This article may be too technical for most readers to understand.(June 2008) |
Tissue-to-air ratio (TAR) is a term used in radiotherapy treatment planning to help calculate absorbed dose to water in conditions other than those directly measured.
This article may be too technical for most readers to understand.(June 2008) |
Tissue-to-air ratio (TAR) is a term used in radiotherapy treatment planning to help calculate absorbed dose to water in conditions other than those directly measured.
The TAR at a point in a water phantom irradiated by a photon beam is taken to be the ratio of the total absorbed dose at that point to the absorbed dose at the same point in a minimal-scatter phantom with just-sufficient build-up. [1] [2]
Tissue-air ratio is defined as the ratio of the dose to water at a given depth to the dose in air measured with a buildup cap:
where D(f,z) is the dose at a given depth z and distance focus-detector f; and D(f,0) is the dose in air (z=0).
Measurements for each are taken using an ion chamber for identical source to detector distances and field sizes. [3]

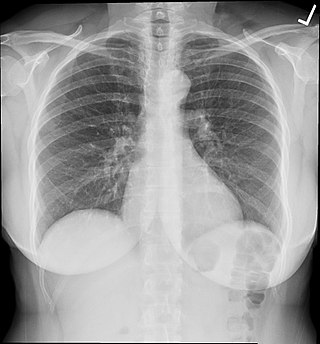
X-ray radiation, or, much less commonly, X-radiation, is a penetrating form of high-energy electromagnetic radiation. Most X-rays have a wavelength ranging from 10 nanometers to 10 picometers, corresponding to frequencies in the range 30 petahertz to 30 exahertz (3×1016 Hz to 3×1019 Hz) and energies in the range 124 keV to 145 eV, respectively. X-ray wavelengths are shorter than those of UV rays and typically longer than those of gamma rays. In many languages, X-radiation is referred to as Röntgen radiation, after the German scientist Wilhelm Conrad Röntgen, who discovered it on November 8, 1895. He named it X-radiation to signify an unknown type of radiation. Spellings of X-ray(s) in English include the variants x-ray(s), xray(s), and X ray(s).

In physics, optical depth or optical thickness is the natural logarithm of the ratio of incident to transmitted radiant power through a material. Thus, the larger the optical depth, the smaller the amount of transmitted radiant power through the material. Spectral optical depth or spectral optical thickness is the natural logarithm of the ratio of incident to transmitted spectral radiant power through a material. Optical depth is dimensionless, and in particular is not a length, though it is a monotonically increasing function of optical path length, and approaches zero as the path length approaches zero. The use of the term "optical density" for optical depth is discouraged.
In physics, attenuation is the gradual loss of flux intensity through a medium. For instance, dark glasses attenuate sunlight, lead attenuates X-rays, and water and air attenuate both light and sound at variable attenuation rates.

The sievert is a unit in the International System of Units (SI) intended to represent the stochastic health risk of ionizing radiation, which is defined as the probability of causing radiation-induced cancer and genetic damage. The sievert is important in dosimetry and radiation protection. It is named after Rolf Maximilian Sievert, a Swedish medical physicist renowned for work on radiation dose measurement and research into the biological effects of radiation.

External beam radiation therapy (EBRT) is a compound word that refers to the use of a collimated beam of ionizing radiation from outside the body to treat a disease.
The gray is the unit of ionizing radiation dose in the International System of Units (SI), defined as the absorption of one joule of radiation energy per kilogram of matter.
Radiation dosimetry in the fields of health physics and radiation protection is the measurement, calculation and assessment of the ionizing radiation dose absorbed by an object, usually the human body. This applies both internally, due to ingested or inhaled radioactive substances, or externally due to irradiation by sources of radiation.
Absorbed dose is a dose quantity which is the measure of the energy deposited in matter by ionizing radiation per unit mass. Absorbed dose is used in the calculation of dose uptake in living tissue in both radiation protection, and radiology. It is also used to directly compare the effect of radiation on inanimate matter such as in radiation hardening.

In medicine, proton therapy, or proton radiotherapy, is a type of particle therapy that uses a beam of protons to irradiate diseased tissue, most often to treat cancer. The chief advantage of proton therapy over other types of external beam radiotherapy is that the dose of protons is deposited over a narrow range of depth; hence in minimal entry, exit, or scattered radiation dose to healthy nearby tissues.
A monitor unit (MU) is a measure of machine output from a clinical accelerator for radiation therapy such as a linear accelerator or an orthovoltage unit. Monitor units are measured by monitor chambers, which are ionization chambers that measure the dose delivered by a beam and are built into the treatment head of radiotherapy linear accelerators.
The ionization chamber is the simplest type of gaseous ionisation detector, and is widely used for the detection and measurement of many types of ionizing radiation, including X-rays, gamma rays, alpha particles and beta particles. Conventionally, the term "ionization chamber" refers exclusively to those detectors which collect all the charges created by direct ionization within the gas through the application of an electric field. It uses the discrete charges created by each interaction between the incident radiation and the gas to produce an output in the form of a small direct current. This means individual ionising events cannot be measured, so the energy of different types of radiation cannot be differentiated, but it gives a very good measurement of overall ionising effect.
Elastic recoil detection analysis (ERDA), also referred to as forward recoil scattering, is an ion beam analysis technique in materials science to obtain elemental concentration depth profiles in thin films. This technique is known by several different names. These names are listed below. In the technique of ERDA, an energetic ion beam is directed at a sample to be characterized and there is an elastic nuclear interaction between the ions of beam and the atoms of the target sample. Such interactions are commonly of Coulomb nature. Depending on the kinetics of the ions, cross section area, and the loss of energy of the ions in the matter, ERDA helps determine the quantification of the elemental analysis. It also provides information about the depth profile of the sample.

In external beam Radiotherapy, transverse and longitudinal dose measurements are taken by a radiation detector in order to characterise the radiation beams from medical linear accelerators. Typically, an ionisation chamber and water phantom are used to create these radiation dose profiles. Water is used due to its tissue equivalence.

In radiotherapy, radiation treatment planning (RTP) is the process in which a team consisting of radiation oncologists, radiation therapist, medical physicists and medical dosimetrists plan the appropriate external beam radiotherapy or internal brachytherapy treatment technique for a patient with cancer.
Particle therapy is a form of external beam radiotherapy using beams of energetic neutrons, protons, or other heavier positive ions for cancer treatment. The most common type of particle therapy as of August 2021 is proton therapy.
In radiotherapy, a percentage depth dose curve (PDD) relates the absorbed dose deposited by a radiation beam into a medium as it varies with depth along the axis of the beam. The dose values are divided by the maximum dose, referred to as dmax, yielding a plot in terms of percentage of the maximum dose. Dose measurements are generally made in water or "water equivalent" plastic with an ionization chamber, since water is very similar to human tissue with regard to radiation scattering and absorption.
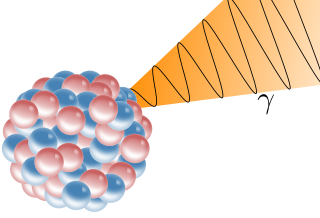
A gamma ray, also known as gamma radiation (symbol γ or ), is a penetrating form of electromagnetic radiation arising from the radioactive decay of atomic nuclei. It consists of the shortest wavelength electromagnetic waves, typically shorter than those of X-rays. With frequencies above 30 exahertz (3×1019 Hz), it imparts the highest photon energy. Paul Villard, a French chemist and physicist, discovered gamma radiation in 1900 while studying radiation emitted by radium. In 1903, Ernest Rutherford named this radiation gamma rays based on their relatively strong penetration of matter; in 1900 he had already named two less penetrating types of decay radiation (discovered by Henri Becquerel) alpha rays and beta rays in ascending order of penetrating power.
In radiation therapy, bolus is a material which has properties equivalent to tissue when irradiated. It is widely used in practice to reduce or alter dosing for targeted radiation therapy.
The computed tomography dose index (CTDI) is a commonly used radiation exposure index in X-ray computed tomography (CT), first defined in 1981. The unit of CTDI is the gray (Gy) and it can be used in conjunction with patient size to estimate the absorbed dose. The CTDI and absorbed dose may differ by more than a factor of two for small patients such as children.
In medical imaging, an anti-scatter grid is a device for limiting the amount of scattered radiation reaching the detector, thereby improving the quality of diagnostic medical x-ray images. The grid is positioned on the opposite side of the patient from the x-ray source, and between the patient and the X-ray detector or film. Reducing the amount of scattered x-rays increases the image's contrast resolution, and consequently the visibility of soft tissues.