epilepsy Female with Mental Retardation. Penetrance for this disorder is estimated at 60%.
Benign familial neonatal seizures (BFNS), formerly called benign familial neonatal convulsions (BFNC), is a rare autosomal dominant inherited form of seizures. It manifests in newborns, normally within the first 7 days of life, as tonic–clonic seizures. Infants are otherwise normal between attacks and develop without incident. Attacks normally spontaneously cease within the first 15 weeks of life. Lifetime susceptibility to seizures is increased, as 16% of those diagnosed with BFNE earlier in life will go on to have seizures versus a 2% lifetime risk for the general population. There are three known genetic causes of BFNE, two being the voltage-gated potassium channels KCNQ2 (BFNC1) and KCNQ3 (BFNC2) and the third being a chromosomal inversion (BFNC3). There is no obvious correlation between most of the known mutations and clinical variability seen in BFNE.
Juvenile myoclonic epilepsy (JME), also known as Janz syndrome, is a form of genetic generalized epilepsy, representing 5–10% of all epilepsy cases. Typically it first presents between the ages of 12 and 18 with myoclonic seizures. These events typically occur after awakening from sleep, during the evening or when sleep deprived. JME is also characterized by generalized tonic–clonic seizures, and a minority of patients have absence seizures. The genetics of JME are complex and rapidly evolving as over 20 chromosomal loci and multiple genes have been identified. Given the genetic and clinical heterogeneity of JME some authors have suggested that it should be thought of as a spectrum disorder.
Autosomal dominant nocturnal frontal lobe epilepsy is an epileptic disorder that causes frequent violent seizures during sleep. These seizures often involve complex motor movements, such as hand clenching, arm raising/lowering, and knee bending. Vocalizations such as shouting, moaning, or crying are also common. ADNFLE is often misdiagnosed as nightmares. Attacks often occur in clusters and typically first manifest in childhood. There are four known loci for ADNFLE, three with known causative genes. These genes, CHRNA4, CHRNB2, and CHRNA2, encode various nicotinic acetylcholine receptor α and β subunits.
Progressive Myoclonic Epilepsies (PME) are a rare group of inherited neurodegenerative diseases characterized by myoclonus, resistance to treatment, and neurological deterioration. The cause of PME depends largely on the type of PME. Most PMEs are caused by autosomal dominant or recessive and mitochondrial mutations. The location of the mutation also affects the inheritance and treatment of PME. Diagnosing PME is difficult due to their genetic heterogeneity and the lack of a genetic mutation identified in some patients. The prognosis depends largely on the worsening symptoms and failure to respond to treatment. There is no current cure for PME and treatment focuses on managing myoclonus and seizures through antiepileptic medication (AED).

Sodium channel protein type 1 subunit alpha (SCN1A), is a protein which in humans is encoded by the SCN1A gene.

Disintegrin and metalloproteinase domain-containing protein 22 also known as ADAM22 is an enzyme that in humans is encoded by the ADAM22 gene.
Sleep-related hypermotor epilepsy (SHE), previously known as nocturnal frontal lobe epilepsy, is a form of focal epilepsy characterized by seizures which arise during sleep. The seizures are most typically characterized by complex motor behaviors. It is a relatively uncommon form of epilepsy that constitutes approximately 9-13% of cases. This disorder is associated with cognitive impairment in at least half of patients as well as excessive daytime sleepiness due to poor sleep quality. This disorder is sometimes misdiagnosed as a non-epileptic sleep disorder. There are many potential causes of SHE including genetic, acquired injuries and structural abnormalities.
Megalencephalic leukoencephalopathy with subcortical cysts is a form of hereditary CNS demyelinating disease. It belongs to a group of disorders called leukodystrophies. It is characterized by early-onset enlargement of the head (macrocephaly) as well as delayed-onset neurological deterioration to include spasticity, epilepsy, and lack of muscular coordination. MLC does not appear to be a disease that is fatal at birth or early in life despite its symptoms, although the number of patients throughout history known to have the disease is fairly limited.

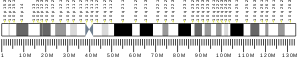
Northern epilepsy syndrome (NE), or progressive epilepsy with mental retardation (EPMR), is a subtype of neuronal ceroid lipofuscinosis and a rare disease that is regarded as a Finnish heritage disease. Unlike most Finnish heritage diseases, this syndrome has been reported only in Finland. The disease is characterized by seizures in early childhood that progressively get worse until after puberty. Once the onset of seizures occurs, mental degradation is seen. This continues into adulthood, even after seizure frequency has decreased. The cause of the disease is a missense mutation on chromosome 8. The creation of a new protein occurs, and the lipid content of the brain is altered because of it. The ratio of the mutation carriers is 1:135. There is nothing that has been found to stop the progression of the disease, but symptomatic approaches, such as the use of benzodiazepines, have helped control seizures.
Vertiginous epilepsy is infrequently the first symptom of a seizure, characterized by a feeling of vertigo. When it occurs, there is a sensation of rotation or movement that lasts for a few seconds before full seizure activity. While the specific causes of this disease are speculative there are several methods for diagnosis, the most important being the patient's recall of episodes. Most times, those diagnosed with vertiginous seizures are left to self-manage their symptoms or are able to use anti-epileptic medication to dampen the severity of their symptoms.
People with epilepsy may be classified into different syndromes based on specific clinical features. These features include the age at which seizures begin, the seizure types, and EEG findings, among others. Identifying an epilepsy syndrome is useful as it helps determine the underlying causes as well as deciding what anti-seizure medication should be tried. Epilepsy syndromes are more commonly diagnosed in infants and children. Some examples of epilepsy syndromes include benign rolandic epilepsy, childhood absence epilepsy and juvenile myoclonic epilepsy. Severe syndromes with diffuse brain dysfunction caused, at least partly, by some aspect of epilepsy, are also referred to as epileptic encephalopathies. These are associated with frequent seizures that are resistant to treatment and severe cognitive dysfunction, for instance Lennox-Gastaut syndrome and West syndrome.
Anti-VGKC-complex encephalitis are caused by antibodies against the voltage gated potassium channel-complex (VGKC-complex) and are implicated in several autoimmune conditions including limbic encephalitis, epilepsy and neuromyotonia.

Solute carrier family 25 member 22 is a protein that in humans is encoded by the SLC25A22 gene. This gene encodes a mitochondrial glutamate carrier. Mutations in this gene are associated with early infantile epileptic encephalopathy. Expression of this gene is increased in colorectal tumor cells.
Autosomal dominant partial epilepsy with auditory features syndrome is a rare, relatively benign, hereditary epileptic disorder that is characterized by seizures, seizure-associated hearing alterations and receptive aphasia. Unlike other genetic disorders, this one does not affect intellect.
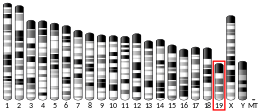
PRICKLE1-related progressive myoclonus epilepsy with ataxia is a very rare genetic disorder which is characterized by myoclonic epilepsy and ataxia.