Related Research Articles

Antidepressants are a class of medications used to treat major depressive disorder, anxiety disorders, chronic pain, and addiction.

Major depressive disorder (MDD), also known as clinical depression, is a mental disorder characterized by at least two weeks of pervasive low mood, low self-esteem, and loss of interest or pleasure in normally enjoyable activities. Introduced by a group of US clinicians in the mid-1970s, the term was adopted by the American Psychiatric Association for this symptom cluster under mood disorders in the 1980 version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), and has become widely used since. The disorder causes the second-most years lived with disability, after lower back pain.

Serotonin or 5-hydroxytryptamine (5-HT) is a monoamine neurotransmitter. Its biological function is complex, touching on diverse functions including mood, cognition, reward, learning, memory, and numerous physiological processes such as vomiting and vasoconstriction.

Tryptophan (symbol Trp or W) is an α-amino acid that is used in the biosynthesis of proteins. Tryptophan contains an α-amino group, an α-carboxylic acid group, and a side chain indole, making it a polar molecule with a non-polar aromatic beta carbon substituent. Tryptophan is also a precursor to the neurotransmitter serotonin, the hormone melatonin, and vitamin B3. It is encoded by the codon UGG.

Sertraline, sold under the brand name Zoloft among others, is an antidepressant of the selective serotonin reuptake inhibitor (SSRI) class. The effectiveness of sertraline for depression is similar to that of other antidepressants, and the differences are mostly confined to side effects. Sertraline is better tolerated than the older tricyclic antidepressants. Sertraline is effective for panic disorder, social anxiety disorder, generalized anxiety disorder (GAD), and obsessive–compulsive disorder (OCD). Although approved for post-traumatic stress disorder (PTSD), sertraline leads to only modest improvement in this condition. Sertraline also alleviates the symptoms of premenstrual dysphoric disorder (PMDD) and can be used in sub-therapeutic doses or intermittently for its treatment.

The serotonin transporter also known as the sodium-dependent serotonin transporter and solute carrier family 6 member 4 is a protein that in humans is encoded by the SLC6A4 gene. SERT is a type of monoamine transporter protein that transports the neurotransmitter serotonin from the synaptic cleft back to the presynaptic neuron, in a process known as serotonin reuptake.

Depression is a mental state of low mood and aversion to activity. It affects more than 280 million people of all ages. Depression affects a person's thoughts, behavior, feelings, and sense of well-being. Depressed people often experience loss of motivation or interest in, or reduced pleasure or joy from, experiences that would normally bring them pleasure or joy.

Beck's cognitive triad, also known as the negative triad, is a cognitive-therapeutic view of the three key elements of a person's belief system present in depression. It was proposed by Aaron Beck in 1967. The triad forms part of his cognitive theory of depression and the concept is used as part of CBT, particularly in Beck's "Treatment of Negative Automatic Thoughts" (TNAT) approach.
Wake therapy is a specific application of intentional sleep deprivation. It encompasses many sleep-restricting paradigms that aim to address mood disorders with a form of non-pharmacological therapy.

Tryptophan hydroxylase 2 (TPH2) is an isozyme of tryptophan hydroxylase found in vertebrates. In humans, TPH2 is primarily expressed in the serotonergic neurons of the brain, with the highest expression in the raphe nucleus of the midbrain. Until the discovery of TPH2 in 2003, serotonin levels in the central nervous system were believed to be regulated by serotonin synthesis in peripheral tissues, in which tryptophan hydroxylase is the dominant form.

Fenclonine, also known as para-chlorophenylalanine (PCPA), acts as a selective and irreversible inhibitor of tryptophan hydroxylase, which is a rate-limiting enzyme in the biosynthesis of serotonin.
5-HTTLPR is a degenerate repeat polymorphic region in SLC6A4, the gene that codes for the serotonin transporter. Since the polymorphism was identified in the middle of the 1990s, it has been extensively investigated, e.g., in connection with neuropsychiatric disorders. A 2006 scientific article stated that "over 300 behavioral, psychiatric, pharmacogenetic and other medical genetics papers" had analyzed the polymorphism. While often discussed as an example of gene-environment interaction, this contention is contested.
Management of depression is the treatment of depression that may involve a number of different therapies: medications, behavior therapy, psychotherapy, and medical devices.
Scientific studies have found that different brain areas show altered activity in humans with major depressive disorder (MDD), and this has encouraged advocates of various theories that seek to identify a biochemical origin of the disease, as opposed to theories that emphasize psychological or situational causes. Factors spanning these causative groups include nutritional deficiencies in magnesium, vitamin D, and tryptophan with situational origin but biological impact. Several theories concerning the biologically based cause of depression have been suggested over the years, including theories revolving around monoamine neurotransmitters, neuroplasticity, neurogenesis, inflammation and the circadian rhythm. Physical illnesses, including hypothyroidism and mitochondrial disease, can also trigger depressive symptoms.
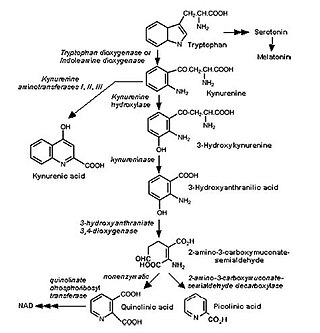
The kynurenine pathway is a metabolic pathway leading to the production of nicotinamide adenine dinucleotide (NAD+). Metabolites involved in the kynurenine pathway include tryptophan, kynurenine, kynurenic acid, xanthurenic acid, quinolinic acid, and 3-hydroxykynurenine. The kynurenine pathway is responsible for about 95% of total tryptophan catabolism. Disruption in the pathway is associated with certain genetic and psychiatric disorders.

Selective serotonin reuptake inhibitors (SSRIs) are a class of drugs that are typically used as antidepressants in the treatment of major depressive disorder, anxiety disorders, and other psychological conditions.

Certain lithium compounds, also known as lithium salts, are used as psychiatric medication, primarily for bipolar disorder and for major depressive disorder. Lithium is taken orally.
The pharmacology of antidepressants is not entirely clear. The earliest and probably most widely accepted scientific theory of antidepressant action is the monoamine hypothesis, which states that depression is due to an imbalance of the monoamine neurotransmitters. It was originally proposed based on the observation that certain hydrazine anti-tuberculosis agents produce antidepressant effects, which was later linked to their inhibitory effects on monoamine oxidase, the enzyme that catalyses the breakdown of the monoamine neurotransmitters. All currently marketed antidepressants have the monoamine hypothesis as their theoretical basis, with the possible exception of agomelatine which acts on a dual melatonergic-serotonergic pathway. Despite the success of the monoamine hypothesis it has a number of limitations: for one, all monoaminergic antidepressants have a delayed onset of action of at least a week; and secondly, there are a sizeable portion (>40%) of depressed patients that do not adequately respond to monoaminergic antidepressants. Further evidence to the contrary of the monoamine hypothesis are the recent findings that a single intravenous infusion with ketamine, an antagonist of the NMDA receptor — a type of glutamate receptor — produces rapid, robust and sustained antidepressant effects. Monoamine precursor depletion also fails to alter mood. To overcome these flaws with the monoamine hypothesis a number of alternative hypotheses have been proposed, including the glutamate, neurogenic, epigenetic, cortisol hypersecretion and inflammatory hypotheses. Another hypothesis that has been proposed which would explain the delay is the hypothesis that monoamines don't directly influence mood, but influence emotional perception biases.

Bipolar disorder is an affective disorder characterized by periods of elevated and depressed mood. The cause and mechanism of bipolar disorder is not yet known, and the study of its biological origins is ongoing. Although no single gene causes the disorder, a number of genes are linked to increase risk of the disorder, and various gene environment interactions may play a role in predisposing individuals to developing bipolar disorder. Neuroimaging and postmortem studies have found abnormalities in a variety of brain regions, and most commonly implicated regions include the ventral prefrontal cortex and amygdala. Dysfunction in emotional circuits located in these regions have been hypothesized as a mechanism for bipolar disorder. A number of lines of evidence suggests abnormalities in neurotransmission, intracellular signalling, and cellular functioning as possibly playing a role in bipolar disorder.
Michael Pascal Hengartner is an academic psychologist at the Zurich University of Applied Sciences who has published on the subject of antidepressants and in other areas. In 2022, he published a book called Evidence-Biased Antidepressant Prescription: Overmedicalisation, Flawed Research, and Conflicts of Interest. He has also published with other notable researchers such as Joanna Moncrieff and Irving Kirsch.
References
- 1 2 3 van Donkelaar EL, Blokland A, Ferrington L, Kelly PA, Steinbusch HW, Prickaerts J (July 2011). "Mechanism of acute tryptophan depletion: is it only serotonin?". Molecular Psychiatry. 16 (7): 695–713. doi: 10.1038/mp.2011.9 . PMID 21339754.
- ↑ Young SN (September 2013). "Acute tryptophan depletion in humans: a review of theoretical, practical and ethical aspects". Journal of Psychiatry & Neuroscience. 38 (5): 294–305. doi:10.1503/jpn.120209. PMC 3756112 . PMID 23428157.
- ↑ Ruhé HG, Mason NS, Schene AH (April 2007). "Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies". Molecular Psychiatry. 12 (4): 331–59. doi:10.1038/sj.mp.4001949.
- ↑ Jauhar S, Arnone D, Baldwin DS, Bloomfield M, Browning M, Cleare AJ, Corlett P, Deakin JF, Erritzoe D, Fu C, Fusar-Poli P, Goodwin GM, Hayes J, Howard R, Howes OD, Juruena MF, Lam RW, Lawrie SM, McAllister-Williams H, Cowen PJ. "(2023). A leaky umbrella has little value: Evidence clearly indicates the serotonin system is implicated in depression". Molecular Psychiatry. 28 (8): 3149–52. doi:10.1038/s41380-023-02095-y. PMC 10618084 .