Related Research Articles

Antipsychotics, also known as neuroleptics, are a class of psychotropic medication primarily used to manage psychosis, principally in schizophrenia but also in a range of other psychotic disorders. They are also the mainstay together with mood stabilizers in the treatment of bipolar disorder.

Benzodiazepines, colloquially called "benzos", are a class of depressant drugs whose core chemical structure is the fusion of a benzene ring and a diazepine ring. They are prescribed to treat conditions such as anxiety disorders, insomnia, and seizures. The first benzodiazepine, chlordiazepoxide (Librium), was discovered accidentally by Leo Sternbach in 1955 and was made available in 1960 by Hoffmann–La Roche, who soon followed with diazepam (Valium) in 1963. By 1977, benzodiazepines were the most prescribed medications globally; the introduction of selective serotonin reuptake inhibitors (SSRIs), among other factors, decreased rates of prescription, but they remain frequently used worldwide.

Hypnotic, or soporific drugs, commonly known as sleeping pills, are a class of psychoactive drugs whose primary function is to induce sleep and to treat insomnia (sleeplessness).

Pharmacology is a science of medical drug and medication, including a substance's origin, composition, pharmacokinetics, therapeutic use, and toxicology. More specifically, it is the study of the interactions that occur between a living organism and chemicals that affect normal or abnormal biochemical function. If substances have medicinal properties, they are considered pharmaceuticals.

Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links health sciences with pharmaceutical sciences and natural sciences. The professional practice is becoming more clinically oriented as most of the drugs are now manufactured by pharmaceutical industries. Based on the setting, pharmacy practice is either classified as community or institutional pharmacy. Providing direct patient care in the community of institutional pharmacies is considered clinical pharmacy.
The Pharmaceutical Benefits Scheme (PBS) is a program of the Australian Government that subsidises prescription medication for Australian citizens and permanent residents, as well as international visitors covered by a reciprocal health care agreement. The PBS is separate to the Medicare Benefits Schedule, a list of health care services that can be claimed under Medicare, Australia's universal health care insurance scheme.
Polypharmacy (polypragmasia) is an umbrella term to describe the simultaneous use of multiple medicines by a patient for their conditions. The term polypharmacy is often defined as regularly taking five or more medicines but there is no standard definition and the term has also been used in the context of when a person is prescribed 2 or more medications at the same time. Polypharmacy may be the consequence of having multiple long-term conditions, also known as multimorbidity and is more common in people who are older. In some cases, an excessive number of medications at the same time is worrisome, especially for people who are older with many chronic health conditions, because this increases the risk of an adverse event in that population. In many cases, polypharmacy cannot be avoided, but 'appropriate polypharmacy' practices are encouraged to decrease the risk of adverse effects. Appropriate polypharmacy is defined as the practice of prescribing for a person who has multiple conditions or complex health needs by ensuring that medications prescribed are optimized and follow 'best evidence' practices.
Pharmacovigilance, also known as drug safety, is the pharmaceutical science relating to the "collection, detection, assessment, monitoring, and prevention" of adverse effects with pharmaceutical products. The etymological roots for the word "pharmacovigilance" are: pharmakon and vigilare. As such, pharmacovigilance heavily focuses on adverse drug reactions (ADR), which are defined as any response to a drug which is noxious and unintended, including lack of efficacy. Medication errors such as overdose, and misuse and abuse of a drug as well as drug exposure during pregnancy and breastfeeding, are also of interest, even without an adverse event, because they may result in an adverse drug reaction.

Nonbenzodiazepines, sometimes referred to colloquially as Z-drugs, are a class of psychoactive drugs that are benzodiazepine-like in uses, such as for treating insomnia and anxiety.

Quazepam, sold under brand name Doral among others, is a relatively long-acting benzodiazepine derivative drug developed by the Schering Corporation in the 1970s. Quazepam is used for the treatment of insomnia including sleep induction and sleep maintenance. Quazepam induces impairment of motor function and has relatively selective hypnotic and anticonvulsant properties with considerably less overdose potential than other benzodiazepines. Quazepam is an effective hypnotic which induces and maintains sleep without disruption of the sleep architecture.
The Beers Criteria for Potentially Inappropriate Medication Use in Older Adults, commonly called the Beers List, are guidelines published by the American Geriatrics Society (AGS) for healthcare professionals to help improve the safety of prescribing medications for adults 65 years and older in all except palliative settings. They emphasize deprescribing medications that are unnecessary, which helps to reduce the problems of polypharmacy, drug interactions, and adverse drug reactions, thereby improving the risk–benefit ratio of medication regimens in at-risk people.

Niaprazine (INN) is a sedative-hypnotic drug of the phenylpiperazine group. It has been used in the treatment of sleep disturbances since the early 1970s in several European countries including France, Italy, and Luxembourg. It is commonly used with children and adolescents on account of its favorable safety and tolerability profile and lack of abuse potential.
The following outline is provided as an overview of and topical guide to clinical research:
A depression rating scale is a psychometric instrument (tool), usually a questionnaire whose wording has been validated with experimental evidence, having descriptive words and phrases that indicate the severity of depression for a time period. When used, an observer may make judgements and rate a person at a specified scale level with respect to identified characteristics. Rather than being used to diagnose depression, a depression rating scale may be used to assign a score to a person's behaviour where that score may be used to determine whether that person should be evaluated more thoroughly for a depressive disorder diagnosis. Several rating scales are used for this purpose.
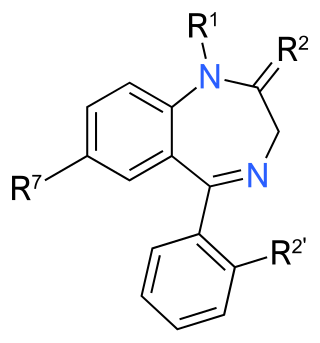
The effects of long-term benzodiazepine use include drug dependence as well as the possibility of adverse effects on cognitive function, physical health, and mental health. Long-term use is sometimes described as use not shorter than three months. Benzodiazepines are generally effective when used therapeutically in the short term, but even then the risk of dependency can be significantly high. There are significant physical, mental and social risks associated with the long-term use of benzodiazepines. Although anxiety can temporarily increase as a withdrawal symptom, there is evidence that a reduction or withdrawal from benzodiazepines can lead in the long run to a reduction of anxiety symptoms. Due to these increasing physical and mental symptoms from long-term use of benzodiazepines, slow withdrawal is recommended for long-term users. Not everyone, however, experiences problems with long-term use.
Late-life depression refers to depression occurring in older adults and has diverse presentations, including as a recurrence of early-onset depression, a new diagnosis of late-onset depression, and a mood disorder resulting from a separate medical condition, substance use, or medication regimen. Research regarding late-life depression often focuses on late-onset depression, which is defined as a major depressive episode occurring for the first time in an older person.

Deprescribing is a process to taper or stop medications with the intention to achieve improved health outcomes by reducing exposure to medications that are potentially either harmful or no longer required. Deprescribing is important to consider with changing health and care goals over time, as well as polypharmacy and adverse effects. Deprescribing can improve adherence, cost, and health outcomes but may have adverse drug withdrawal effects. More specifically, deprescribing is the planned and supervised process of intentionally stopping a medication or reducing its dose to improve the person's health or reduce the risk of adverse side effects. Deprescribing is usually done because the drug may be causing harm, may no longer be helping the patient, or may be inappropriate for the individual patient's current situation. Deprescribing can help correct polypharmacy and prescription cascade.

Brian L. Strom is the inaugural Chancellor of Rutgers Biomedical and Health Sciences and the Executive Vice President for Health Affairs at Rutgers University. Strom was the Executive Vice Dean for Institutional Affairs, Founding Chair of the Department of Biostatistics and Epidemiology, Founding Director of the Center for Clinical Epidemiology and Biostatistics, and Founding Director of the Graduate Program in Epidemiology and Biostatistics, at the Perelman School of Medicine of the University of Pennsylvania. In addition to writing more than 650 papers and 15 books, he has been principal investigator for more than 275 grants. He was honored as one of the Best Doctors in America for each of his last eight years at Penn.
Joerg Hasford is a German physician, biometrician, and epidemiologist. He is emeritus professor in the Institute for Medical Informatics, Biometry and Epidemiology at Ludwig Maximilian University of Munich, chair of the Ethics Committee of the Physicians’ Chamber of the Free State of Bavaria, president of the Association of the Research Ethics Committees in Germany and a member of the Expert Group on Clinical Trials of the European Commission. He has been influential in the study of safety of drugs and pharmacoepidemiology. He was one of the first biostatisticians to look at reliably compiled drug dosing history data in light of pharmacometric consequences. He is the namesake of the Hasford Score, a prognostic score for chronic myeloid leukemia.
References
- ↑ Strom, Brian (2006). Textbook of Pharmacoepidemiology . West Sussex, England: John Wiley and Sons. pp. 3. ISBN 978-0-470-02925-1.
- ↑ Porta M, editor. Greenland S, Hernán M, dos Santos Silva I, Last JM, associate editors (2014). "A dictionary of epidemiology", 6th. edition. New York: Oxford University Press. ISBN 9780199976737
- ↑ Almeida, Osvaldo P.; Page, Amy; Sanfilippo, Frank M.; Etherton-Beer, Christopher (October 2023). "Prospective Association Between the Dispensing of Antidepressants and of Medications to Treat Osteoporosis in Older Age". The American Journal of Geriatric Psychiatry. doi:10.1016/j.jagp.2023.10.004. ISSN 1064-7481. PMID 37919102. S2CID 264118214.
- ↑ Almeida, Osvaldo P.; Etherton-Beer, Christopher; Sanfilippo, Frank; Page, Amy (2024-01-01). "Health morbidities associated with the dispensing of lithium to males and females: Cross-sectional analysis of the 10 % Pharmaceutical Benefits Scheme sample for 2022". Journal of Affective Disorders. 344: 503–509. doi:10.1016/j.jad.2023.10.115. ISSN 1573-2517. PMID 37852583. S2CID 264181868.
- ↑ Ilomäki, Jenni; Fanning, Laura; Keen, Claire; Sluggett, Janet K.; Page, Amy T.; Korhonen, Maarit J.; Meretoja, Atte; Mc Namara, Kevin P.; Bell, J. Simon (2019). "Trends and Predictors of Oral Anticoagulant Use in People with Alzheimer's Disease and the General Population in Australia". Journal of Alzheimer's Disease: JAD. 70 (3): 733–745. doi:10.3233/JAD-190094. ISSN 1875-8908. PMID 31256129. S2CID 195762396.
- ↑ Almeida, Osvaldo P.; Etherton-Beer, Christopher; Kelty, Erin; Sanfilippo, Frank; Preen, David B.; Page, Amy (September 2023). "Lithium Dispensed for Adults Aged ≥ 50 Years Between 2012 and 2021: Analyses of a 10% Sample of the Australian Pharmaceutical Benefits Scheme". The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry. 31 (9): 716–725. doi:10.1016/j.jagp.2023.03.012. ISSN 1545-7214. PMID 37080815. S2CID 257824414.
- ↑ Page, Amy T.; Falster, Michael O.; Litchfield, Melisa; Pearson, Sallie-Anne; Etherton-Beer, Christopher (July 2019). "Polypharmacy among older Australians, 2006-2017: a population-based study". The Medical Journal of Australia. 211 (2): 71–75. doi:10.5694/mja2.50244. ISSN 1326-5377. PMID 31219179. S2CID 195188969.