A head injury is any injury that results in trauma to the skull or brain. The terms traumatic brain injury and head injury are often used interchangeably in the medical literature. Because head injuries cover such a broad scope of injuries, there are many causes—including accidents, falls, physical assault, or traffic accidents—that can cause head injuries.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, coma and death.

Shaken baby syndrome (SBS), also known as abusive head trauma (AHT), is the leading cause of fatal head injuries in children younger than two years. Diagnosing the syndrome has proved both challenging and contentious for medical professionals, in that objective witnesses to the initial trauma are generally unavailable. This is said to be particularly problematic when the trauma is deemed 'non accidental'. Some medical professionals propose that SBS is the result of respiratory abnormalities leading to hypoxia and swelling of the brain The courtroom has become a forum for conflicting theories with which generally accepted medical literature has not been reconciled. Often there are no outwardly visible signs of trauma, despite the presence of severe internal brain and eye. Complications include seizures, visual impairment, cerebral palsy, cognitive impairment, and death.

Intracranial pressure (ICP) is the pressure exerted by fluids such as cerebrospinal fluid (CSF) inside the skull and on the brain tissue. ICP is measured in millimeters of mercury (mmHg) and at rest, is normally 7–15 mmHg for a supine adult. The body has various mechanisms by which it keeps the ICP stable, with CSF pressures varying by about 1 mmHg in normal adults through shifts in production and absorption of CSF.

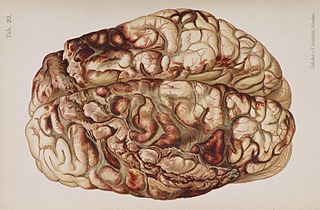
A subdural hematoma (SDH) is a type of bleeding in which a collection of blood—usually but not always associated with a traumatic brain injury—gathers between the inner layer of the dura mater and the arachnoid mater of the meninges surrounding the brain. It usually results from tears in bridging veins that cross the subdural space.

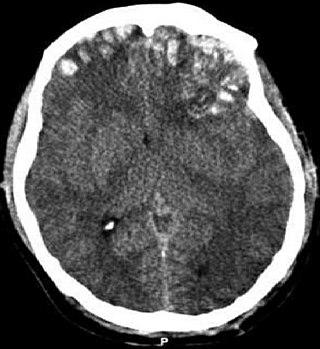
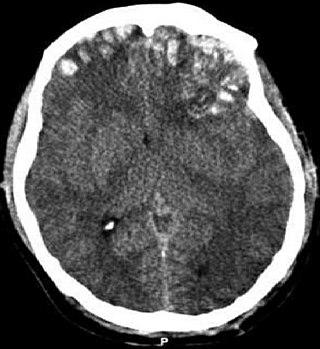
Intracranial hemorrhage (ICH), also known as intracranial bleed, is bleeding within the skull. Subtypes are intracerebral bleeds, subarachnoid bleeds, epidural bleeds, and subdural bleeds. More often than not it ends in a lethal outcome.

Epidural hematoma is when bleeding occurs between the tough outer membrane covering the brain and the skull. Often there is loss of consciousness following a head injury, a brief regaining of consciousness, and then loss of consciousness again. Other symptoms may include headache, confusion, vomiting, and an inability to move parts of the body. Complications may include seizures.
A traumatic brain injury (TBI), also known as an intracranial injury, is an injury to the brain caused by an external force. TBI can be classified based on severity, mechanism, or other features. Head injury is a broader category that may involve damage to other structures such as the scalp and skull. TBI can result in physical, cognitive, social, emotional and behavioral symptoms, and outcomes can range from complete recovery to permanent disability or death.
A penetrating head injury, or open head injury, is a head injury in which the dura mater, the outer layer of the meninges, is breached. Penetrating injury can be caused by high-velocity projectiles or objects of lower velocity such as knives, or bone fragments from a skull fracture that are driven into the brain. Head injuries caused by penetrating trauma are serious medical emergencies and may cause permanent disability or death.

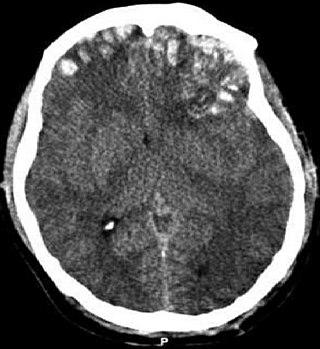
Intracerebral hemorrhage (ICH), also known as cerebral bleed, intraparenchymal bleed, and haemorrhagic stroke, is a sudden bleeding into the tissues of the brain, into its ventricles, or into both. An ICH is one kind of bleeding within the skull and one kind of stroke. Symptoms can include headache, one-sided weakness, vomiting, seizures, decreased level of consciousness, and neck stiffness. Often, symptoms get worse over time. Fever is also common.
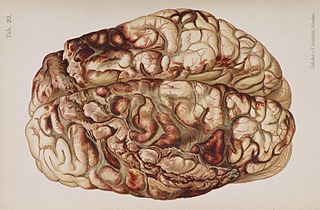
Cerebral contusion, Latin contusio cerebri, a form of traumatic brain injury, is a bruise of the brain tissue. Like bruises in other tissues, cerebral contusion can be associated with multiple microhemorrhages, small blood vessel leaks into brain tissue. Contusion occurs in 20–30% of severe head injuries. A cerebral laceration is a similar injury except that, according to their respective definitions, the pia-arachnoid membranes are torn over the site of injury in laceration and are not torn in contusion. The injury can cause a decline in mental function in the long term and in the emergency setting may result in brain herniation, a life-threatening condition in which parts of the brain are squeezed past parts of the skull. Thus treatment aims to prevent dangerous rises in intracranial pressure, the pressure within the skull.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, is physical traumas, and particularly in the elderly who fall. It is contrasted with penetrating trauma which occurs when an object pierces the skin and enters a tissue of the body, creating an open wound and bruise.

A subdural hygroma (SDG) is a collection of cerebrospinal fluid (CSF), without blood, located under the dural membrane of the brain. Most subdural hygromas are believed to be derived from chronic subdural hematomas. They are commonly seen in elderly people after minor trauma but can also be seen in children following infection or trauma. One of the common causes of subdural hygroma is a sudden decrease in pressure as a result of placing a ventricular shunt. This can lead to leakage of CSF into the subdural space especially in cases with moderate to severe brain atrophy. In these cases the symptoms such as mild fever, headache, drowsiness and confusion can be seen, which are relieved by draining this subdural fluid.
In medicine, a mass effect is the effect of a growing mass that results in secondary pathological effects by pushing on or displacing surrounding tissue.

The cave of septum pellucidum (CSP), cavum septi pellucidi, or cavity of septum pellucidum is a slit-like space in the septum pellucidum that is present in fetuses but usually fuses during infancy. The septum pellucidum is a thin, laminated translucent vertical membrane in the midline of the brain separating the anterior horns of the right and left ventricles. It lies posterior to the corpus callosum. Persistence of the cave of septum pellucidum after infancy has been loosely associated with neural maldevelopment and several mental disorders that correlate with decreased brain tissue.
Kernohan's notch is a cerebral peduncle indentation associated with some forms of transtentorial herniation. It is a secondary condition caused by a primary injury on the opposite hemisphere of the brain. Kernohan's notch is an ipsilateral condition, in that a left-sided primary lesion evokes motor impairment in the left side of the body and a right-sided primary injury evokes motor impairment in the right side of the body. The seriousness of Kernohan's notch varies depending on the primary problem causing it, which may range from benign brain tumors to advanced subdural hematoma.
The monitoring of intracranial pressure (ICP) is used in the treatment of a number of neurological conditions ranging from severe traumatic brain injury to stroke and brain bleeds. This process is called intracranial pressure monitoring. Monitoring is important as persistent increases in ICP is associated with worse prognosis in brain injuries due to decreased oxygen delivery to the injured area and risk of brain herniation.
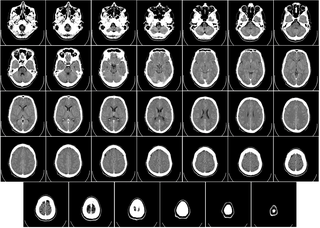
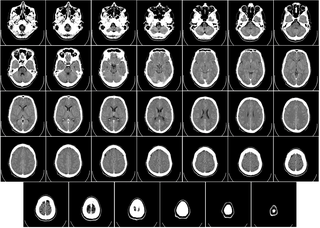
Computed tomography of the head uses a series of X-rays in a CT scan of the head taken from many different directions; the resulting data is transformed into a series of cross sections of the brain using a computer program. CT images of the head are used to investigate and diagnose brain injuries and other neurological conditions, as well as other conditions involving the skull or sinuses; it used to guide some brain surgery procedures as well. CT scans expose the person getting them to ionizing radiation which has a risk of eventually causing cancer; some people have allergic reactions to contrast agents that are used in some CT procedures.
A sports-related traumatic brain injury is a serious accident which may lead to significant morbidity or mortality. Traumatic brain injury (TBI) in sports are usually a result of physical contact with another person or stationary object, These sports may include boxing, gridiron football, field/ice hockey, lacrosse, martial arts, rugby, soccer, wrestling, auto racing, cycling, equestrian, rollerblading, skateboarding, skiing or snowboarding.
Clinicians routinely check the pupils of critically injured and ill patients to monitor neurological status. However, manual pupil measurements have been shown to be subjective, inaccurate, and not repeatable or consistent. Automated assessment of the pupillary light reflex has emerged as an objective means of measuring pupillary reactivity across a range of neurological diseases, including stroke, traumatic brain injury and edema, tumoral herniation syndromes, and sports or war injuries. Automated pupillometers are used to assess an array of objective pupillary variables including size, constriction velocity, latency, and dilation velocity, which are normalized and standardized to compute an indexed score such as the Neurological Pupil index (NPi).