Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes inside the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body. MRI does not involve X-rays or the use of ionizing radiation, which distinguishes it from computed tomography (CT) and positron emission tomography (PET) scans. MRI is a medical application of nuclear magnetic resonance (NMR) which can also be used for imaging in other NMR applications, such as NMR spectroscopy.
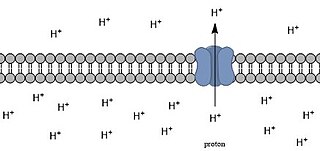
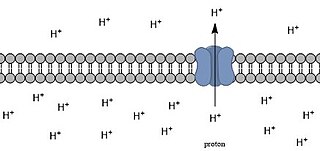
Intracellular pH (pHi) is the measure of the acidity or basicity of intracellular fluid. The pHi plays a critical role in membrane transport and other intracellular processes. In an environment with the improper pHi, biological cells may have compromised function. Therefore, pHi is closely regulated in order to ensure proper cellular function, controlled cell growth, and normal cellular processes. The mechanisms that regulate pHi are usually considered to be plasma membrane transporters of which two main types exist — those that are dependent and those that are independent of the concentration of bicarbonate. Physiologically normal intracellular pH is most commonly between 7.0 and 7.4, though there is variability between tissues. There is also pH variation across different organelles, which can span from around 4.5 to 8.0. pHi can be measured in a number of different ways.
Graham Wiggins was an American musician and scientist. He played the didgeridoo, keyboards, melodica, sampler, and various percussion instruments with his groups, the Oxford-based Outback and Dr. Didg. He also developed new technologies for magnetic resonance imaging (MRI).
Diffusion-weighted magnetic resonance imaging is the use of specific MRI sequences as well as software that generates images from the resulting data that uses the diffusion of water molecules to generate contrast in MR images. It allows the mapping of the diffusion process of molecules, mainly water, in biological tissues, in vivo and non-invasively. Molecular diffusion in tissues is not random, but reflects interactions with many obstacles, such as macromolecules, fibers, and membranes. Water molecule diffusion patterns can therefore reveal microscopic details about tissue architecture, either normal or in a diseased state. A special kind of DWI, diffusion tensor imaging (DTI), has been used extensively to map white matter tractography in the brain.

Prostate biopsy is a procedure in which small hollow needle-core samples are removed from a man's prostate gland to be examined for the presence of prostate cancer. It is typically performed when the result from a PSA blood test is high. It may also be considered advisable after a digital rectal exam (DRE) finds possible abnormality. PSA screening is controversial as PSA may become elevated due to non-cancerous conditions such as benign prostatic hyperplasia (BPH), by infection, or by manipulation of the prostate during surgery or catheterization. Additionally many prostate cancers detected by screening develop so slowly that they would not cause problems during a man's lifetime, making the complications due to treatment unnecessary.

High-intensity focused ultrasound (HIFU) is a non-invasive therapeutic technique that uses non-ionizing ultrasonic waves to heat or ablate tissue. HIFU can be used to increase the flow of blood or lymph or to destroy tissue, such as tumors, via thermal and mechanical mechanisms. Given the prevalence and relatively low cost of ultrasound generation mechanisms, the premise of HIFU is that it is expected to be a non-invasive and low-cost therapy that can at least outperform care in the operating room.
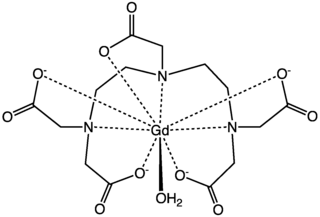
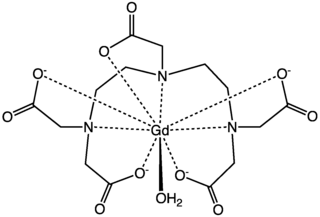
Gadopentetic acid, sold under the brand name Magnevist, is a gadolinium-based MRI contrast agent.
Magnetic resonance elastography (MRE) is a form of elastography that specifically leverages MRI to quantify and subsequently map the mechanical properties of soft tissue. First developed and described at Mayo Clinic by Muthupillai et al. in 1995, MRE has emerged as a powerful, non-invasive diagnostic tool, namely as an alternative to biopsy and serum tests for staging liver fibrosis.
During nuclear magnetic resonance observations, spin–lattice relaxation is the mechanism by which the longitudinal component of the total nuclear magnetic moment vector (parallel to the constant magnetic field) exponentially relaxes from a higher energy, non-equilibrium state to thermodynamic equilibrium with its surroundings (the "lattice"). It is characterized by the spin–lattice relaxation time, a time constant known as T1.
MRI contrast agents are contrast agents used to improve the visibility of internal body structures in magnetic resonance imaging (MRI). The most commonly used compounds for contrast enhancement are gadolinium-based contrast agents (GBCAs). Such MRI contrast agents shorten the relaxation times of nuclei within body tissues following oral or intravenous administration.
In vivo magnetic resonance spectroscopy (MRS) is a specialized technique associated with magnetic resonance imaging (MRI).
Preclinical imaging is the visualization of living animals for research purposes, such as drug development. Imaging modalities have long been crucial to the researcher in observing changes, either at the organ, tissue, cell, or molecular level, in animals responding to physiological or environmental changes. Imaging modalities that are non-invasive and in vivo have become especially important to study animal models longitudinally. Broadly speaking, these imaging systems can be categorized into primarily morphological/anatomical and primarily molecular imaging techniques. Techniques such as high-frequency micro-ultrasound, magnetic resonance imaging (MRI) and computed tomography (CT) are usually used for anatomical imaging, while optical imaging, positron emission tomography (PET), and single photon emission computed tomography (SPECT) are usually used for molecular visualizations.
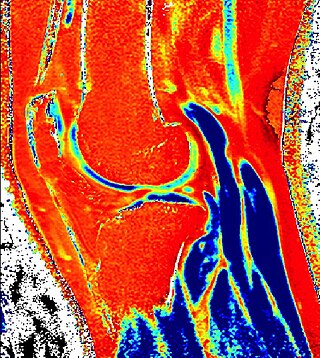
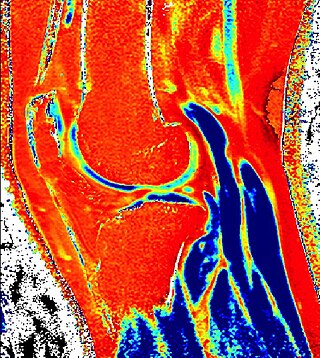
Delayed gadolinium-enhanced magnetic resonance imaging of cartilage or dGEMRIC measures the fixed-charge density and relative proteoglycan content of articular cartilage using the spin-lattice relaxation time or T1 relaxation time. Current research is investigating the clinical application of dGEMRIC as a quantitative tool for monitoring cartilage function in diseased or repair cartilage.

Magnetic resonance imaging of the brain uses magnetic resonance imaging (MRI) to produce high quality two-dimensional or three-dimensional images of the brain and brainstem as well as the cerebellum without the use of ionizing radiation (X-rays) or radioactive tracers.
Functional magnetic resonance spectroscopy of the brain (fMRS) uses magnetic resonance imaging (MRI) to study brain metabolism during brain activation. The data generated by fMRS usually shows spectra of resonances, instead of a brain image, as with MRI. The area under peaks in the spectrum represents relative concentrations of metabolites.

Perfusion MRI or perfusion-weighted imaging (PWI) is perfusion scanning by the use of a particular MRI sequence. The acquired data are then post-processed to obtain perfusion maps with different parameters, such as BV, BF, MTT and TTP.
In the field of medicine, radiomics is a method that extracts a large number of features from medical images using data-characterisation algorithms. These features, termed radiomic features, have the potential to uncover tumoral patterns and characteristics that fail to be appreciated by the naked eye. The hypothesis of radiomics is that the distinctive imaging features between disease forms may be useful for predicting prognosis and therapeutic response for various cancer types, thus providing valuable information for personalized therapy. Radiomics emerged from the medical fields of radiology and oncology and is the most advanced in applications within these fields. However, the technique can be applied to any medical study where a pathological process can be imaged.
The history of magnetic resonance imaging (MRI) includes the work of many researchers who contributed to the discovery of nuclear magnetic resonance (NMR) and described the underlying physics of magnetic resonance imaging, starting early in the twentieth century. One researcher was American physicist Isidor Isaac Rabi who won the Nobel Prize in Physics in 1944 for his discovery of nuclear magnetic resonance, which is used in magnetic resonance imaging. MR imaging was invented by Paul C. Lauterbur who developed a mechanism to encode spatial information into an NMR signal using magnetic field gradients in September 1971; he published the theory behind it in March 1973.

An MRI pulse sequence in magnetic resonance imaging (MRI) is a particular setting of pulse sequences and pulsed field gradients, resulting in a particular image appearance.
Michael Albert Thomas is an Indian-American physicist, academic, and clinical researcher. He is a Professor-in-Residence of Radiological Sciences, and Psychiatry at the Geffen School of Medicine, University of California, Los Angeles (UCLA). He is most known for developing novel single voxel based 2D NMR techniques, multi-voxel 2D MRS techniques using hybrid Cartesian as well as non-Cartesian spatio-temporal encoding such as concentric ring, radial and rosette trajectories.