Cerebrospinal fluid (CSF) is a clear, colorless body fluid found within the tissue that surrounds the brain and spinal cord of all vertebrates.
Idiopathic intracranial hypertension (IIH), previously known as pseudotumor cerebri and benign intracranial hypertension, is a condition characterized by increased intracranial pressure without a detectable cause. The main symptoms are headache, vision problems, ringing in the ears, and shoulder pain. Complications may include vision loss.

Syringomyelia is a generic term referring to a disorder in which a cyst or cavity forms within the spinal cord. Often, syringomyelia is used as a generic term before an etiology is determined. This cyst, called a syrinx, can expand and elongate over time, destroying the spinal cord. The damage may result in loss of feeling, paralysis, weakness, and stiffness in the back, shoulders, and extremities. Syringomyelia may also cause a loss of the ability to feel extremes of hot or cold, especially in the hands. It may also lead to a cape-like bilateral loss of pain and temperature sensation along the upper chest and arms. The combination of symptoms varies from one patient to another depending on the location of the syrinx within the spinal cord, as well as its extent.

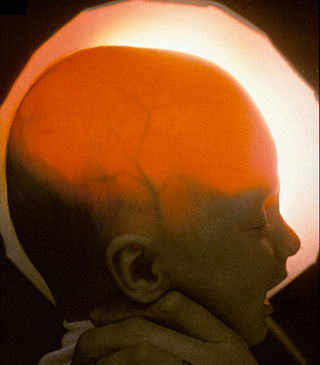
Hydrocephalus is a condition in which an accumulation of cerebrospinal fluid (CSF) occurs within the brain. This typically causes increased pressure inside the skull. Older people may have headaches, double vision, poor balance, urinary incontinence, personality changes, or mental impairment. In babies, it may be seen as a rapid increase in head size. Other symptoms may include vomiting, sleepiness, seizures, and downward pointing of the eyes.

Chiari malformation (CM) is a structural defect in the cerebellum, characterized by a downward displacement of one or both cerebellar tonsils through the foramen magnum. CMs can cause headaches, difficulty swallowing, vomiting, dizziness, neck pain, unsteady gait, poor hand coordination, numbness and tingling of the hands and feet, and speech problems. Less often, people may experience ringing or buzzing in the ears, weakness, slow heart rhythm, or fast heart rhythm, curvature of the spine (scoliosis) related to spinal cord impairment, abnormal breathing, such as central sleep apnea, characterized by periods of breathing cessation during sleep, and, in severe cases, paralysis.
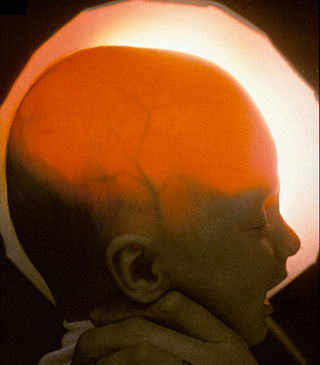
Hydranencephaly is a condition in which the brain's cerebral hemispheres are absent to a great degree and the remaining cranial cavity is filled with cerebrospinal fluid. "Cephalic" is the scientific term for "head" or "head end of body".

Lumbar puncture (LP), also known as a spinal tap, is a medical procedure in which a needle is inserted into the spinal canal, most commonly to collect cerebrospinal fluid (CSF) for diagnostic testing. The main reason for a lumbar puncture is to help diagnose diseases of the central nervous system, including the brain and spine. Examples of these conditions include meningitis and subarachnoid hemorrhage. It may also be used therapeutically in some conditions. Increased intracranial pressure is a contraindication, due to risk of brain matter being compressed and pushed toward the spine. Sometimes, lumbar puncture cannot be performed safely. It is regarded as a safe procedure, but post-dural-puncture headache is a common side effect if a small atraumatic needle is not used.
Normal-pressure hydrocephalus (NPH), also called malresorptive hydrocephalus, is a form of communicating hydrocephalus in which excess cerebrospinal fluid (CSF) occurs in the ventricles, and with normal or slightly elevated cerebrospinal fluid pressure. As the fluid builds up, it causes the ventricles to enlarge and the pressure inside the head to increase, compressing surrounding brain tissue and leading to neurological complications. The disease presents in a classic triad of symptoms, which are memory impairment, urinary frequency, and balance problems/gait deviations. The disease was first described by Salomón Hakim and Adams in 1965.

Arachnoid cysts are cerebrospinal fluid covered by arachnoidal cells and collagen that may develop between the surface of the brain and the cranial base or on the arachnoid membrane, one of the three meningeal layers that cover the brain and the spinal cord. Primary arachnoid cysts are a congenital disorder whereas secondary arachnoid cysts are the result of head injury or trauma. Most cases of primary cysts begin during infancy; however, onset may be delayed until adolescence.

Dandy–Walker malformation (DWM), also known as Dandy–Walker syndrome (DWS), is a rare congenital brain malformation in which the part joining the two hemispheres of the cerebellum does not fully form, and the fourth ventricle and space behind the cerebellum are enlarged with cerebrospinal fluid. Most of those affected develop hydrocephalus within the first year of life, which can present as increasing head size, vomiting, excessive sleepiness, irritability, downward deviation of the eyes and seizures. Other, less common symptoms are generally associated with comorbid genetic conditions and can include congenital heart defects, eye abnormalities, intellectual disability, congenital tumours, other brain defects such as agenesis of the corpus callosum, skeletal abnormalities, an occipital encephalocele or underdeveloped genitalia or kidneys. It is sometimes discovered in adolescents or adults due to mental health problems.

Choroid plexus papilloma, also known as papilloma of the choroid plexus, is a rare benign neuroepithelial intraventricular WHO grade I lesion found in the choroid plexus. It leads to increased cerebrospinal fluid production, thus causing increased intracranial pressure and hydrocephalus.

A colloid cyst is a non-malignant tumor in the brain. It consists of a gelatinous material contained within a membrane of epithelial tissue. It is almost always found just posterior to the foramen of Monro in the anterior aspect of the third ventricle, originating from the roof of the ventricle. Because of its location, it can cause obstructive hydrocephalus and increased intracranial pressure. Colloid cysts represent 0.5–1.0% of intracranial tumors.

A cerebral shunt is a device permanently implanted inside the head and body to drain excess fluid away from the brain. They are commonly used to treat hydrocephalus, the swelling of the brain due to excess buildup of cerebrospinal fluid (CSF). If left unchecked, the excess CSF can lead to an increase in intracranial pressure (ICP), which can cause intracranial hematoma, cerebral edema, crushed brain tissue or herniation. The drainage provided by a shunt can alleviate or prevent these problems in patients with hydrocephalus or related diseases.

An external ventricular drain (EVD), also known as a ventriculostomy or extraventricular drain, is a device used in neurosurgery to treat hydrocephalus and relieve elevated intracranial pressure when the normal flow of cerebrospinal fluid (CSF) inside the brain is obstructed. An EVD is a flexible plastic catheter placed by a neurosurgeon or neurointensivist and managed by intensive care unit (ICU) physicians and nurses. The purpose of external ventricular drainage is to divert fluid from the ventricles of the brain and allow for monitoring of intracranial pressure. An EVD must be placed in a center with full neurosurgical capabilities, because immediate neurosurgical intervention can be needed if a complication of EVD placement, such as bleeding, is encountered.

The CSF tap test, sometimes lumbar tap test or Miller Fisher Test, is a medical test that is used to decide whether shunting of cerebrospinal fluid (CSF) would be helpful in a patient with suspected normal pressure hydrocephalus (NPH). The test involves removing 30-50 ml of cerebrospinal fluid (CSF) through a lumbar puncture, after which motor and cognitive function is clinically reassessed. The name "Fisher test" is after C. Miller Fisher, a Canadian neurologist working in Boston, Massachusetts, who described the test.

Pineoblastoma is a malignant tumor of the pineal gland. A pineoblastoma is a supratentorial midline primitive neuroectodermal tumor. Pineoblastoma can present at any age, but is most common in young children. They account for 0.001% of all primary CNS neoplasms.
Bobble-head doll syndrome is a rare neurological movement disorder in which patients, usually children around age 3, begin to bob their head and shoulders forward and back, or sometimes side-to-side, involuntarily, in a manner reminiscent of a bobblehead doll. The syndrome is related to cystic lesions and swelling of the third ventricle in the brain. Symptoms of bobble-head doll syndrome are diverse but can be grouped into two categories: physical and neurological. The most common form of treatment is surgical implanting of a shunt to relieve the swelling of the brain.

Aqueductal stenosis is a narrowing of the aqueduct of Sylvius which blocks the flow of cerebrospinal fluid (CSF) in the ventricular system. Blockage of the aqueduct can lead to hydrocephalus, specifically as a common cause of congenital and/or obstructive hydrocephalus.

L1 syndrome is a group of mild to severe X-linked recessive disorders that share a common genetic basis. The spectrum of L1 syndrome disorders includes X-linked complicated corpus callosum dysgenesis, spastic paraplegia 1, MASA syndrome, and X-linked hydrocephalus with stenosis of the aqueduct of Sylvius (HSAS). It is also called L1CAM syndrome and CRASH syndrome, an acronym for its primary clinical features: corpus callosum hypoplasia, retardation, adducted thumbs, spasticity, and hydrocephalus.
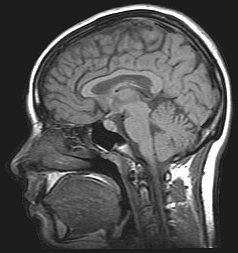
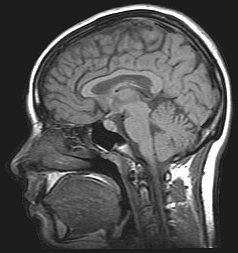
Cerebrospinal fluid (CSF) flow MRI is used to assess pulsatile CSF flow both qualitatively and quantitatively. Time-resolved 2D phase-contrast MRI with velocity encoding is the most common method for CSF analysis. CSF Fluid Flow MRI detects back and forth flow of Cerebrospinal fluid that corresponds to vascular pulsations from mostly the cardiac cycle of the choroid plexus. Bulk transport of CSF, characterized by CSF circulation through the Central Nervous System, is not used because it is too slow to assess clinically. CSF would have to pass through the brain's lymphatic system and be absorbed by arachnoid granulations.