Related Research Articles
The management of HIV/AIDS normally includes the use of multiple antiretroviral drugs as a strategy to control HIV infection. There are several classes of antiretroviral agents that act on different stages of the HIV life-cycle. The use of multiple drugs that act on different viral targets is known as highly active antiretroviral therapy (HAART). HAART decreases the patient's total burden of HIV, maintains function of the immune system, and prevents opportunistic infections that often lead to death. HAART also prevents the transmission of HIV between serodiscordant same-sex and opposite-sex partners so long as the HIV-positive partner maintains an undetectable viral load.

The United States President's Emergency Plan For AIDS Relief (PEPFAR) is a United States governmental initiative to address the global HIV/AIDS epidemic and help save the lives of those suffering from the disease. Launched by U.S. President George W. Bush in 2003, as of May 2020, PEPFAR has provided about $90 billion in cumulative funding for HIV/AIDS treatment, prevention, and research since its inception, making it the largest global health program focused on a single disease in history until the COVID-19 pandemic. PEPFAR is implemented by a combination of U.S. government agencies in over 50 countries and overseen by the Global AIDS Coordinator at the United States Department of State. As of 2023, PEPFAR has saved over 25 million lives, primarily in sub-Saharan Africa.
HIV/AIDS has been a public health concern for Latin America due to a remaining prevalence of the disease. In 2018 an estimated 2.2 million people had HIV in Latin America and the Caribbean, making the HIV prevalence rate approximately 0.4% in Latin America.

The global epidemic of HIV/AIDS began in 1981, and is an ongoing worldwide public health issue. According to the World Health Organization (WHO), as of 2021, HIV/AIDS has killed approximately 40.1 million people, and approximately 38.4 million people are infected with HIV globally. Of these 38.4 million people, 75% are receiving antiretroviral treatment. There were about 770,000 deaths from HIV/AIDS in 2018, and 650,000 deaths in 2021. The 2015 Global Burden of Disease Study estimated that the global incidence of HIV infection peaked in 1997 at 3.3 million per year. Global incidence fell rapidly from 1997 to 2005, to about 2.6 million per year. Incidence of HIV has continued to fall, decreasing by 23% from 2010 to 2020, with progress dominated by decreases in Eastern Africa and Southern Africa. As of 2020, there are approximately 1.5 million new infections of HIV per year globally.
The Division of Acquired Immunodeficiency Syndrome (DAIDS) is a division of the National Institute of Allergy and Infectious Diseases, which is part of the National Institutes of Health. It was formed in 1986 as a part of the initiative to address the national research needs created by the advent and spread of the HIV/AIDS epidemic. Specifically, the Division's mission is to increase basic knowledge of the pathogenesis, natural history, and transmission of HIV disease and to support research that promotes progress in its detection, treatment, and prevention. DAIDS accomplishes this through planning, implementing, managing, and evaluating programs in (1) fundamental basic research, (2) discovery and development of therapies for HIV infection and its complications, and (3) discovery and development of vaccines and other prevention strategies.

Jim Yong Kim, also known as Kim Yong (김용/金墉), is an American physician and anthropologist who served as the 12th president of the World Bank from 2012 to 2019.

Infection with HIV, a retrovirus, can be managed with treatment but without treatment can lead to a spectrum of conditions including AIDS.

As of 2012, approximately 1,100,000 people in Malawi are HIV-positive, which represents 10.8% of the country's population. Because the Malawian government was initially slow to respond to the epidemic under the leadership of Hastings Banda (1966–1994), the prevalence of HIV/AIDS increased drastically between 1985, when the disease was first identified in Malawi, and 1993, when HIV prevalence rates were estimated to be as high as 30% among pregnant women. The Malawian food crisis in 2002 resulted, at least in part, from a loss of agricultural productivity due to the prevalence of HIV/AIDS. Various degrees of government involvement under the leadership of Bakili Muluzi (1994–2004) and Bingu wa Mutharika (2004–2012) resulted in a gradual decline in HIV prevalence, and, in 2003, many people living in Malawi gained access to antiretroviral therapy. Condoms have become more widely available to the public through non-governmental organizations, and more Malawians are taking advantage of HIV testing services.
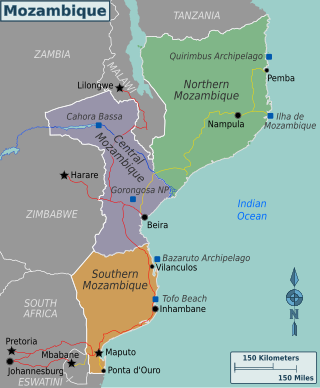
Mozambique is a country particularly hard-hit by the HIV/AIDS epidemic. According to 2008 UNAIDS estimates, this southeast African nation has the 8th highest HIV rate in the world. With 1,600,000 Mozambicans living with HIV, 990,000 of which are women and children, Mozambique's government realizes that much work must be done to eradicate this infectious disease. To reduce HIV/AIDS within the country, Mozambique has partnered with numerous global organizations to provide its citizens with augmented access to antiretroviral therapy and prevention techniques, such as condom use. A surge toward the treatment and prevention of HIV/AIDS in women and children has additionally aided in Mozambique's aim to fulfill its Millennium Development Goals (MDGs). Nevertheless, HIV/AIDS has made a drastic impact on Mozambique; individual risk behaviors are still greatly influenced by social norms, and much still needs to be done to address the epidemic and provide care and treatment to those in need.
UNAIDS has said that HIV/AIDS in Indonesia is one of Asia's fastest growing epidemics. In 2010, it is expected that 5 million Indonesians will have HIV/AIDS. In 2007, Indonesia was ranked 99th in the world by prevalence rate, but because of low understanding of the symptoms of the disease and high social stigma attached to it, only 5-10% of HIV/AIDS sufferers actually get diagnosed and treated. According to the a census conducted in 2019, it is counted that 640,443 people in the country are living with HIV. The adult prevalence for HIV/ AIDS in the country is 0.4%. Indonesia is the country is Southeast Asia to have the most number of recorded people living with HIV while Thailand has the highest adult prevalence.
The Philippines has one of the lowest rates of infection of HIV/AIDS, yet has one of the fastest growing number of cases worldwide. The Philippines is one of seven countries with growth in number of cases of over 25%, from 2001 to 2009.
Cases of HIV/AIDS in Peru are considered to have reached the level of a concentrated epidemic.
Teguest Guerma is an Ethiopian medical doctor specializing in public health and HIV/AIDS. Guerma is appointed by the African Medical and Research Foundation Board of Directors as Director General in June 2010. She has been the Associate Director of the HIV/AIDS Department of the World Health Organization between 2004–2010. She has started her career in HIV/AIDS in Burundi and has since extensively worked in Africa and South East Asia, including as country representative for the World Health Organization and Regional Advisor of HIV/AIDS for the Africa Regional Office of the WHO. She also represented the Africa Region of the World Health Organization at the United Nations headquarters in New York City from 2001–2004 and promoted African health issues, notably HIV/AIDS, tuberculosis and malaria, that has significantly contributed to their inclusion into resolution of the general assembly and the Security Council of the UN. She has been very instrumental in the establishment and initiation of a WHO and UNAIDS 3 by 5 Initiative. The 3 by 5 Initiative was a global target of putting 3 million people living with HIV on life saving antiretroviral treatment by end of 2005, which heralded a breakthrough to the access of HIV treatment in resource limited countries. She did her undergraduate degree in Doctor of Medicine at the University of Reims Champagne-Ardenne in France and post graduate public health trainings at the University of Dakar in Senegal and Johns Hopkins University in the United States.

Eric Goosby is an American public health official, currently serving as the UN Special Envoy on Tuberculosis. Goosby previously served as the United States Global AIDS Coordinator from 2009 until mid-November 2013. In the role, Goosby directed the U.S. strategy for addressing HIV around the world and led President Obama's implementation of the President's Emergency Plan for AIDS Relief (PEPFAR). Goosby was sworn in during June 2009 and resigned in November 2013, taking a position as a professor at UCSF, where he directs the Center for Global Health Delivery and Diplomacy, a collaboration between UCSF and the University of California, Berkeley.
HIV drug resistance occurs when microevolution causes virions to become tolerant to antiretroviral treatments (ART). ART can be used to successfully manage HIV infection, but a number of factors can contribute to the virus mutating and becoming resistant. Drug resistance occurs as bacterial or viral populations evolve to no longer respond to medications that previously worked. In the case of HIV, there have been recognized cases of treatment resistant strains since 1989, with drug resistance being a major contributor to treatment failure. While global incidence varies greatly from region to region, there has been a general increase in overall HIV drug resistance. The two main types of resistance, primary and induced, differ mostly in causation, with the biggest cause of resistance being a lack of adherence to the specific details of treatment. These newly created resistant strains of HIV pose a public health issue as they infect a growing number of people because they are harder to treat, and can be spread to other individuals. For this reason, the reaction to the growing number of cases of resistant HIV strains has mostly been to try to increase access to treatment and implement other measures to make sure people stay in care, as well as to look into the development of an HIV vaccine or cure.
The first HIV/AIDS case in Malaysia made its debut in 1986. Since then, HIV/AIDS has become one of the country's most serious health and development challenges. As of 2020, the Ministry of Health estimated that 87 per cent of an estimated 92,063 people living with HIV (PLHIV) in Malaysia were aware of their status, 58 per cent of reported PLHIV received antiretroviral therapy, and 85 per cent of those on antiretroviral treatment became virally suppressed. Despite making positive progress, Malaysia still fell short of meeting the global 2020 HIV goals of 90-90-90, with a scorecard of 87-58-85.
Global Health Initiatives (GHIs) are humanitarian initiatives that raise and disburse additional funds for infectious diseases – such as AIDS, tuberculosis, and malaria – for immunizations and for strengthening health systems in developing countries. GHIs classify a type of global initiative, which is defined as an organized effort integrating the involvement of organizations, individuals, and stakeholders around the world to address a global issue.
The cost of HIV treatment is a complicated issue with an extremely wide range of costs due to varying factors such as the type of antiretroviral therapy and the country in which the treatment is administered. The first line therapy of HIV, or the initial antiretroviral drug regimen for an HIV-infected patient, is generally cheaper than subsequent second-line or third-line therapies. There is also a great variability of drug prices among low, middle, and high income countries. In general, low-income countries have the lowest cost of antiretroviral therapy, while middle- and high-income tend to have considerably higher costs. Certain prices of HIV drugs may be high and difficult to afford due to patent barriers on antiretroviral drugs and slow regulatory approval for drugs, which may lead to indirect consequences such as greater HIV drug resistance and an increased number of opportunistic infections. Government and activist movements have taken efforts to limit the price of HIV drugs.
Julio S. G. Montaner, is an Argentine-Canadian physician, professor and researcher. He is the director of the British Columbia Centre for Excellence in HIV/AIDS, the chair in AIDS Research and head of the Division of AIDS in the Faculty of Medicine at the University of British Columbia and the past-president of the International AIDS Society. He is also the director of the John Ruedy Immunodeficiency Clinic, and the Physician Program Director for HIV/AIDS PHC. He is known for his work on HAART, a role in the discovery of triple therapy as an effective treatment for HIV in the late 1990s, and a role in advocating the "Treatment as Prevention" Strategy in the mid-2000s, led by Myron Cohen of the HPTN 052 trial.
Treatment as prevention (TasP) is a concept in public health that promotes treatment as a way to prevent and reduce the likelihood of HIV illness, death and transmission from an infected individual to others. Expanding access to earlier HIV diagnosis and treatment as a means to address the global epidemic by preventing illness, death and transmission was first proposed in 2000 by Garnett et al. The term is often used to talk about treating people that are currently living with human immunodeficiency virus (HIV) and acquired immune deficiency syndrome (AIDS) to prevent illness, death and transmission. Although some experts narrow this to only include preventing infections, treatment prevents illnesses such as tuberculosis and has been shown to prevent death. In relation to HIV, antiretroviral therapy (ART) is a three or more drug combination therapy that is used to decrease the viral load, or the measured amount of virus, in an infected individual. Such medications are used as a preventative for infected individuals to not only spread the HIV virus to their negative partners but also improve their current health to increase their lifespans. When taken correctly, ART is able to diminish the presence of the HIV virus in the bodily fluids of an infected person to a level of undetectability. Consistent adherence to an ARV regimen, monitoring, and testing are essential for continued confirmed viral suppression. Treatment as prevention rose to great prominence in 2011, as part of the HPTN 052 study, which shed light on the benefits of early treatment for HIV positive individuals.
References
- ↑ "The 3 by 5 Initiative". World Health Organization. Retrieved May 2, 2016.
- 1 2 3 4 Maria Ines Battistella Nemes; et al. (2006). "EVALUATION OF WHO's CONTRIBUTION TO "3 BY 5": Main Report" (PDF). World Health Organization. Retrieved May 2, 2016.
- ↑ "Treating 3 million by 2005: Making it happen - The WHO Strategy" (PDF). World Health Organization. 2003. Retrieved May 2, 2016.
- ↑ Kim, Jim Yong; Ammann, Arthur (November 30, 2004). "Is the "3 by 5" Initiative the Best Approach to Tackling the HIV Pandemic?". PLOS Medicine. 1 (2): e37. doi: 10.1371/journal.pmed.0010037 . PMC 529425 . PMID 15578107.