Related Research Articles

Peritonitis is inflammation of the localized or generalized peritoneum, the lining of the inner wall of the abdomen and cover of the abdominal organs. Symptoms may include severe pain, swelling of the abdomen, fever, or weight loss. One part or the entire abdomen may be tender. Complications may include shock and acute respiratory distress syndrome.

Colonoscopy or coloscopy is the endoscopic examination of the large bowel and the distal part of the small bowel with a CCD camera or a fiber optic camera on a flexible tube passed through the anus. It can provide a visual diagnosis and grants the opportunity for biopsy or removal of suspected colorectal cancer lesions.

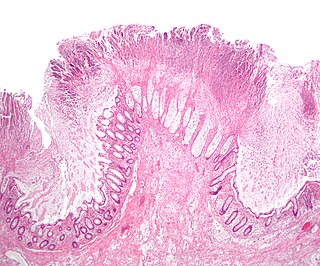
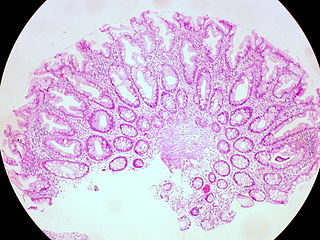
In anatomy, a polyp is an abnormal growth of tissue projecting from a mucous membrane. If it is attached to the surface by a narrow elongated stalk, it is said to be pedunculated; if it is attached without a stalk, it is said to be sessile. Polyps are commonly found in the colon, stomach, nose, ear, sinus(es), urinary bladder, and uterus. They may also occur elsewhere in the body where there are mucous membranes, including the cervix, vocal folds, and small intestine. Some polyps are tumors (neoplasms) and others are non-neoplastic, for example hyperplastic or dysplastic, which are benign. The neoplastic ones are usually benign, although some can be pre-malignant, or concurrent with a malignancy.

In medicine (gastroenterology), angiodysplasia is a small vascular malformation of the gut. It is a common cause of otherwise unexplained gastrointestinal bleeding and anemia. Lesions are often multiple, and frequently involve the cecum or ascending colon, although they can occur at other places. Treatment may be with colonoscopic interventions, angiography and embolization, medication, or occasionally surgery.

Dieulafoy's lesion is a medical condition characterized by a large tortuous arteriole most commonly in the stomach wall (submucosal) that erodes and bleeds. It can present in any part of the gastrointestinal tract. It can cause gastric hemorrhage but is relatively uncommon. It is thought to cause less than 5% of all gastrointestinal bleeds in adults. It was named after French surgeon Paul Georges Dieulafoy, who described this condition in his paper "Exulceratio simplex: Leçons 1-3" in 1898. It is also called "caliber-persistent artery" or "aneurysm" of gastric vessels. However, unlike most other aneurysms, these are thought to be developmental malformations rather than degenerative changes.

Rectal foreign bodies are large foreign items found in the rectum that can be assumed to have been inserted through the anus, rather than reaching the rectum via the mouth and gastrointestinal tract. It can be of clinical relevance if the patient cannot remove it the way they intended. Smaller, ingested foreign bodies, such as bones eaten with food, can sometimes be found stuck in the rectum upon x-ray and are rarely of clinical relevance.
Toxic megacolon is an acute form of colonic distension. It is characterized by a very dilated colon (megacolon), accompanied by abdominal distension (bloating), and sometimes fever, abdominal pain, or shock.

Gastrointestinal perforation, also known as ruptured bowel, is a hole in the wall of part of the gastrointestinal tract. The gastrointestinal tract includes the esophagus, stomach, small intestine, and large intestine. Symptoms include severe abdominal pain and tenderness. When the hole is in the stomach or early part of the small intestine, the onset of pain is typically sudden while with a hole in the large intestine onset may be more gradual. The pain is usually constant in nature. Sepsis, with an increased heart rate, increased breathing rate, fever, and confusion may occur.

Lower gastrointestinal bleeding, commonly abbreviated LGIB, is any form of gastrointestinal bleeding in the lower gastrointestinal tract. LGIB is a common reason for seeking medical attention at a hospital's emergency department. LGIB accounts for 30–40% of all gastrointestinal bleeding and is less common than upper gastrointestinal bleeding (UGIB). It is estimated that UGIB accounts for 100–200 per 100,000 cases versus 20–27 per 100,000 cases for LGIB. Approximately 85% of lower gastrointestinal bleeding involves the colon, 10% are from bleeds that are actually upper gastrointestinal bleeds, and 3–5% involve the small intestines.

Fundic gland polyposis is a medical syndrome where the fundus and the body of the stomach develop many fundic gland polyps. The condition has been described both in patients with familial adenomatous polyposis (FAP) and attenuated variants (AFAP), and in patients in whom it occurs sporadically.

Argon plasma coagulation (APC) is a medical endoscopic procedure used to control bleeding from certain lesions in the gastrointestinal tract. It is administered during esophagogastroduodenoscopy or colonoscopy.

Colonic polypectomy is the removal of colorectal polyps in order to prevent them from turning cancerous.

An endoclip is a metallic mechanical device used in endoscopy in order to close two mucosal surfaces without the need for surgery and suturing. Its function is similar to a suture in gross surgical applications, as it is used to join together two disjointed surfaces, but, can be applied through the channel of an endoscope under direct visualization. Endoclips have found use in treating gastrointestinal bleeding, in preventing bleeding after therapeutic procedures such as polypectomy, and in closing gastrointestinal perforations. Many forms of endoclips exist of different shapes and sizes, including two and three prong devices, which can be administered using single use and reloadable systems, and may or may not open and close to facilitate placement.
Hiromi Shinya is a Japanese-born general surgeon. He pioneered modern colonoscopic techniques, and invented the electrosurgical polypectomy snare now common on colonoscopes, allowing for removal of colon polyps without invasive surgery.

A colorectal polyp is a polyp occurring on the lining of the colon or rectum. Untreated colorectal polyps can develop into colorectal cancer.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
The non-lifting sign is a finding on endoscopic examination that provides information on the suitability of large flat or sessile colorectal polyps for polypectomy by endoscopic mucosal resection (EMR). When fluid is injected under a polyp in preparation for endoscopic mucosal resection, some polyps do not "lift", indicating that the polyp is not separating from the submucosa. This makes polypectomy more technically difficult, and increases the risk of intestinal perforation if polypectomy is then attempted. It is also thought to be indicative of an early colorectal cancer that has invaded the submucosa significantly, which would make surgical removal of the tumour preferable to allow complete removal of the cancer. Consequently, the non-lifting sign is generally considered to be a contraindication to performing endoscopic mucosal resection.
Endoscopic mucosal resection is a technique used to remove cancerous or other abnormal lesions found in the digestive tract. It is one method of performing a mucosectomy.
Serrated polyposis syndrome (SPS), previously known as hyperplastic polyposis syndrome, is a disorder characterized by the appearance of serrated polyps in the colon. While serrated polyposis syndrome does not cause symptoms, the condition is associated with a higher risk of colorectal cancer (CRC). The lifelong risk of CRC is between 25 and 40%. SPS is the most common polyposis syndrome affecting the colon, but is under recognized due to a lack of systemic long term monitoring. Diagnosis requires colonoscopy, and is defined by the presence of either of two criteria: ≥5 serrated lesions/polyps proximal to the rectum, or >20 serrated lesions/polyps of any size distributed throughout the colon with 5 proximal to the rectum.
Juvenile polyps are a type of polyp found in the colon. While juvenile polyps are typically found in children, they may be found in people of any age. Juvenile polyps are a type of hamartomatous polyps, which consist of a disorganized mass of tissue. They occur in about two percent of children. Juvenile polyps often do not cause symptoms (asymptomatic); when present, symptoms usually include gastrointestinal bleeding and prolapse through the rectum. Juvenile polyps are diagnosed via colonoscopy or flexible sigmoidoscopy. If symptoms are present, then removal of the polyp (polypectomy) is warranted. In the absence of symptoms, removal is not necessary. Recurrence of polyps following removal is relatively common. Juvenile polyps are usually sporadic, occurring in isolation, although they may occur as a part of juvenile polyposis syndrome. Sporadic juvenile polyps may occur in any part of the colon, but are usually found in the distal colon. In contrast to other types of colon polyps, juvenile polyps are not premalignant and are not usually associated with a higher risk of cancer; however, individuals with juvenile polyposis syndrome are at increased risk of gastric and colorectal cancer., Unlike juvenile polyposis syndrome, solitary juvenile polyps do not require follow up with surveillance colonoscopy.
References
- 1 2 3 4 5 Hirasawa, K; Sato, C; Makazu, M; Kaneko, H; Kobayashi, R; Kokawa, A; Maeda, S (10 September 2015). "Coagulation syndrome: Delayed perforation after colorectal endoscopic treatments". World Journal of Gastrointestinal Endoscopy. 7 (12): 1055–61. doi:10.4253/wjge.v7.i12.1055. PMC 4564832 . PMID 26380051.
- 1 2 La Regina, D; Mongelli, F; Fasoli, A; Lollo, G; Ceppi, M; Saporito, A; Garofalo, F; Di Giuseppe, M; Ferrario di Tor Vajana, A (2020). "Clinical Adverse Events after Endoscopic Resection for Colorectal Lesions: A Meta-Analysis on the Antibiotic Prophylaxis". Digestive Diseases (Basel, Switzerland). 38 (1): 15–22. doi: 10.1159/000502055 . PMID 31408875. S2CID 199573818.
- 1 2 3 4 5 6 Kim, HW (May 2014). "What Is Different between Postpolypectomy Fever and Postpolypectomy Coagulation Syndrome?". Clinical Endoscopy. 47 (3): 205–6. doi:10.5946/ce.2014.47.3.205. PMC 4058534 . PMID 24944980.
- ↑ Shin, YJ; Kim, YH; Lee, KH; Lee, YJ; Park, JH (October 2016). "CT findings of post-polypectomy coagulation syndrome and colonic perforation in patients who underwent colonoscopic polypectomy". Clinical Radiology. 71 (10): 1030–6. doi:10.1016/j.crad.2016.03.010. PMID 27085213.
- ↑ Waye, JD (June 1993). "Management of complications of colonoscopic polypectomy". The Gastroenterologist. 1 (2): 158–64. PMID 8049888.