Related Research Articles

Antidepressants are a class of medications used to treat major depressive disorder, anxiety disorders, chronic pain, and addiction.

A psychiatric or psychotropic medication is a psychoactive drug taken to exert an effect on the chemical makeup of the brain and nervous system. Thus, these medications are used to treat mental illnesses. These medications are typically made of synthetic chemical compounds and are usually prescribed in psychiatric settings, potentially involuntarily during commitment. Since the mid-20th century, such medications have been leading treatments for a broad range of mental disorders and have decreased the need for long-term hospitalization, thereby lowering the cost of mental health care. The recidivism or rehospitalization of the mentally ill is at a high rate in many countries, and the reasons for the relapses are under research.

Sertraline, sold under the brand name Zoloft among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. The efficacy of sertraline for depression is similar to that of other antidepressants, and the differences are mostly confined to side effects. Sertraline is better tolerated than the older tricyclic antidepressants. Sertraline is effective for panic disorder, social anxiety disorder, generalized anxiety disorder (GAD), and obsessive–compulsive disorder (OCD). However, for OCD, cognitive behavioral therapy, particularly in combination with sertraline, is a better treatment. Although approved for post-traumatic stress disorder (PTSD), sertraline leads to only modest improvement in this condition. Sertraline also alleviates the symptoms of premenstrual dysphoric disorder (PMDD) and can be used in sub-therapeutic doses or intermittently for its treatment.
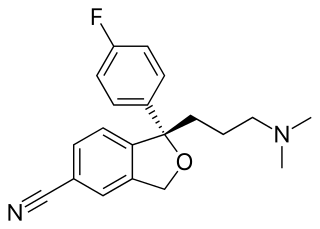
Escitalopram, sold under the brand names Lexapro and Cipralex, among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. Escitalopram is mainly used to treat major depressive disorder and generalized anxiety disorder. It is taken by mouth, available commercially as an oxalate salt exclusively.

Citalopram, sold under the brand name Celexa among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. It is used to treat major depressive disorder, obsessive compulsive disorder, panic disorder, and social phobia. The antidepressant effects may take one to four weeks to occur. It is typically taken orally. In some European countries, it is sometimes given intravenously to initiate treatment, before switching to the oral route of administration for continuation of treatment. It has also been used intravenously in other parts of the world in some other circumstances.

Venlafaxine, sold under the brand name Effexor among others, is an antidepressant medication of the serotonin-norepinephrine reuptake inhibitor (SNRI) class. It is used to treat major depressive disorder, generalized anxiety disorder, panic disorder, and social anxiety disorder. Studies have shown that Venlafaxine improves quality of life. It may also be used for chronic pain. It is taken by mouth. It is also available as the salt venlafaxine besylate in an extended-release formulation.

Mirtazapine, sold under the brand name Remeron amongst others, is an atypical tetracyclic antidepressant, and as such is used primarily to treat depression. Its effects may take up to four weeks, but can also manifest as early as one to two weeks. It is often used in cases of depression complicated by anxiety or insomnia. The effectiveness of mirtazapine is comparable to other commonly prescribed antidepressants. It is taken by mouth.

Serotonin–norepinephrine reuptake inhibitors (SNRIs) are a class of antidepressant medications used to treat major depressive disorder (MDD), anxiety disorders, obsessive–compulsive disorder (OCD), social phobia, attention-deficit hyperactivity disorder (ADHD), chronic neuropathic pain, fibromyalgia syndrome (FMS), and menopausal symptoms. SNRIs are monoamine reuptake inhibitors; specifically, they inhibit the reuptake of serotonin and norepinephrine. These neurotransmitters are thought to play an important role in mood regulation. SNRIs can be contrasted with the selective serotonin reuptake inhibitors (SSRIs) and norepinephrine reuptake inhibitors (NRIs), which act upon single neurotransmitters.

Generalized anxiety disorder (GAD) is a mental and behavioral disorder, specifically an anxiety disorder characterized by excessive, uncontrollable and often irrational worry about events or activities. Worry often interferes with daily functioning, and individuals with GAD are often overly concerned about everyday matters such as health, finances, death, family, relationship concerns, or work difficulties. Symptoms may include excessive worry, restlessness, trouble sleeping, exhaustion, irritability, sweating, and trembling.
Double depression refers to the co-existence of major depressive disorder (MDD) and persistent depressive disorder (PDD),. Research has shown that double depression tends to be more severe than either MDD or PDD alone and that individuals with double depression experience relapse more often than those with either MDD or PDD alone. However, there is some research that indicates few differences exist between double depression, MDD, and PDD; as a result, those researchers conclude that double depression is not a distinct disorder.
Dysthymia, also known as persistent depressive disorder (PDD), is a mental and behavioral disorder, specifically a disorder primarily of mood, consisting of similar cognitive and physical problems as major depressive disorder, but with longer-lasting symptoms. The concept was used by Robert Spitzer as a replacement for the term "depressive personality" in the late 1970s.
Atypical depression is defined in the DSM IV as depression that shares many of the typical symptoms of major depressive disorder or dysthymia but is characterized by improved mood in response to positive events. In contrast to those with atypical depression, people with melancholic depression generally do not experience an improved mood in response to normally pleasurable events. Atypical depression also often features significant weight gain or an increased appetite, hypersomnia, a heavy sensation in the limbs, and interpersonal rejection sensitivity that results in significant social or occupational impairment.

Psychotic depression, also known as depressive psychosis, is a major depressive episode that is accompanied by psychotic symptoms. It can occur in the context of bipolar disorder or major depressive disorder. It can be difficult to distinguish from schizoaffective disorder, a diagnosis that requires the presence of psychotic symptoms for at least two weeks without any mood symptoms present. Unipolar psychotic depression requires that psychotic symptoms occur during severe depressive episodes, although residual psychotic symptoms may also be present in between episodes. Diagnosis using the DSM-5 involves meeting the criteria for a major depressive episode, along with the criteria for "mood-congruent or mood-incongruent psychotic features" specifier.
The cognitive behavioral analysis system of psychotherapy (CBASP) is a talking therapy, a synthesis model of interpersonal and cognitive and behavioral therapies developed by James P. McCullough Jr. of Virginia Commonwealth University specifically for the treatment of all varieties of DSM-IV chronic depression. McCullough writes that chronic depression, particularly the type beginning during adolescence (early-onset), is essentially a refractory mood disorder arising from traumatic experiences or interpersonal psychological insults delivered by the patient's significant others.
The number of new psychiatric drugs, and especially antidepressants on the market in Japan, is significantly less than Western countries.
Treatment of chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) is variable and uncertain, and the condition is primarily managed rather than cured.
Management of depression is the treatment of depression that may involve a number of different therapies: medications, behavior therapy, psychotherapy, and medical devices.

Depression is a mental disorder characterized by prolonged unhappiness or irritability. It is accompanied by a constellation of somatic and cognitive signs and symptoms such as fatigue, apathy, sleep problems, loss of appetite, loss of engagement, low self-regard/worthlessness, difficulty concentrating or indecisiveness, or recurrent thoughts of death or suicide.

Selective serotonin reuptake inhibitors (SSRIs) are a class of drugs that are typically used as antidepressants in the treatment of major depressive disorder, anxiety disorders, and other psychological conditions.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 Sinyor M, Schaffer A, Levitt A (2010). "The Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Trial: A Review". The Canadian Journal of Psychiatry. 55 (3): 126–135. doi:10.1177/070674371005500303. PMID 20370962. S2CID 19442084.
- ↑ Insel, Thomas R., M.D. (2006). "Beyond Efficacy: The STAR*D Trial". Blog Publication by the NIMH Director. National Institute of Mental Health. 163 (1): 5–7. doi:10.1176/appi.ajp.163.1.5. PMC 1586101 . PMID 16390879. Archived from the original on 2014-04-04. Retrieved 4 April 2014.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ BS, Amanda Stevens (2023-02-10). "Does Adderall Help With Depression?". New Waters Recovery. Retrieved 2023-04-15.
- 1 2 3 4 5 6 7 8 9 Howland RH (2008). "Sequenced Treatment Alternatives to Relieve Depression (STAR*D)--Part 2: Study Outcomes". Journal of Psychosocial Nursing and Mental Health Services. 46 (10): 21–24. doi:10.3928/02793695-20081001-05. PMID 18935932.
- ↑ "STAR*D: Latest News". Project website for NIMH-funded collaborative study on the treatment of depression. University of Pittsburgh. Archived from the original on 5 March 2013. Retrieved 10 February 2013.
- 1 2 3 Pigott, H. E. (2011). STAR*D: A tale and trail of bias Ethical Human Psychology and Psychiatry: An International Journal of Critical Inquiry, 13(1), 6-28. https://doi.org/10.1891/1559-4343.13.1.6.
- ↑ Robert Whitaker (2010) The STAR*D Scandal: A New Paper Sums It All Up Psychology Today "Thus, if the study protocol had been followed and the results honestly reported, the researchers would have announced that 38% of the patients remitted during the four steps of treatment, and that the remaining 62% either dropped out or failed to remit."
- ↑ Leventhal, A. M., & Antonuccio, D. O. (2009). On chemical imbalances, antidepressants, and the diagnosis of depression. Ethical Human Psychology and Psychiatry, 11(3), 199. DOI: https://doi.org/10.1891/1559-4343.11.3.199 "Although the study’s reports make no mention of this outcome, their data show that after a year of continuation treatment following remission, of the 4,041 patients who entered the program only 108 (3%) had a sustained remission — all the other patients either dropped out or relapsed" p. 205, pdf p. 7.