A mental disorder, also referred to as a mental illness or psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. A mental disorder is also characterized by a clinically significant disturbance in an individual's cognition, emotional regulation, or behavior. It is usually associated with distress or impairment in important areas of functioning. There are many different types of mental disorders. Mental disorders may also be referred to as mental health conditions. Such features may be persistent, relapsing and remitting, or occur as single episodes. Many disorders have been described, with signs and symptoms that vary widely between specific disorders. Such disorders may be diagnosed by a mental health professional, usually a clinical psychologist or psychiatrist.
A psychiatrist is a physician who specializes in psychiatry. Psychiatrists are physicians and evaluate patients to determine whether their symptoms are the result of a physical illness, a combination of physical and mental ailments or strictly mental issues. Sometimes a psychiatrist works within a multi-disciplinary team, which may comprise clinical psychologists, social workers, occupational therapists, and nursing staff. Psychiatrists have broad training in a biopsychosocial approach to the assessment and management of mental illness.
Anti-psychiatry, sometimes spelled antipsychiatry, is a movement based on the view that psychiatric treatment is often more damaging than helpful to patients, highlighting controversies about psychiatry. Objections include the reliability of psychiatric diagnosis, the questionable effectiveness and harm associated with psychiatric medications, the failure of psychiatry to demonstrate any disease treatment mechanism for psychiatric medication effects, and legal concerns about equal human rights and civil freedom being nullified by the presence of diagnosis. Historically critiques of psychiatry came to light after focus on the extreme harms associated with electroconvulsive treatment or insulin shock therapy. The term "anti-psychiatry" is in dispute and often used to dismiss all critics of psychiatry, many of whom agree that a specialized role of helper for people in emotional distress may at times be appropriate, and allow for individual choice around treatment decisions.
Factitious disorder imposed on self, also known as Munchausen syndrome, is a factitious disorder in which those affected feign or induce disease, illness, injury, abuse, or psychological trauma to draw attention, sympathy, or reassurance to themselves. Munchausen syndrome fits within the subclass of factitious disorder with predominantly physical signs and symptoms, but patients also have a history of recurrent hospitalization, travelling, and dramatic, extremely improbable tales of their past experiences. The condition derives its name from the fictional character Baron Munchausen.
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis requires symptoms of both schizophrenia and a mood disorder: either bipolar disorder or depression. The main criterion is the presence of psychotic symptoms for at least two weeks without any mood symptoms. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar I disorder, schizophreniform disorder, or schizophrenia. This is a problem as treatment and prognosis differ greatly for most of these diagnoses.
Clinical psychology is an integration of human science, behavioral science, theory, and clinical knowledge for the purpose of understanding, preventing, and relieving psychologically-based distress or dysfunction and to promote subjective well-being and personal development. Central to its practice are psychological assessment, clinical formulation, and psychotherapy, although clinical psychologists also engage in research, teaching, consultation, forensic testimony, and program development and administration. In many countries, clinical psychology is a regulated mental health profession.
Forensic psychiatry is a subspeciality of psychiatry and is related to criminology. It encompasses the interface between law and psychiatry. According to the American Academy of Psychiatry and the Law, it is defined as "a subspecialty of psychiatry in which scientific and clinical expertise is applied in legal contexts involving civil, criminal, correctional, regulatory, or legislative matters, and in specialized clinical consultations in areas such as risk assessment or employment." A forensic psychiatrist provides services – such as determination of competency to stand trial – to a court of law to facilitate the adjudicative process and provide treatment, such as medications and psychotherapy, to criminals.
The mental status examination (MSE) is an important part of the clinical assessment process in neurological and psychiatric practice. It is a structured way of observing and describing a patient's psychological functioning at a given point in time, under the domains of appearance, attitude, behavior, mood and affect, speech, thought process, thought content, perception, cognition, insight, and judgment. There are some minor variations in the subdivision of the MSE and the sequence and names of MSE domains.
Social psychiatry is a branch of psychiatry that focuses on the interpersonal and cultural context of mental disorder and mental wellbeing. It involves a sometimes disparate set of theories and approaches, with work stretching from epidemiological survey research on the one hand, to an indistinct boundary with individual or group psychotherapy on the other. Social psychiatry combines a medical training and perspective with fields such as social anthropology, social psychology, cultural psychiatry, sociology and other disciplines relating to mental distress and disorder. Social psychiatry has been particularly associated with the development of therapeutic communities, and to highlighting the effect of socioeconomic factors on mental illness. Social psychiatry can be contrasted with biopsychiatry, with the latter focused on genetics, brain neurochemistry and medication. Social psychiatry was the dominant form of psychiatry for periods of the 20th century but is currently less visible than biopsychiatry.
Psychiatric nursing or mental health nursing is the appointed position of a nurse that specialises in mental health, and cares for people of all ages experiencing mental illnesses or distress. These include: neurodevelopmental disorders, schizophrenia, schizoaffective disorder, mood disorders, addiction, anxiety disorders, personality disorders, eating disorders, suicidal thoughts, psychosis, paranoia, and self-harm.

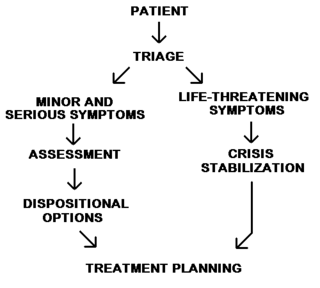
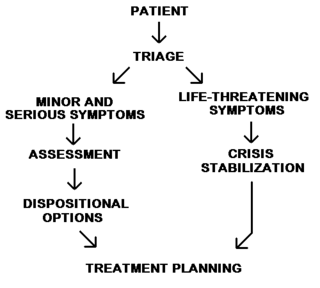
Emergency psychiatry is the clinical application of psychiatry in emergency settings. Conditions requiring psychiatric interventions may include attempted suicide, substance abuse, depression, psychosis, violence or other rapid changes in behavior.
Medical model is the term coined by psychiatrist R. D. Laing in his The Politics of the Family and Other Essays (1971), for the "set of procedures in which all doctors are trained". It includes complaint, history, physical examination, ancillary tests if needed, diagnosis, treatment, and prognosis with and without treatment.
Psychiatric and mental health nurses in the U.S. Army Nurse Corps employing groundbreaking protocols and treatments in psychiatric issues to address the unique challenges that our service men and women face, more commonly post-traumatic stress disorder and traumatic brain injuries. Most people understand that trauma exposure is a popular occupational hazard for military members. Psychiatric screenings, before and during their enlistment, and treatments after being exposed to warfare, death, destruction, and torture have been extremely beneficial for military personnel and their dependents.
A mental health professional is a health care practitioner or social and human services provider who offers services for the purpose of improving an individual's mental health or to treat mental disorders. This broad category was developed as a name for community personnel who worked in the new community mental health agencies begun in the 1970s to assist individuals moving from state hospitals, to prevent admissions, and to provide support in homes, jobs, education, and community. These individuals were the forefront brigade to develop the community programs, which today may be referred to by names such as supported housing, psychiatric rehabilitation, supported or transitional employment, sheltered workshops, supported education, daily living skills, affirmative industries, dual diagnosis treatment, individual and family psychoeducation, adult day care, foster care, family services and mental health counseling.
In the United States, a psychiatric-mental health nurse practitioner (PMHNP) is an advanced practice registered nurse trained to provide a wide range of mental health services to patients and families in a variety of settings. PMHNPs diagnose, conduct therapy, and prescribe medications for patients who have psychiatric disorders, medical organic brain disorders or substance abuse problems. They are licensed to provide emergency psychiatric services, psychosocial and physical assessment of their patients, treatment plans, and manage patient care. They may also serve as consultants or as educators for families and staff. The PMHNP has a focus on psychiatric diagnosis, including the differential diagnosis of medical disorders with psychiatric symptoms, and on medication treatment for psychiatric disorders.
Child and adolescent psychiatry is a branch of psychiatry that focuses on the diagnosis, treatment, and prevention of mental disorders in children, adolescents, and their families. It investigates the biopsychosocial factors that influence the development and course of psychiatric disorders and treatment responses to various interventions. Child and adolescent psychiatrists primarily use psychotherapy and/or medication to treat mental disorders in the pediatric population.
Psychiatry is the medical specialty devoted to the diagnosis, prevention, and treatment of deleterious mental conditions. These include various matters related to mood, behaviour, cognition, and perceptions.
A psychological injury is the psychological or psychiatric consequence of a traumatic event or physical injury. Such an injury might result from events such as abusive behavior, whistleblower retaliation, bullying, kidnapping, rape, motor vehicular collision or other negligent action. It may cause impairments, disorders, and disabilities perhaps as an exacerbation of a pre-existing condition.
The following outline is provided as an overview of and topical guide to psychiatry:
Psychiatry is, and has historically been, viewed as controversial by those under its care, as well as sociologists and psychiatrists themselves. There are a variety of reasons cited for this controversy, including the subjectivity of diagnosis, the use of diagnosis and treatment for social and political control including detaining citizens and treating them without consent, the side effects of treatments such as electroconvulsive therapy, antipsychotics and historical procedures like the lobotomy and other forms of psychosurgery or insulin shock therapy, and the history of racism within the profession in the United States.