The ME Association is a UK health charitable organization that provides information, advocacy, and services to persons and families affected by ME/CFS, and raises funds for research into ME/CFS. It has been reported to be one of the two largest UK charities for ME/CFS.

Exercise intolerance is a condition of inability or decreased ability to perform physical exercise at the normally expected level or duration for people of that age, size, sex, and muscle mass. It also includes experiences of unusually severe post-exercise pain, fatigue, nausea, vomiting or other negative effects. Exercise intolerance is not a disease or syndrome in and of itself, but can result from various disorders.

Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) has a long history with an evolution in medical understanding, diagnoses and social perceptions.
Management of ME/CFS focusses on symptoms management, as no treatments that address the root cause of the illness are available. Pacing, or regulating one's activities to avoid triggering worse symptoms, is the most common management strategy for post-exertional malaise. Clinical management varies widely, with many patients receiving combinations of therapies.

Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is an illness with a history of controversy. Although it is classified as an organic disease, it was historically assumed to be psychosocial, and a minority of medical professionals still hold this view. The pathophysiology of ME/CFS remains unclear, there exists many competing diagnostic criteria, and some proposed treatments are controversial. There is a lack of awareness about the condition, which has led to substantiated accusations of patient neglect and harm.

Clinical descriptions of ME/CFS vary. Different groups have produced sets of diagnostic criteria that share many similarities. The biggest differences between criteria are whether post-exertional malaise (PEM) is required, and the number of symptoms needed.
Graded exercise therapy (GET) is a programme of physical activity that starts very slowly and gradually increases over time, intended as a treatment for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Most public health bodies, including the CDC and NICE, consider it ineffective, and its safety is disputed. However, GET still enjoys support among a minority of clinicians and organizations.
David Sheffield Bell is an American physician who has done extensive research on the clinical aspects of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). He has also conducted evaluations and research in pediatric ME/CFS and written numerous articles about the condition.
Daniel Peterson is an American physician in private practice in the state of Nevada, and has been described as a "pioneer" in the treatment of chronic fatigue syndrome (CFS). He graduated from the University of Rochester School of Medicine, Rochester, New York, in 1976 and was an intern and resident at the University of Utah Medical Center from 1976 to 1979. In 1979, he became a diplomate of the American Board of Internal Medicine. He is president of Sierra Internal Medicine of Incline Village, established in 1981.

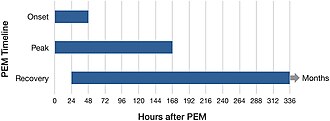
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a debilitating long-term medical condition. People with ME/CFS experience delayed worsening of the illness after minor physical or mental activity, which is the hallmark symptom of the illness. Other symptoms are a greatly reduced ability to do tasks that were previously easy, severe fatigue that does not improve much with rest, and sleep disturbances. Further common symptoms include dizziness or nausea when sitting or standing, along with memory and concentration issues and pain.
Rosamund Vallings is a medical doctor, known as one of the leading authorities on Chronic Fatigue Syndrome (ME/CFS) in New Zealand.
Idiopathic chronic fatigue (ICF) or chronic idiopathic fatigue or insufficient/idiopathic fatigue is a term used for cases of unexplained fatigue that have lasted at least six consecutive months and which do not meet the criteria for Myalgic Encephalomyelitis/chronic fatigue syndrome. Such fatigue is widely understood to have a profound effect on the lives of patients who experience it.
Pacing is an activity management technique for managing a long-term health condition or disability, aiming to maximize what a person can do while reducing, or at least controlling, any symptoms that restrict activity. Pacing is commonly used to help manage conditions that cause chronic pain or chronic fatigue.
Long COVID or long-haul COVID is a group of health problems persisting or developing after an initial period of COVID-19 infection. Symptoms can last weeks, months or years and are often debilitating. The World Health Organization defines long COVID as starting three months after the initial COVID-19 infection, but other agencies define it as starting at four weeks after the initial infection.

A 2-day CPET is a cardiopulmonary exercise test given on two successive days to measure the effect of post-exertional malaise (PEM) on a patient's ability to exercise. PEM is a cardinal symptom of myalgic encephalomyelitis/chronic fatigue syndrome and is common in long COVID as well.
Post-acute infection syndromes (PAISs) or post-infectious syndromes are medical conditions characterized by symptoms attributed to a prior infection. While it is commonly assumed that people either recover or die from infections, long-term symptoms—or sequelae—are a possible outcome as well. Examples include long COVID, chronic fatigue syndrome (ME/CFS), and post-Ebola virus syndrome. Common symptoms include post-exertional malaise (PEM), severe fatigue, neurocognitive symptoms, flu-like symptoms, and pain. The pathology of most of these conditions is not understood and management is generally symptomatic.
Andrew Melvin Ramsay (1901–1990) was a British physician, who is known for his research and advocacy on myalgic encephalomyelitis (ME), a chronic disease causing muscle weakness and cognitive dysfunction. Ramsay worked as a consultant at the Royal Free Hospital in London during a mysterious 1955 disease outbreak of what later became known as ME. He studied the disease and similar outbreaks elsewhere. Work by Ramsay showed that although ME seldom caused death, the disease could be highly disabling.
Carmen Scheibenbogen is a German immunologist who is the acting director of the Institute for Medical Immunology of the Charité university hospital in Berlin. She specialises in hematology, oncology and immunology. She leads the Outpatient Clinic for Immunodeficiency and the Fatigue Centre at the Charité hospital. She is one of the few doctors specialised in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in Germany, and also researches long COVID.
The PACE trial was a large and controversial trial which compared the effects of cognitive behavioural therapy (CBT), graded exercise therapy (GET), adaptive pacing therapy, and specialist medical care for people with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Chronotropic incompetence (CI) is the inability of heart rate to increase as expected in response to exercise. In healthy people, cardiac output during exercise increases via a rise in both heart rate and stroke volume. When the heart rate does not rise sufficiently, this can lead to exercise intolerance. CI can be detected using a cardiopulmonary exercise test. People with CI have a higher risk of cardiovascular disease and early death.