Heating, ventilation, and air conditioning (HVAC) is the use of various technologies to control the temperature, humidity, and purity of the air in an enclosed space. Its goal is to provide thermal comfort and acceptable indoor air quality. HVAC system design is a subdiscipline of mechanical engineering, based on the principles of thermodynamics, fluid mechanics, and heat transfer. "Refrigeration" is sometimes added to the field's abbreviation as HVAC&R or HVACR, or "ventilation" is dropped, as in HACR.

A cleanroom or clean room is an engineered space, which maintains a very low concentration of airborne particulates. It is well isolated, well-controlled from contamination, and actively cleansed. Such rooms are commonly needed for scientific research, and in industrial production for all nanoscale processes, such as semiconductor manufacturing. A cleanroom is designed to keep everything from dust, to airborne organisms, or vaporised particles, away from it, and so from whatever material is being handled inside it.

Mechanical ventilation, assisted ventilation or intermittent mandatory ventilation (IMV) is the medical term for using a machine called a ventilator to fully or partially provide artificial ventilation. Mechanical ventilation helps move air into and out of the lungs, with the main goal of helping the delivery of oxygen and removal of carbon dioxide. Mechanical ventilation is used for many reasons, including to protect the airway due to mechanical or neurologic cause, to ensure adequate oxygenation, or to remove excess carbon dioxide from the lungs. Various healthcare providers are involved with the use of mechanical ventilation and people who require ventilators are typically monitored in an intensive care unit.

An operating theater is a facility within a hospital where surgical operations are carried out in an aseptic environment.

Ventilation is the intentional introduction of outdoor air into a space. Ventilation is mainly used to control indoor air quality by diluting and displacing indoor pollutants; it can also be used to control indoor temperature, humidity, and air motion to benefit thermal comfort, satisfaction with other aspects of the indoor environment, or other objectives.
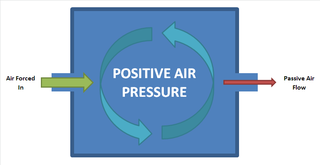
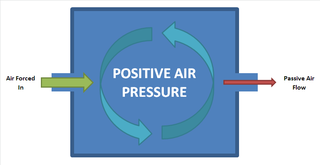
Positive pressure is a pressure within a system that is greater than the environment that surrounds that system. Consequently, if there is any leak from the positively pressured system, it will egress into the surrounding environment. This is in contrast to a negative pressure room, where air is sucked in.

A hospital-acquired infection, also known as a nosocomial infection, is an infection that is acquired in a hospital or other healthcare facility. To emphasize both hospital and nonhospital settings, it is sometimes instead called a healthcare-associated infection. Such an infection can be acquired in hospital, nursing home, rehabilitation facility, outpatient clinic, diagnostic laboratory or other clinical settings. A number of dynamic processes can bring contamination into operating rooms and other areas within nosocomial settings. Infection is spread to the susceptible patient in the clinical setting by various means. Healthcare staff also spread infection, in addition to contaminated equipment, bed linens, or air droplets. The infection can originate from the outside environment, another infected patient, staff that may be infected, or in some cases, the source of the infection cannot be determined. In some cases the microorganism originates from the patient's own skin microbiota, becoming opportunistic after surgery or other procedures that compromise the protective skin barrier. Though the patient may have contracted the infection from their own skin, the infection is still considered nosocomial since it develops in the health care setting. Nosocomial infection tends to lack evidence that it was present when the patient entered the healthcare setting, thus meaning it was acquired post-admission.

A bag valve mask (BVM), sometimes known by the proprietary name Ambu bag or generically as a manual resuscitator or "self-inflating bag", is a hand-held device commonly used to provide positive pressure ventilation to patients who are not breathing or not breathing adequately. The device is a required part of resuscitation kits for trained professionals in out-of-hospital settings (such as ambulance crews) and is also frequently used in hospitals as part of standard equipment found on a crash cart, in emergency rooms or other critical care settings. Underscoring the frequency and prominence of BVM use in the United States, the American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiac Care recommend that "all healthcare providers should be familiar with the use of the bag-mask device." Manual resuscitators are also used within the hospital for temporary ventilation of patients dependent on mechanical ventilators when the mechanical ventilator needs to be examined for possible malfunction or when ventilator-dependent patients are transported within the hospital. Two principal types of manual resuscitators exist; one version is self-filling with air, although additional oxygen (O2) can be added but is not necessary for the device to function. The other principal type of manual resuscitator (flow-inflation) is heavily used in non-emergency applications in the operating room to ventilate patients during anesthesia induction and recovery.
Infection prevention and control is the discipline concerned with preventing healthcare-associated infections; a practical rather than academic sub-discipline of epidemiology. In Northern Europe, infection prevention and control is expanded from healthcare into a component in public health, known as "infection protection". It is an essential part of the infrastructure of health care. Infection control and hospital epidemiology are akin to public health practice, practiced within the confines of a particular health-care delivery system rather than directed at society as a whole.

Continuous positive airway pressure (CPAP) is a form of positive airway pressure (PAP) ventilation in which a constant level of pressure greater than atmospheric pressure is continuously applied to the upper respiratory tract of a person. The application of positive pressure may be intended to prevent upper airway collapse, as occurs in obstructive sleep apnea, or to reduce the work of breathing in conditions such as acute decompensated heart failure. CPAP therapy is highly effective for managing obstructive sleep apnea. Compliance and acceptance of use of CPAP therapy can be a limiting factor, with 8% of people stopping use after the first night and 50% within the first year.
Infiltration is the unintentional or accidental introduction of outside air into a building, typically through cracks in the building envelope and through use of doors for passage. Infiltration is sometimes called air leakage. The leakage of room air out of a building, intentionally or not, is called exfiltration. Infiltration is caused by wind, negative pressurization of the building, and by air buoyancy forces known commonly as the stack effect.
Barrier isolator is a general term that includes two types of devices: isolators and restricted access barriers (RABS). Both are devices that provide a physical and aerodynamic barrier between the external clean room environment and a work process. The isolator design is the more dependable of the two barrier design choices, as it prevents contamination hazards by achieving a more comprehensive separation of the processing environment from the surrounding facility. Nonetheless, both Isolator and RABS designs are contemporary approaches developed over the last 35 years and a great advancement over designs of the 1950s-70s that were far more prone to microbial contamination problems.
Aerobiological engineering is the science of designing buildings and systems to control airborne pathogens and allergens in indoor environments. The most-common environments include commercial buildings, residences and hospitals. This field of study is important because controlled indoor climates generally tend to favor the survival and transmission of contagious human pathogens as well as certain kinds of fungi and bacteria.

In health care facilities, isolation represents one of several measures that can be taken to implement in infection control: the prevention of communicable diseases from being transmitted from a patient to other patients, health care workers, and visitors, or from outsiders to a particular patient. Various forms of isolation exist, in some of which contact procedures are modified, and others in which the patient is kept away from all other people. In a system devised, and periodically revised, by the U.S. Centers for Disease Control and Prevention (CDC), various levels of patient isolation comprise application of one or more formally described "precaution".

A positive pressure enclosure, also known as a welding habitat or hot work habitat, is a chamber used to provide a safe working environment for performing hot work in the presence of explosive gases or vapors. They are commonly used in welding environments and are associated with the offshore oil industry.
Transmission-based precautions are infection-control precautions in health care, in addition to the so-called "standard precautions". They are the latest routine infection prevention and control practices applied for patients who are known or suspected to be infected or colonized with infectious agents, including certain epidemiologically important pathogens, which require additional control measures to effectively prevent transmission. Universal precautions are also important to address as far as transmission-based precautions. Universal precautions is the practice of treating all bodily fluids as if it is infected with HIV, HBV, or other blood borne pathogens.

On a ship, the fire room, or FR or boiler room or stokehold, referred to the space, or spaces, of a vessel where water was brought to a boil. The steam was then transmitted to a separate engine room, often located immediately aft, where it was utilized to power the vessel. To increase the safety and damage survivability of a vessel, the machinery necessary for operations may be segregated into various spaces, the fire room was one of these spaces, and was among the largest physical compartment of the machinery space. On some ships, the space comprised more than one fire room, such as forward and aft, or port or starboard fire rooms, or may be simply numbered. Each room was connected to a flue, exhausting into a stack ventilating smoke.

The Aeromedical Biological Containment System (ABCS) is an aeromedical evacuation capability devised by the U.S. Centers for Disease Control and Prevention (CDC) in collaboration with the U.S. Department of Defense (DoD) and government contractor Phoenix Air between 2007 and 2010. Its purpose is to safely air-transport a highly contagious patient; it comprises a transit isolator and an appropriately configured supporting aircraft. Originally developed to support CDC staff who might become infected while investigating avian flu and SARS in East Asia, it was never used until the 2014 Ebola virus epidemic in West Africa, transporting 36 Ebola patients out of West Africa.
Engineering controls are strategies designed to protect workers from hazardous conditions by placing a barrier between the worker and the hazard or by removing a hazardous substance through air ventilation. Engineering controls involve a physical change to the workplace itself, rather than relying on workers' behavior or requiring workers to wear protective clothing.

Engineering controls for nanomaterials are a set of hazard control methods and equipment for workers who interact with nanomaterials. Engineering controls are physical changes to the workplace that isolate workers from hazards, and are considered the most important set of methods for controlling the health and safety hazards of nanomaterials after systems and facilities have been designed.