In mammals, the vagina is the elastic, muscular part of the female genital tract. In humans, it extends from the vestibule to the cervix. The outer vaginal opening is normally partly covered by a thin layer of mucosal tissue called the hymen. At the deep end, the cervix bulges into the vagina. The vagina allows for sexual intercourse and birth. It also channels menstrual flow, which occurs in humans and closely related primates as part of the menstrual cycle.
Vulvodynia is a chronic pain syndrome that affects the vulvar area and occurs without an identifiable cause. Symptoms typically include a feeling of burning or irritation. It has been established by the ISSVD that for the diagnosis to be made symptoms must last at least three months.
Dyspareunia is painful sexual intercourse due to medical or psychological causes. The term dyspareunia covers both female dyspareunia and male dyspareunia, but many discussions that use the term without further specification concern the female type, which is more common than the male type. In females, the pain can primarily be on the external surface of the genitalia, or deeper in the pelvis upon deep pressure against the cervix. Medically, dyspareunia is a pelvic floor dysfunction and is frequently underdiagnosed. It can affect a small portion of the vulva or vagina or be felt all over the surface. Understanding the duration, location, and nature of the pain is important in identifying the causes of the pain.

Episiotomy, also known as perineotomy, is a surgical incision of the perineum and the posterior vaginal wall generally done by a midwife or obstetrician. This is usually performed during second stage of labor to quickly enlarge the aperture allowing the baby to pass through. The incision, which can be done from the posterior midline of the vulva straight toward the anus or at an angle to the right or left, is performed under local anesthetic, and is sutured after delivery.

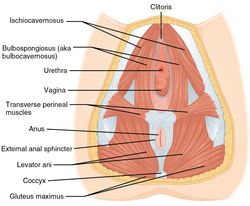
The pelvic floor or pelvic diaphragm is an anatomical location in the human body, which has an important role in urinary and anal continence, sexual function and support of the pelvic organs. The pelvic floor includes muscles, both skeletal and smooth, ligaments and fascia. and separates between the pelvic cavity from above, and the perineum from below. It is formed by the levator ani muscle and coccygeus muscle, and associated connective tissue.
In gynecology, a rectocele or posterior vaginal wall prolapse results when the rectum bulges (herniates) into the vagina. Two common causes of this defect are childbirth and hysterectomy. Rectocele also tends to occur with other forms of pelvic organ prolapse, such as enterocele, sigmoidocele and cystocele.

Vaginoplasty is any surgical procedure that results in the construction or reconstruction of the vagina. It is a type of genitoplasty. Pelvic organ prolapse is often treated with one or more surgeries to repair the vagina. Sometimes a vaginoplasty is needed following the treatment or removal of malignant growths or abscesses to restore a normal vaginal structure and function. Surgery to the vagina is done to correct congenital defects to the vagina, urethra and rectum. It may correct protrusion of the urinary bladder into the vagina (cystocele) and protrusion of the rectum (rectocele) into the vagina. Often, a vaginoplasty is performed to repair the vagina and its attached structures due to trauma or injury. Labiaplasty, which alters the appearance of the vulva, can be performed as a discreet surgery, or as a subordinate procedure within a vaginoplasty.

Vulvectomy refers to a gynecological procedure in which the vulva is partly or completely removed. The procedure is usually performed as a last resort in certain cases of cancer, vulvar dysplasia, vulvar intraepithelial neoplasia, or as part of female genital mutilation. Although there may be severe pain in the groin area after the procedure, for a number of weeks, sexual function is generally still possible but limited.

Labiaplasty is a plastic surgery procedure for altering the labia minora and the labia majora, the folds of skin surrounding the human vulva. There are two main categories of women seeking cosmetic genital surgery: those with congenital conditions such as intersex, and those with no underlying condition who experience physical discomfort or wish to alter the appearance of their genitals because they believe they do not fall within a normal range.

Vaginectomy is a surgery to remove all or part of the vagina. It is one form of treatment for individuals with vaginal cancer or rectal cancer that is used to remove tissue with cancerous cells. It can also be used in gender-affirming surgery. Some people born with a vagina who identify as trans men or as nonbinary may choose vaginectomy in conjunction with other surgeries to make the clitoris more penis-like (metoidioplasty), construct of a full-size penis (phalloplasty), or create a relatively smooth, featureless genital area.
Vulvar vestibulitis syndrome (VVS), vestibulodynia, or simply vulvar vestibulitis, is vulvodynia localized to the vulvar vestibule. It tends to be associated with a highly localized "burning" or "cutting" type of pain. Until recently, "vulvar vestibulitis" was the term used for localized vulvar pain: the suffix "-itis" would normally imply inflammation, but in fact there is little evidence to support an inflammatory process in the condition. "Vestibulodynia" is the term now recognized by the International Society for the Study of Vulvovaginal Disease.

Vulvar cancer is a cancer of the vulva, the outer portion of the female genitals. It most commonly affects the labia majora. Less often, the labia minora, clitoris, or vaginal glands are affected. Symptoms include a lump, itchiness, changes in the skin, or bleeding from the vulva.

Clitoral hood reduction, also termed clitoral hoodectomy, clitoral unhooding, clitoridotomy, or (partial) hoodectomy, is a plastic surgery procedure for reducing the size and the area of the clitoral hood (prepuce) in order to further expose the clitoral glans of the clitoris.

In mammals, the vulva consists of the external female genitalia. The human vulva includes the mons pubis, labia majora, labia minora, clitoris, vestibular bulbs, vulval vestibule, urinary meatus, the vaginal opening, hymen, and Bartholin's and Skene's vestibular glands. The urinary meatus is also included as it opens into the vulval vestibule. Other features of the vulva include the pudendal cleft, sebaceous glands, the urogenital triangle, and pubic hair. The vulva includes the entrance to the vagina, which leads to the uterus, and provides a double layer of protection for this by the folds of the outer and inner labia. Pelvic floor muscles support the structures of the vulva. Other muscles of the urogenital triangle also give support.
A vulvar disease is a particular abnormal, pathological condition that affects part or all of the vulva. Several pathologies are defined. Some can be prevented by vulvovaginal health maintenance.
Genitoplasty is plastic surgery to the genitals. Genitoplasties may be reconstructive to repair injuries, and damage arising from cancer treatment, or congenital disorders, endocrine conditions, or they may be cosmetic.
A vestibulectomy is a gynecological surgical procedure that can be used to treat vulvar pain, specifically in cases of provoked vestibulodynia. Vestibulodynia is a chronic pain syndrome that is a subtype of localized vulvodynia where chronic pain and irritation is present in the vulval vestibule, which is near the entrance of the vagina. Vestibulectomy may be partial or complete.

The vaginal support structures are those muscles, bones, ligaments, tendons, membranes and fascia, of the pelvic floor that maintain the position of the vagina within the pelvic cavity and allow the normal functioning of the vagina and other reproductive structures in the female. Defects or injuries to these support structures in the pelvic floor leads to pelvic organ prolapse. Anatomical and congenital variations of vaginal support structures can predispose a woman to further dysfunction and prolapse later in life. The urethra is part of the anterior wall of the vagina and damage to the support structures there can lead to incontinence and urinary retention.
Transvaginal mesh, also known as vaginal mesh implant, is a net-like surgical tool that is used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI) among female patients. The surgical mesh is placed transvaginally to reconstruct weakened pelvic muscle walls and to support the urethra or bladder.