Related Research Articles
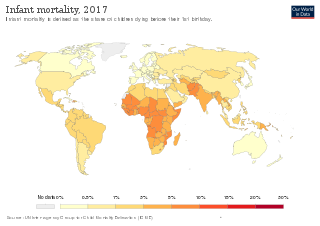
Infant mortality is the death of an infant before the infant's first birthday. The occurrence of infant mortality in a population can be described by the infant mortality rate (IMR), which is the number of deaths of infants under one year of age per 1,000 live births. Similarly, the child mortality rate, also known as the under-five mortality rate, compares the death rate of children up to the age of five.
Health equity arises from access to the social determinants of health, specifically from wealth, power and prestige. Individuals who have consistently been deprived of these three determinants are significantly disadvantaged from health inequities, and face worse health outcomes than those who are able to access certain resources. It is not equity to simply provide every individual with the same resources; that would be equality. In order to achieve health equity, resources must be allocated based on an individual need-based principle.
The Whitehall Studies investigated social determinants of health, specifically the cardiovascular disease prevalence and mortality rates among British civil servants. The initial prospective cohort study, the Whitehall I Study, examined over 17,500 male civil servants between the ages of 20 and 64, and was conducted over a period of ten years, beginning in 1967. A second cohort study, the Whitehall II Study, was conducted from 1985 to 1988 and examined the health of 10,308 civil servants aged 35 to 55, of whom two thirds were men and one third women. A long-term follow-up of study subjects from the first two phases is ongoing.

Population health has been defined as "the health outcomes of a group of individuals, including the distribution of such outcomes within the group". It is an approach to health that aims to improve the health of an entire human population. It has been described as consisting of three components. These are "health outcomes, patterns of health determinants, and policies and interventions".

Screening, in medicine, is a strategy used to look for as-yet-unrecognised conditions or risk markers. This testing can be applied to individuals or to a whole population without symptoms or signs of the disease being screened.

Sir Michael Gideon Marmot is Professor of Epidemiology and Public Health at University College London. He is currently the Director of The UCL Institute of Health Equity. Marmot has led research groups on health inequalities for over thirty years, working for various international and governmental bodies. In 2023, he was elected to the American Philosophical Society.

The social determinants of health (SDOH) are the economic and social conditions that influence individual and group differences in health status. They are the health promoting factors found in one's living and working conditions, rather than individual risk factors that influence the risk or vulnerability for a disease or injury. The distribution of social determinants is often shaped by public policies that reflect prevailing political ideologies of the area.
The Black Report was a 1980 document published by the Department of Health and Social Security in the United Kingdom, which was the report of the expert committee into health inequality chaired by Sir Douglas Black. It was demonstrated that although, in general, health had improved since the introduction of the welfare state, there were widespread health inequalities. It also found that the main cause of these inequalities was economic inequality. The report showed that the death rate for men in social class V was twice that for men in social class I and that gap between the two was increasing, not reducing as was expected.

Richard Gerald Wilkinson is a British social epidemiologist, author, advocate, and left-wing political activist. He is Professor Emeritus of social epidemiology at the University of Nottingham, having retired in 2008. He is also Honorary Professor of Epidemiology and Public Health at University College London and Visiting Professor at University of York. In 2009, Richard co-founded The Equality Trust. Richard was awarded a 2013 Silver Rose Award from Solidar for championing equality and the 2014 Charles Cully Memorial Medal by the Irish Cancer Society.

The Wolfson Research Institute for Health and Wellbeing is an interdisciplinary research centre within Durham University. It is based at the university's Queen's Campus in Thornaby, Stockton-on-Tees.

Social medicine is an interdisciplinary field that focuses on the profound interplay between socio-economic factors and individual health outcomes. Rooted in the challenges of the Industrial Revolution, it seeks to:
- Understand how specific social, economic, and environmental conditions directly impact health, disease, and the delivery of medical care.
- Promote conditions and interventions that address these determinants, aiming for a healthier and more equitable society.

In medicine, rural health or rural medicine is the interdisciplinary study of health and health care delivery in rural environments. The concept of rural health incorporates many fields, including wilderness medicine, geography, midwifery, nursing, sociology, economics, and telehealth or telemedicine.

Danny Dorling is a British social geographer. Since 2013, he has been Halford Mackinder Professor of Geography of the School of Geography and the Environment of the University of Oxford.

Public Health England (PHE) was an executive agency of the Department of Health and Social Care in England which began operating on 1 April 2013 to protect and improve health and wellbeing and reduce health inequalities. Its formation came as a result of the reorganisation of the National Health Service (NHS) in England outlined in the Health and Social Care Act 2012. It took on the role of the Health Protection Agency, the National Treatment Agency for Substance Misuse and a number of other health bodies. It was an executive agency of the Department of Health and Social Care, and a distinct delivery organisation with operational autonomy.
The social determinants of health in poverty describe the factors that affect impoverished populations' health and health inequality. Inequalities in health stem from the conditions of people's lives, including living conditions, work environment, age, and other social factors, and how these affect people's ability to respond to illness. These conditions are also shaped by political, social, and economic structures. The majority of people around the globe do not meet their potential best health because of a "toxic combination of bad policies, economics, and politics". Daily living conditions work together with these structural drivers to result in the social determinants of health.

EuroHealthNet is a non-profit partnership of organisations, agencies and statutory bodies working to contribute to a healthier Europe by promoting health and health equity between and within European countries. EuroHealthNet promotes health through its partnership framework by supporting members’ work in the EU and associated states through policy and project development, networking, and communications.
Black maternal mortality in the United States refers to the disproportionately high rate of maternal death among those who identify as Black or African American women. Maternal death is often linked to both direct obstetric complications and indirect obstetric deaths that exacerbate pre-existing health conditions. In general, the Centers for Disease Control and Prevention defines maternal mortality as a death occurring within 42 days of the end of pregnancy from any cause related to or aggravated by the pregnancy or its management. In the United States, around 700 women die from pregnancy-related complications per year, with Black women facing a mortality rate nearly three times more than the rate for white women.

The COVID-19 pandemic has revealed race-based health care disparities in many countries, including the United States, United Kingdom, Norway, Sweden, Canada, and Singapore. These disparities are believed to originate from structural racism in these countries which pre-dates the pandemic; a commentary in The BMJ noted that "ethnoracialised differences in health outcomes have become the new normal across the world" as a result of ethnic and racial disparities in COVID-19 healthcare, determined by social factors. Data from the United States and elsewhere shows that minorities, especially black people, have been infected and killed at a disproportionate rate to white people.
There are various factors affecting the health of ethnic minorities in the UK due to health inequalities. The term "BAME" is often used however, the use of this term can be problematic for various reasons, such as an indicating power relations and also having a focus on skin colour. Therefore, this article will use the term ethnic minorities.

The Office for Health Improvement and Disparities (OHID) is a government unit within the Department of Health and Social Care that leads national efforts to improve public health policy across England.
References
- ↑ Graham, H., Understanding Health Inequalities, (2000), Open University Press
- ↑ Committee of Inquiry into the Future Development of the Public Health Function, Acheson, D., Public health in England: The Report of the Committee of Inquiry into the Future Development to the Public Health Function, (1988), ISBN 978-0101028929
- ↑ Isaacs, J.D., Stephen L. and Steven A. Schroeder. "Class - The Ignored Determinant of the Nation's Health". New England Journal of Medicine 351.11 (Sep 2004), 1137-1142.
- ↑ Black & al, Inequalities in Health, (1990), Penguin
- ↑ The Stationery Office, Our Healthier Nation, (1998)
- ↑ Ray Earwicker (2007). "Progress in tackling health inequalities: a policy maker's reflections". In Dowler, Elizabeth; Spencer, Nick J. (eds.). Challenging health inequalities: from Acheson to 'Choosing Health' . Bristol: Policy Press. p. 17. ISBN 978-1861348999.
- ↑ Bambra, Clare (2016). Health Divides. Bristol: Policy Press. pp. 192–7. ISBN 9781447330356 . Retrieved 30 December 2016.