Related Research Articles
Ataxia is a neurological sign consisting of lack of voluntary coordination of muscle movements that can include gait abnormality, speech changes, and abnormalities in eye movements, that indicates dysfunction of parts of the nervous system that coordinate movement, such as the cerebellum.

Peripheral neuropathy, often - and rightly so - shortened to neuropathy, refers to damage or disease affecting the nerves. Damage to nerves may impair sensation, movement, gland function, and/or organ function depending on which nerves are affected. Neuropathies affecting motor, sensory, or autonomic nerves result in different symptoms. More than one type of nerve may be affected simultaneously. Peripheral neuropathy may be acute or chronic, and may be reversible or permanent.

Polyneuropathy is damage or disease affecting peripheral nerves in roughly the same areas on both sides of the body, featuring weakness, numbness, and burning pain. It usually begins in the hands and feet and may progress to the arms and legs and sometimes to other parts of the body where it may affect the autonomic nervous system. It may be acute or chronic. A number of different disorders may cause polyneuropathy, including diabetes and some types of Guillain–Barré syndrome.

Alcoholic polyneuropathy is a neurological disorder in which peripheral nerves throughout the body malfunction simultaneously. It is defined by axonal degeneration in neurons of both the sensory and motor systems and initially occurs at the distal ends of the longest axons in the body. This nerve damage causes an individual to experience pain and motor weakness, first in the feet and hands and then progressing centrally. Alcoholic polyneuropathy is caused primarily by chronic alcoholism; however, vitamin deficiencies are also known to contribute to its development. This disease typically occurs in chronic alcoholics who have some sort of nutritional deficiency. Treatment may involve nutritional supplementation, pain management, and abstaining from alcohol.

Tropical spastic paraparesis (TSP), is a medical condition that causes weakness, muscle spasms, and sensory disturbance by human T-lymphotropic virus resulting in paraparesis, weakness of the legs. As the name suggests, it is most common in tropical regions, including the Caribbean. Blood transfusion products are screened for human T-lymphotropic virus 1 (HTLV-1) antibodies, as a preventive measure.

Neuritis, from the Greek νεῦρον), is inflammation of a nerve or the general inflammation of the peripheral nervous system. Inflammation, and frequently concomitant demyelination, cause impaired transmission of neural signals and leads to aberrant nerve function. Neuritis is often conflated with neuropathy, a broad term describing any disease process which affects the peripheral nervous system. However, neuropathies may be due to either inflammatory or non-inflammatory causes, and the term encompasses any form of damage, degeneration, or dysfunction, while neuritis refers specifically to the inflammatory process.

Behr syndrome is characterized by the association of early-onset optic atrophy with spinocerebellar degeneration resulting in ataxia, pyramidal signs, peripheral neuropathy and developmental delay.
Dominant optic atrophy (DOA), or autosomal dominant optic atrophy (ADOA), (Kjer's type) is an autosomally inherited disease that affects the optic nerves, causing reduced visual acuity and blindness beginning in childhood. However, the disease can seem to re-present a second time with further vision loss due to the early onset of presbyopia symptoms (i.e., difficulty in viewing objects up close). DOA is characterized as affecting neurons called retinal ganglion cells (RGCs). This condition is due to mitochondrial dysfunction mediating the death of optic nerve fibers. The RGCs axons form the optic nerve. Therefore, the disease can be considered of the central nervous system. Dominant optic atrophy was first described clinically by Batten in 1896 and named Kjer’s optic neuropathy in 1959 after Danish ophthalmologist Poul Kjer, who studied 19 families with the disease. Although dominant optic atrophy is the most common autosomally inherited optic neuropathy (i.e., disease of the optic nerves), it is often misdiagnosed.
Chronic inflammatory demyelinating polyneuropathy (CIDP) is an acquired autoimmune disease of the peripheral nervous system characterized by progressive weakness and impaired sensory function in the legs and arms. The disorder is sometimes called chronic relapsing polyneuropathy (CRP) or chronic inflammatory demyelinating polyradiculoneuropathy. CIDP is closely related to Guillain–Barré syndrome and it is considered the chronic counterpart of that acute disease. Its symptoms are also similar to progressive inflammatory neuropathy. It is one of several types of neuropathy.
Toxic and nutritional optic neuropathy is a group of medical disorders defined by visual impairment due to optic nerve damage secondary to a toxic substance and/or nutritional deficiency. The causes of these disorders are various, but they are linked by shared signs and symptoms, which this article will describe. In several of these disorders, both toxic and nutritional factors play a role, acting synergistically.

MERRF syndrome is a mitochondrial disease. It is extremely rare, and has varying degrees of expressivity owing to heteroplasmy. MERRF syndrome affects different parts of the body, particularly the muscles and nervous system. The signs and symptoms of this disorder appear at an early age, generally childhood or adolescence. The causes of MERRF syndrome are difficult to determine, but because it is a mitochondrial disorder, it can be caused by the mutation of nuclear DNA or mitochondrial DNA. The classification of this disease varies from patient to patient, since many individuals do not fall into one specific disease category. The primary features displayed on a person with MERRF include myoclonus, seizures, cerebellar ataxia, myopathy, and ragged red fibers (RRF) on muscle biopsy, leading to the disease's name. Secondary features include dementia, optic atrophy, bilateral deafness, peripheral neuropathy, spasticity, or multiple lipomata. Mitochondrial disorders, including MERRFS, may present at any age.

Konzo is an epidemic paralytic disease occurring among hunger-stricken rural populations in Africa where a diet dominated by insufficiently processed cassava results in simultaneous malnutrition and high dietary cyanide intake. Konzo was first described by Giovanni Trolli in 1938 who compiled the observations from eight doctors working in the Kwango area of the Belgian Congo.
Copper deficiency, or hypocupremia, is defined either as insufficient copper to meet the needs of the body, or as a serum copper level below the normal range. Symptoms may include fatigue, decreased red blood cells, early greying of the hair, and neurological problems presenting as numbness, tingling, muscle weakness, and ataxia. The neurodegenerative syndrome of copper deficiency has been recognized for some time in ruminant animals, in which it is commonly known as "swayback". Copper deficiency can manifest in parallel with vitamin B12 and other nutritional deficiencies.
Mitohondrial optic neuropathies are a heterogenous group of disorders that present with visual disturbances resultant from mitochondrial dysfunction within the anatomy of the Retinal Ganglion Cells (RGC), optic nerve, optic chiasm, and optic tract. These disturbances are multifactorial, their aetiology consisting of metabolic and/or structural damage as a consequence of genetic mutations, environmental stressors, or both. The three most common neuro-ophthalmic abnormalities seen in mitochondrial disorders are bilateral optic neuropathy, ophthalmoplegia with ptosis, and pigmentary retinopathy.

Arts syndrome is a rare metabolic disorder that causes serious neurological problems in males due to a malfunction of the PRPP synthetase 1 enzyme. Arts Syndrome is part of a spectrum of PRPS-1 related disorders with reduced activity of the enzyme that includes Charcot–Marie–Tooth disease and X-linked non-syndromic sensorineural deafness.
Megavitamin-B6 syndrome is a collection of symptoms that can result from chronic supplementation, or acute overdose, of vitamin B6. While it is also known as hypervitaminosis B6, vitamin B6 toxicity and vitamin B6 excess, megavitamin-b6 syndrome is the name used in the ICD-10.
Tropical neuropathy is a class of illnesses with similar signs and symptoms, including konzo, tropical spastic paraparesis (TSP), and tropical ataxic neuropathy (TAN). TAN is poorly understood, and some researchers subdivide it further into separate illnesses.
Sensory ataxic neuropathy, dysarthria, and ophthalmoparesis, also known as SANDO syndrome, is a very rare genetic disorder which is characterized by ocular and nerve anomalies.
CAPOS syndrome is a rare genetic neurological disorder which is characterized by abnormalities of the feet, eyes and brain which affect their normal function. These symptoms occur episodically when a fever-related infection is present within the body. The name is an acronym for "cerebellar ataxia, areflexia, pes cavus, optic atrophy, and sensorineural hearing loss".
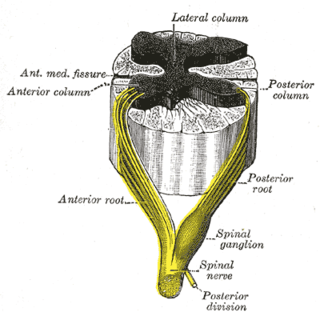
Sensory neuronopathy is a type of peripheral neuropathy that results primarily in sensory symptoms due to destruction of nerve cell bodies in the dorsal root ganglion. The causes of nerve damage are grouped into categories including those due to paraneoplastic causes, immune mediated, infectious, inherited or degenerative causes and those due to toxin exposure. In idiopathic sensory neuronopathy no cause is identified. Idiopathic causes account for about 50% of cases. Sensory neuronopathy differs from the more common length dependent axonal polyneuropathies in that the symptoms do not progress in a distal to proximal pattern, rather symptoms develop in a multifocal, asymmetric, and non-length dependent manner. Ataxia is a prominent symptom early in the disease course. The trigeminal nerve ganglion is also commonly affected leading to facial numbness. Motor nerves are usually not affected however some cases do have mild motor involvement in the form of weakness. Symptoms tend to develop sub-acutely, over weeks, in acquired sensory neuronopathy and more slowly in inherited or primary degenerative cases. In cases of paraneoplastic or infectious sensory neuropathy, treatment is directed at the underlying cancer or infectious cause respectively. Immunomodulatory and anti-inflammatory therapies are also commonly used however their effectiveness is limited.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Netto, AB; Netto, CM; Mahadevan, A; Taly, AB; Agadi, JB (2016). "Tropical ataxic neuropathy - A century old enigma". Neurology India. 64 (6): 1151–1159. doi: 10.4103/0028-3886.193755 . PMID 27841178.
- ↑ Pryse-Phillips, William (2009). "Strachan-Scott Syndrome". Companion to Clinical Neurology. Oxford University Press. p. 966. ISBN 978-0-19-971004-1 . Retrieved 12 March 2020.
- 1 2 Trivedi, S; Pandit, A; Ganguly, G; Das, SK (July–September 2017). "Epidemiology of Peripheral Neuropathy: An Indian Perspective". Annals of Indian Academy of Neurology. 20 (3): 173–184. doi: 10.4103/aian.AIAN_470_16 . PMC 5586108 . PMID 28904445.
- ↑ Adamolekun, B (March 2011). "Neurological disorders associated with cassava diet: a review of putative etiological mechanisms". Metabolic Brain Disease. 26 (1): 79–85. doi:10.1007/s11011-011-9237-y. PMID 21327546. S2CID 19377135.
- ↑ Robson, D; Welch, E; Beeching, NJ; Gill, GV (February 2009). "Consequences of captivity: health effects of far East imprisonment in World War II". QJM: Monthly Journal of the Association of Physicians. 102 (2): 87–96. doi: 10.1093/qjmed/hcn137 . PMID 18854350.
- ↑ "Tropical ataxic neuropathy". British Medical Journal. 3 (5619): 632–3. 14 September 1968. doi:10.1136/bmj.3.5663.178-a. PMC 1986522 . PMID 5673206.
- ↑ Román, GC; Spencer, PS; Schoenberg, BS (August 1985). "Tropical myeloneuropathies: the hidden endemias". Neurology. 35 (8): 1158–70. doi:10.1212/wnl.35.8.1158. PMID 2991814. S2CID 20850916.