In multicellular organisms, stem cells are undifferentiated or partially differentiated cells that can change into various types of cells and proliferate indefinitely to produce more of the same stem cell. They are the earliest type of cell in a cell lineage. They are found in both embryonic and adult organisms, but they have slightly different properties in each. They are usually distinguished from progenitor cells, which cannot divide indefinitely, and precursor or blast cells, which are usually committed to differentiating into one cell type.

Hematopoietic stem-cell transplantation (HSCT) is the transplantation of multipotent hematopoietic stem cells, usually derived from bone marrow, peripheral blood, or umbilical cord blood, in order to replicate inside a patient and produce additional normal blood cells. HSCT may be autologous, syngeneic, or allogeneic.

Graft-versus-host disease (GvHD) is a syndrome, characterized by inflammation in different organs. GvHD is commonly associated with bone marrow transplants and stem cell transplants.
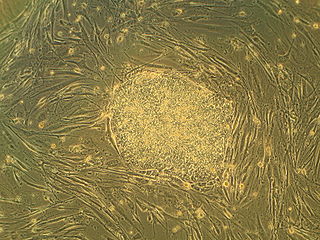
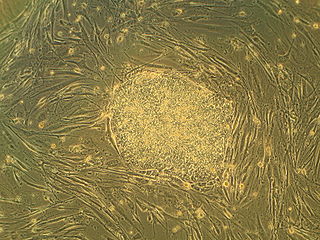
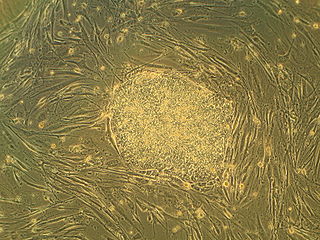
Embryonic stem cells (ESCs) are pluripotent stem cells derived from the inner cell mass of a blastocyst, an early-stage pre-implantation embryo. Human embryos reach the blastocyst stage 4–5 days post fertilization, at which time they consist of 50–150 cells. Isolating the inner cell mass (embryoblast) using immunosurgery results in destruction of the blastocyst, a process which raises ethical issues, including whether or not embryos at the pre-implantation stage have the same moral considerations as embryos in the post-implantation stage of development.
Regenerative medicine deals with the "process of replacing, engineering or regenerating human or animal cells, tissues or organs to restore or establish normal function". This field holds the promise of engineering damaged tissues and organs by stimulating the body's own repair mechanisms to functionally heal previously irreparable tissues or organs.

Homeobox protein NANOG(hNanog) is a transcriptional factor that helps embryonic stem cells (ESCs) maintain pluripotency by suppressing cell determination factors. hNanog is encoded in humans by the NANOG gene. Several types of cancer are associated with NANOG.

Adult stem cells are undifferentiated cells, found throughout the body after development, that multiply by cell division to replenish dying cells and regenerate damaged tissues. Also known as somatic stem cells, they can be found in juvenile, adult animals, and humans, unlike embryonic stem cells.

The stem cell controversy concerns the ethics of research involving the development and use of human embryos. Most commonly, this controversy focuses on embryonic stem cells. Not all stem cell research involves human embryos. For example, adult stem cells, amniotic stem cells, and induced pluripotent stem cells do not involve creating, using, or destroying human embryos, and thus are minimally, if at all, controversial. Many less controversial sources of acquiring stem cells include using cells from the umbilical cord, breast milk, and bone marrow, which are not pluripotent.
Stem-cell therapy uses stem cells to treat or prevent a disease or condition. As of 2024, the only FDA-approved therapy using stem cells is hematopoietic stem cell transplantation. This usually takes the form of a bone marrow or peripheral blood stem cell transplantation, but the cells can also be derived from umbilical cord blood. Research is underway to develop various sources for stem cells as well as to apply stem-cell treatments for neurodegenerative diseases and conditions such as diabetes and heart disease.

An organoid is a miniaturised and simplified version of an organ produced in vitro in three dimensions that mimics the key functional, structural, and biological complexity of that organ. It is derived from one or a few cells from a tissue, embryonic stem cells, or induced pluripotent stem cells, which can self-organize in three-dimensional culture owing to their self-renewal and differentiation capacities. The technique for growing organoids has rapidly improved since the early 2010s, and The Scientist named it one of the biggest scientific advancements of 2013. Scientists and engineers use organoids to study development and disease in the laboratory, for drug discovery and development in industry, personalized diagnostics and medicine, gene and cell therapies, tissue engineering, and regenerative medicine.

Anthony Atala is an American bioengineer, urologist, and pediatric surgeon. He is the W.H. Boyce professor of urology, the founding director of the Wake Forest Institute for Regenerative Medicine, and the chair of the Department of Urology at Wake Forest School of Medicine in North Carolina. His work focuses on the science of regenerative medicine: "a practice that aims to refurbish diseased or damaged tissue using the body's own healthy cells".

Induced pluripotent stem cells are a type of pluripotent stem cell that can be generated directly from a somatic cell. The iPSC technology was pioneered by Shinya Yamanaka and Kazutoshi Takahashi in Kyoto, Japan, who together showed in 2006 that the introduction of four specific genes, collectively known as Yamanaka factors, encoding transcription factors could convert somatic cells into pluripotent stem cells. Shinya Yamanaka was awarded the 2012 Nobel Prize along with Sir John Gurdon "for the discovery that mature cells can be reprogrammed to become pluripotent."
Amniotic stem cells are the mixture of stem cells that can be obtained from the amniotic fluid as well as the amniotic membrane. They can develop into various tissue types including skin, cartilage, cardiac tissue, nerves, muscle, and bone. The cells also have potential medical applications, especially in organ regeneration.
Adult mesenchymal stem cells are being used by researchers in the fields of regenerative medicine and tissue engineering to artificially reconstruct human tissue which has been previously damaged. Mesenchymal stem cells are able to differentiate, or mature from a less specialized cell to a more specialized cell type, to replace damaged tissues in various organs.
Cord lining, cord tissue, or umbilical cord lining membrane, is the outermost layer of the umbilical cord. As the umbilical cord itself is an extension of the placenta, the umbilical cord lining membrane is an extension of the amniotic membrane covering the placenta. The umbilical cord lining membrane comprises two layers: the amniotic layer and the sub-amniotic layer. The umbilical cord lining membrane is a rich source of two strains of stem cells (CLSCs): epithelial stem cells (CLECs) and mesenchymal stem cells (CLMCs). Discovered by Singapore-based CellResearch Corporation in 2004, this is the best known source for harvesting human stem cells.
Regeneration in humans is the regrowth of lost tissues or organs in response to injury. This is in contrast to wound healing, or partial regeneration, which involves closing up the injury site with some gradation of scar tissue. Some tissues such as skin, the vas deferens, and large organs including the liver can regrow quite readily, while others have been thought to have little or no capacity for regeneration following an injury.

Limbal stem cells, also known as corneal epithelial stem cells, are unipotent stem cells located in the basal epithelial layer of the corneal limbus. They form the border between the cornea and the sclera. Characteristics of limbal stem cells include a slow turnover rate, high proliferative potential, clonogenicity, expression of stem cell markers, as well as the ability to regenerate the entire corneal epithelium. Limbal stem cell proliferation has the role of maintaining the cornea; for example, by replacing cells that are lost via tears. Additionally, these cells also prevent the conjunctival epithelial cells from migrating onto the surface of the cornea.
Lorenz Studer is a Swiss biologist. He is the founder and director of the Center for Stem Cell Biology at Memorial-Sloan Kettering Cancer Center in New York City. He is a developmental biologist and neuroscientist who is pioneering the generation of midbrain dopamine neurons for transplantation and clinical applications. His expertise in cell engineering spans a wide range of cells/tissues within the nervous system geared toward disease modeling and exploring cell replacement therapy. Currently, he is a member of the Developmental Biology Program and Department of Neurosurgery at Memorial Sloan-Kettering Cancer Center and a professor of Neuroscience at Weill Cornell Medical College in New York City, NY.
Pregnancy-specific biological substances, which include the placenta, umbilical cord, amniotic fluid, and amniotic membrane are being studied for a number of health uses. For example, Placental-derived stem cells are being studied so they can serve as a potential treatment method for cell therapy. Hepatocyte-like cells (HLC) are generated from differentiated human amniotic epithelial cells (hAEC) that are abundant in the placenta. HLC may replace hepatocytes for hepatocyte transplantation to treat acute or chronic liver damage.

Stem cell therapy for macular degeneration is an emerging treatment approach aimed at restoring vision in individuals suffering from various forms of macular degeneration, particularly age-related macular degeneration (AMD). This therapy involves the transplantation of stem cells into the retina to replace damaged or lost retinal pigment epithelium (RPE) and photoreceptor cells, which are critical for central vision. Clinical trials have shown promise in stabilizing or improving visual function, but are nevertheless inefficient.