Alexander disease is a very rare autosomal dominant leukodystrophy, which are neurological conditions caused by anomalies in the myelin which protects nerve fibers in the brain. The most common type is the infantile form that usually begins during the first two years of life. Symptoms include mental and physical developmental delays, followed by the loss of developmental milestones, an abnormal increase in head size and seizures. The juvenile form of Alexander disease has an onset between the ages of 2 and 13 years. These children may have excessive vomiting, difficulty swallowing and speaking, poor coordination, and loss of motor control. Adult-onset forms of Alexander disease are less common. The symptoms sometimes mimic those of Parkinson's disease or multiple sclerosis, or may present primarily as a psychiatric disorder.

Progressive supranuclear palsy (PSP) is a late-onset neurodegenerative disease involving the gradual deterioration and death of specific volumes of the brain. The condition leads to symptoms including loss of balance, slowing of movement, difficulty moving the eyes, and cognitive impairment. PSP may be mistaken for other types of neurodegeneration such as Parkinson's disease, frontotemporal dementia and Alzheimer's disease. The cause of the condition is uncertain, but involves the accumulation of tau protein within the brain. Medications such as levodopa and amantadine may be useful in some cases.
Thalamotomy is a surgical procedure in which a functional lesion is made into the thalamus to improve the overall brain function in patients. First introduced in the 1950s, it is primarily effective for tremors such as those associated with Parkinson's disease, where a selected portion of the thalamus is surgically destroyed (ablated). Neurosurgeons use specialized equipment to precisely locate an area of the thalamus, usually choosing to work on only one side. Bilateral procedures are poorly tolerated because of increased complications and risk, including vision and speech problems. The positive effects on tremors are immediate. Other less destructive procedures are sometimes preferred, such as subthalamic deep brain stimulation, since this procedure can also improve tremors and other symptoms of PD.
Spinocerebellar ataxia (SCA) is a progressive, degenerative, genetic disease with multiple types, each of which could be considered a neurological condition in its own right. An estimated 150,000 people in the United States have a diagnosis of spinocerebellar ataxia at any given time. SCA is hereditary, progressive, degenerative, and often fatal. There is no known effective treatment or cure. SCA can affect anyone of any age. The disease is caused by either a recessive or dominant gene. In many cases people are not aware that they carry a relevant gene until they have children who begin to show signs of having the disorder.
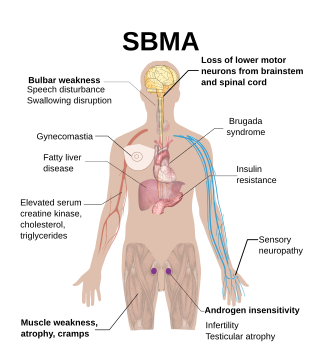
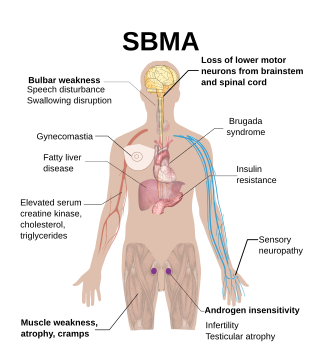
Spinal and bulbar muscular atrophy (SBMA), popularly known as Kennedy's disease, is a rare, adult-onset, X-linked recessive lower motor neuron disease caused by trinucleotide CAG repeat expansions in exon 1 of the androgen receptor (AR) gene, which results in both loss of AR function and toxic gain of function.

Corticobasal degeneration (CBD) is a rare neurodegenerative disease involving the cerebral cortex and the basal ganglia. CBD symptoms typically begin in people from 50 to 70 years of age, and typical survival before death is eight years. It is characterized by marked disorders in movement and cognition, and is classified as one of the Parkinson plus syndromes. Diagnosis is difficult, as symptoms are often similar to those of other disorders, such as Parkinson's disease, progressive supranuclear palsy, and dementia with Lewy bodies, and a definitive diagnosis of CBD can only be made upon neuropathologic examination.

Omigapil is a drug that was developed by Novartis and tested in clinical trials for its ability to help treat Parkinson's disease (PD) and amyotrophic lateral sclerosis (ALS). The development for PD and ALS have been terminated due to lack of benefit, but Santhera Pharmaceuticals bought the compound for development for the treatment of congenital muscular dystrophy (CMD).

Tauopathies are neurodegenerative diseases involving the aggregation of abnormal tau protein. Tangles are formed by hyperphosphorylation of the microtubule protein known as tau, causing the protein to dissociate from microtubules and form insoluble aggregate. Various neuropathologic phenotypes are identified based on the specific engagement of anatomical regions, cell types, and the presence of unique isoforms of tau within pathological deposits. The designation 'primary tauopathy' is assigned to disorders where the predominant feature is the deposition of tau protein. Alternatively, diseases exhibiting tau pathologies attributed to different and varied underlying causes are termed 'secondary tauopathies. Some neuropathologic phenotypes involving tau protein is Alzheimer's disease, Pick disease, Progressive supranuclear palsy and corticobasal degeneration.

A neurodegenerative disease is caused by the progressive loss of structure or function of neurons, in the process known as neurodegeneration. Such neuronal damage may ultimately involve cell death. Neurodegenerative diseases include amyotrophic lateral sclerosis, multiple sclerosis, Parkinson's disease, Alzheimer's disease, Huntington's disease, multiple system atrophy, tauopathies, and prion diseases. Neurodegeneration can be found in the brain at many different levels of neuronal circuitry, ranging from molecular to systemic. Because there is no known way to reverse the progressive degeneration of neurons, these diseases are considered to be incurable; however research has shown that the two major contributing factors to neurodegeneration are oxidative stress and inflammation. Biomedical research has revealed many similarities between these diseases at the subcellular level, including atypical protein assemblies and induced cell death. These similarities suggest that therapeutic advances against one neurodegenerative disease might ameliorate other diseases as well.

Rasagiline is an irreversible inhibitor of monoamine oxidase-B used as a monotherapy to treat symptoms in early Parkinson's disease or as an adjunct therapy in more advanced cases.
In the management of Parkinson's disease, due to the chronic nature of Parkinson's disease (PD), a broad-based program is needed that includes patient and family education, support-group services, general wellness maintenance, exercise, and nutrition. At present, no cure for the disease is known, but medications or surgery can provide relief from the symptoms.

Parkinson's disease (PD), or simply Parkinson's, is a chronic degenerative disorder of the central nervous system that affects both the motor system and non-motor systems. The symptoms usually emerge slowly, and as the disease progresses, non-motor symptoms become more common. Early symptoms are tremor, rigidity, slowness of movement, and difficulty with walking. Problems may also arise with cognition, behaviour, sleep, and sensory systems. Parkinson's disease dementia is common in advanced stages.
The Pacific Udall Center was established in 2009 as a new Morris K. Udall Center of Excellence for Parkinson's Disease Research. It is one of nine Udall Centers across the U.S. that honor former Utah Congressman Morris Udall with a "multidisciplinary research approach to elucidate the fundamental causes of PD [Parkinson's Disease] as well as to improve the diagnosis and treatment of patients with Parkinson's and related neurodegenerative disorders." The Pacific Udall Center is a collaboration among Stanford University, the University of Washington, the VA Puget Sound Health Care System, Oregon Health & Science University, and the Portland VA Medical Center. It is funded by a grant from the National Institute of Neurological Disorders and Stroke.

Parkinsonian gait is the type of gait exhibited by patients with Parkinson's disease (PD). It is often described by people with Parkinson's as feeling like being stuck in place, when initiating a step or turning, and can increase the risk of falling. This disorder is caused by a deficiency of dopamine in the basal ganglia circuit leading to motor deficits. Gait is one of the most affected motor characteristics of this disorder although symptoms of Parkinson's disease are varied.
The Lee Silverman Voice Treatment – LOUD is a treatment for speech disorders associated with Parkinson's disease (PD). It focuses on increasing vocal loudness and is delivered by a speech therapist in sixteen one-hour sessions spread over four weeks. A derivative of this treatment, known as LSVT BIG, is used in treating movement aspects of Parkinson's disease.
Gene therapy in Parkinson's disease consists of the creation of new cells that produce a specific neurotransmitter (dopamine), protect the neural system, or the modification of genes that are related to the disease. Then these cells are transplanted to a patient with the disease. There are different kinds of treatments that focus on reducing the symptoms of the disease but currently there is no cure.
Rhonda Renee Voskuhl is an American physician, research scientist, and professor. She is a member of the Brain Research Institute (BRI) at the David Geffen School of Medicine at UCLA and is the director of its Multiple Sclerosis Program. Voskuhl has published numerous scientific articles in academic journals and has served in the role of principal investigator for several treatment trials investigating potential treatments for multiple sclerosis (MS).

The Shake It Up Australia Foundation (SIUAF) is an Australian non-for-profit foundation founded in 2011 by Clyde and Greg Campbell. It is partnered with the Michael J. Fox Foundation (MJFF) to achieve the foundations primary aims of "promoting and funding Parkinson's disease research in Australia to slow, stop and cure the disease". Together MJFF and SIUAF are the largest non-government funders of Parkinson's research across multiple institutes in Australia. Since its founding, the foundation has co-founded 38 Parkinson's research projects across 12 institutes to the value of over $10.8 million. The foundation's funding model ensures that 100% of proceeds goes towards Parkinson's research in Australia. This is possible due to the founding directors covering all overhead costs and expenses. In January 2019, Shake It Up are one of the partner organisation in the Australian Parkinson's Mission which was awarded a $30 million-dollar grant to test repurposed drugs in clinical trials.
Rapid eye movement sleep behaviour disorder and Parkinson's disease is rapid eye movement sleep behavior disorder (RBD) that is associated with Parkinson's disease. RBC is linked genetically and neuropathologically to α- synuclein, a presynaptic neuronal protein that exerts deleterious effects on neighbouring proteins, leading to neuronal death. This pathology is linked to numerous other neurodegenerative disorders, such as Lewy bodies dementia, and collectively these disorders are known as synucleinopathies. Numerous reports over the past few years have stated the frequent association of synucleinopathies with REM sleep behaviour disorder (RBD). In particular, the frequent association of RBD with Parkinson's. In the general population the incidence of RBD is around 0.5%, compared to the prevalence of RBD in PD patients, which has been reported to be between 38% and 60%. The diagnosis and symptom onset of RBD typically precedes the onset of motor or cognitive symptoms of PD by a number of years, typically ranging anywhere from 2 to 15 years prior. Hence, this link could provide an important window of opportunity in the implementation of therapies and treatments, that could prevent or slow the onset of PD.
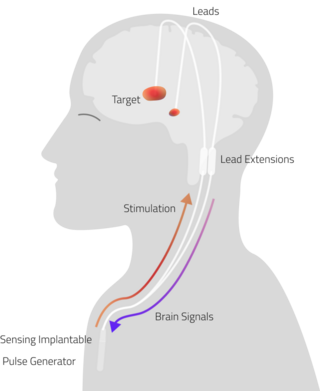
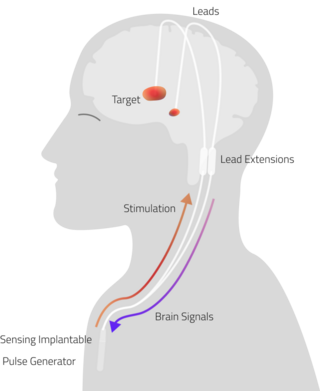
Adaptive Deep Brain Stimulation (aDBS), also known as Closed Loop Deep Brain stimulation (clDBS), is a neuro-modulatory technique currently under investigation for the treatment of neurodegenerative diseases.