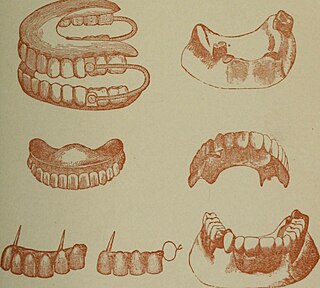
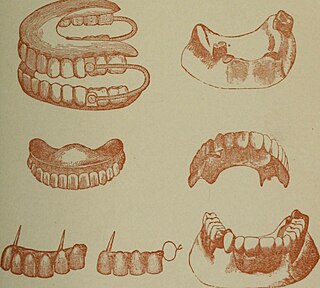
Dentures are prosthetic devices constructed to replace missing teeth, supported by the surrounding soft and hard tissues of the oral cavity. Conventional dentures are removable. However, there are many denture designs, some of which rely on bonding or clasping onto teeth or dental implants. There are two main categories of dentures, the distinction being whether they fit onto the mandibular arch or on the maxillary arch.

Dental surgery is any of a number of medical procedures that involve artificially modifying dentition; in other words, surgery of the teeth, gums and jaw bones.

A bridge is a fixed dental restoration used to replace one or more missing teeth by joining an artificial tooth definitively to adjacent teeth or dental implants.

A dental technician is a member of the dental team who, upon prescription from a dental clinician, constructs custom-made restorative and dental appliances.

A dental implant is a prosthesis that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, or facial prosthesis or to act as an orthodontic anchor. The basis for modern dental implants is a biological process called osseointegration, in which materials such as titanium or zirconia form an intimate bond to the bone. The implant fixture is first placed so that it is likely to osseointegrate, then a dental prosthetic is added. A variable amount of healing time is required for osseointegration before either the dental prosthetic is attached to the implant or an abutment is placed which will hold a dental prosthetic/crown.
Prosthodontics, also known as dental prosthetics or prosthetic dentistry, is the area of dentistry that focuses on dental prostheses. It is one of 12 dental specialties recognized by the American Dental Association (ADA), Royal College of Surgeons of England, Royal College of Surgeons of Edinburgh, Royal College of Surgeons of Ireland, Royal College of Surgeons of Glasgow, Royal College of Dentists of Canada, and Royal Australasian College of Dental Surgeons. The ADA defines it as "the dental specialty pertaining to the diagnosis, treatment planning, rehabilitation and maintenance of the oral function, comfort, appearance and health of patients with clinical conditions associated with missing or deficient teeth or oral and maxillofacial tissues using biocompatible substitutes."
A removable partial denture (RPD) is a denture for a partially edentulous patient who desires to have replacement teeth for functional or aesthetic reasons and who cannot have a bridge for any reason, such as a lack of required teeth to serve as support for a bridge or financial limitations.
A dental emergency is an issue involving the teeth and supporting tissues that are of high importance to be treated by the relevant professional. Dental emergencies do not always involve pain, although this is a common signal that something needs to be looked at. Pain can originate from the tooth, surrounding tissues or can have the sensation of originating in the teeth but be caused by an independent source. Depending on the type of pain experienced an experienced clinician can determine the likely cause and can treat the issue as each tissue type gives different messages in a dental emergency.

Toothlessness, or edentulism, is the condition of having no teeth. In organisms that naturally have teeth, it is the result of tooth loss. Organisms that never possessed teeth can also be described as edentulous. Examples are the members of the former zoological classification order of Edentata, which included anteaters and sloths, as they possess no anterior teeth and no or poorly developed posterior teeth.
A denturist in the United States and Canada, clinical dental technologist in the United Kingdom and Ireland, dental prosthetist in Australia, or a clinical dental technician in New Zealand is a member of the oral health care team and role as primary oral health care provider who provides an oral health examination, planning treatment, takes impressions of the surrounding oral tissues, constructs and delivers removable oral prosthesis treatment directly to the patient.
Fixed prosthodontics is the branch of prosthodontics that focuses on dental prostheses that are permanently affixed (fixed). Crowns, bridges, inlays, onlays, and veneers are some examples of indirect dental restorations. Prosthodontists are dentists who have completed training in this specialty that has been recognized by academic institutes. Fixed prosthodontics can be used to reconstruct single or many teeth, spanning tooth loss areas. The main advantages of fixed prosthodontics over direct restorations are improved strength in big restorations and the possibility to build an aesthetic-looking tooth. The concepts utilised to select the suitable repair, as with any dental restoration, include consideration of the materials to be used, the level of tooth destruction, the orientation and placement of the tooth, and the condition of neighboring teeth

Crown lengthening is a surgical procedure performed by a dentist, or more frequently a periodontist, where more tooth is exposed by removing some of the gingival margin (gum) and supporting bone. Crown lengthening can also be achieved orthodontically by extruding the tooth.
In dentistry, Ante's law is a postulate about crown-to-root ratio put forth by Irwin H. Ante in a thesis paper he wrote in 1926.
In dentistry, overeruption is the physiological movement of a tooth lacking an opposing partner in the dental occlusion. Because of the lack of opposing force and the natural eruptive potential of the tooth there is a tendency for the tooth to erupt out of the line of the occlusion.
In dentistry, an abutment is a connecting element. This is used in the context of a fixed bridge, partial removable dentures and in implants. The implant fixture is the screw-like component that is osseointegrated.

The term All-on-4, also known as All‐on‐Four and All‐in‐Four, refers to 'all' teeth being supported 'on four' dental implants, a prosthodontics procedure for total rehabilitation of the edentulous (toothless) patient, or for patients with badly broken down teeth, decayed teeth, or compromised teeth due to gum disease. It consists of the rehabilitation of either edentulous or dentate maxilla and / or mandible with fixed prosthesis by placing four implants in the anterior maxilla, where bone density is higher. The four implants support a fixed prosthesis with 10 to 14 teeth, and it is placed immediately, typically within 24 hours of surgery.
In dentistry, the neutral zone refers to that space in the oral cavity where the forces exerted by the musculature of the tongue are equal and balanced with the forces exerted by the buccinator muscle of the cheek laterally and the orbicularis oris muscle anteriorly.
Alveoloplasty is a surgical pre-prosthetic procedure performed to facilitate removal of teeth, and smoothen or reshape the jawbone for prosthetic and cosmetic purposes. In this procedure, the bony edges of the alveolar ridge and its surrounding structures is made smooth, redesigned or recontoured so that a well-fitting, comfortable, and esthetic prosthesis may be fabricated or implants may be surgically inserted. This pre-prosthetic surgery which may include bone grafting prepares the mouth to receive a prosthesis or implants by improving the condition and quality of the supporting structures so they can provide support, better retention and stability to the prosthesis.
A complete denture is a removable appliance used when all teeth within a jaw have been lost and need to be prosthetically replaced. In contrast to a partial denture, a complete denture is constructed when there are no more teeth left in an arch, hence it is an exclusively tissue-supported prosthesis. A complete denture can be opposed by natural dentition, a partial or complete denture, fixed appliances or, sometimes, soft tissues.
Occlusion according to The Glossary of Prosthodontic Terms Ninth Edition is defined as 'the static relationship between the incising or masticating surfaces of the maxillary or mandibular teeth or tooth analogues'.