Pelvic inflammatory disease, also known as pelvic inflammatory disorder (PID), is an infection of the upper part of the female reproductive system, namely the uterus, fallopian tubes, and ovaries, and inside of the pelvis. Often, there may be no symptoms. Signs and symptoms, when present, may include lower abdominal pain, vaginal discharge, fever, burning with urination, pain with sex, bleeding after sex, or irregular menstruation. Untreated PID can result in long-term complications including infertility, ectopic pregnancy, chronic pelvic pain, and cancer.

Endometriosis is a disease of the female reproductive system in which cells similar to those in the endometrium, the layer of tissue that normally covers the inside of the uterus, grow outside the uterus. Most often this is on the ovaries, fallopian tubes, and tissue around the uterus and ovaries; however, in rare cases it may also occur in other parts of the body. Some symptoms include pelvic pain, heavy periods, pain with bowel movements, and infertility. Nearly half of those affected have chronic pelvic pain, while in 70% pain occurs during menstruation. Pain during sexual intercourse is also common. Infertility occurs in up to half of affected individuals. About 25% of individuals have no symptoms and 85% of those seen with infertility in a tertiary center have no pain. Endometriosis can have both social and psychological effects.
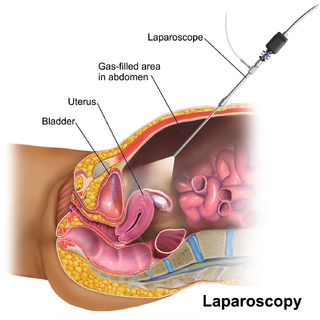
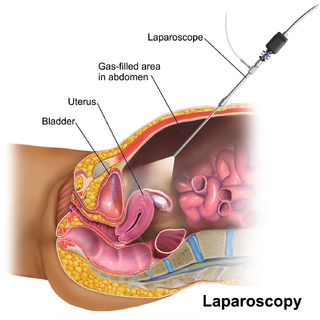
Laparoscopy is an operation performed in the abdomen or pelvis using small incisions with the aid of a camera. The laparoscope aids diagnosis or therapeutic interventions with a few small cuts in the abdomen.
Chronic pain is classified as pain that lasts longer than three to six months. In medicine, the distinction between acute and chronic pain is sometimes determined by the amount of time since onset. Two commonly used markers are pain that continues at 3 months and 6 months since onset, but some theorists and researchers have placed the transition from acute to chronic pain at 12 months. Others apply the term acute to pain that lasts less than 30 days, chronic to pain of more than six months duration, and subacute to pain that lasts from one to six months. A popular alternative definition of chronic pain, involving no fixed duration, is "pain that extends beyond the expected period of healing".

Pain management is an aspect of medicine and health care involving relief of pain in various dimensions, from acute and simple to chronic and challenging. Most physicians and other health professionals provide some pain control in the normal course of their practice, and for the more complex instances of pain, they also call on additional help from a medical specialty devoted to pain, which is called pain medicine. Pain management often uses a multidisciplinary approach for easing the suffering and improving the quality of life of anyone experiencing pain, whether acute pain or chronic pain. Relief of pain in general (analgesia) is often an acute affair, whereas managing chronic pain requires additional dimensions. The typical pain management team includes medical practitioners, pharmacists, clinical psychologists, physiotherapists, occupational therapists, recreational therapists, physician assistants, nurses, and dentists. The team may also include other mental health specialists and massage therapists. Pain sometimes resolves quickly once the underlying trauma or pathology has healed, and is treated by one practitioner, with drugs such as pain relievers (analgesics) and occasionally also anxiolytics. Effective management of chronic (long-term) pain, however, frequently requires the coordinated efforts of the pain management team. Effective pain management does not always mean total eradication of all pain. Rather, it often means achieving adequate quality of life in the presence of pain, through any combination of lessening the pain and/or better understanding it and being able to live happily despite it.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.
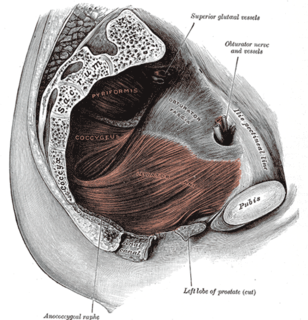
Pudendal nerve entrapment (PNE), also known as Alcock canal syndrome, is an uncommon source of chronic pain in which the pudendal nerve is entrapped or compressed in Alcock's canal. There are several different types of PNE based on the site of entrapment anatomically. Pain is positional and is worsened by sitting. Other symptoms include genital numbness, fecal incontinence and urinary incontinence.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.

The superior hypogastric plexus is a plexus of nerves situated on the vertebral bodies anterior to the bifurcation of the abdominal aorta.

Pelvic pain is pain in the area of the pelvis. Acute pain is more common than chronic pain. If the pain lasts for more than six months, it is deemed to be chronic pelvic pain. It can affect both the male and female pelvis.
A neurectomy is a type of nerve block involving the severing or removal of a nerve. This surgery is performed in rare cases of severe chronic pain where no other treatments have been successful, and for other conditions such as vertigo, involuntary twitching and excessive blushing or sweating.

The inferior hypogastric plexus is a network of nerves that supplies the organs of the pelvic cavity. The inferior hypogastric plexus gives rise to the prostatic plexus in males and the uterovaginal plexus in females.
Post herniorrhaphy pain syndrome, or inguinodynia is pain or discomfort lasting greater than 3 months after surgery of inguinal hernia. Randomized trials of laparoscopic vs open inguinal hernia repair have demonstrated similar recurrence rates with the use of mesh and have identified that chronic groin pain (>10%) surpasses recurrence (<2%) and is an important measure of success.

Adhesions are fibrous bands that form between tissues and organs, often as a result of injury during surgery. They may be thought of as internal scar tissue that connects tissues not normally connected.
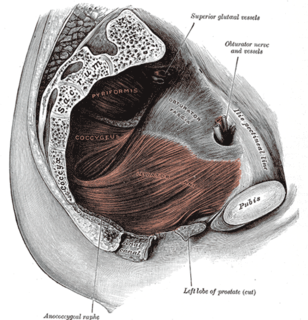
Pelvic splanchnic nerves or nervi erigentes are splanchnic nerves that arise from sacral spinal nerves S2, S3, S4 to provide parasympathetic innervation to the organs of the pelvic cavity.
Total mesorectal excision (TME) is a standard surgical technique for treatment of rectal cancer, first described in 1982 by Professor Bill Heald at the UK's Basingstoke District Hospital. It is a precise dissection of the mesorectal envelope comprising rectum containing the tumour together with all the surrounding fatty tissue and the sheet of tissue that contains lymph nodes and blood vessels. Dissection is along the avascular alveolar plane between the presacral and mesorectal fascia, described as holy plane. Dissection along this plane facilitates a straightforward dissection and preserves the sacral vessels and hypogastric nerves and is a sphincter-sparing resection and decreases permanent stoma rates. It is possible to rejoin the two ends of the colon; however, most patients require a temporary ileostomy pouch to bypass the colon, allowing it to heal with less risk of infection, perforation or leakage.
Manipulation under anesthesia (MUA) or fibrosis release procedures is a multidisciplinary, chronic pain-related manual therapy modality which is used for the purpose of improving articular and soft tissue movement. This is accomplished by way of a combination of controlled joint mobilization/manipulation and myofascial release techniques. Medication-assisted manipulation (MAM) may also be used to describe the procedure, although that term more broadly categorizes the varied forms of existing MUA techniques. In any form, MUA is used by osteopathic/orthopedic physicians and specially trained chiropractors. It is intended as a means of breaking up adhesions of or about spinal joints, or extremity joint articulations to which painfully restricted range of motion significantly limits function. Failed attempts at other standard conservative treatment methods, over a sufficient time-frame, is one of the principal patient qualifiers.
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), previously known as chronic nonbacterial prostatitis, is long-term pelvic pain and lower urinary tract symptoms (LUTS) without evidence of a bacterial infection. It affects about 2–6% of men. Together with IC/BPS, it makes up urologic chronic pelvic pain syndrome (UCPPS).
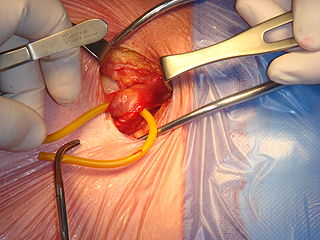
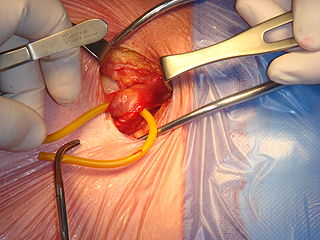
Inguinal hernia surgery is an operation to repair a weakness in the abdominal wall that abnormally allows abdominal contents to slip into a narrow tube called the inguinal canal in the groin region.

A lumbar anterior root stimulator is a type of neuroprosthesis used in patients with a spinal cord injury or to treat some forms of chronic spinal pain. More specifically, the root stimulator can be used in patients who have lost proper bowel function due to damaged neurons related to gastrointestinal control and potentially allow paraplegics to exercise otherwise paralyzed leg muscles.