Related Research Articles

Epilepsy is a group of non-communicable neurological disorders characterized by recurrent epileptic seizures. An epileptic seizure is the clinical manifestation of an abnormal, excessive, and synchronized electrical discharge in the neurons. The occurrence of two or more unprovoked seizures defines epilepsy. The occurrence of just one seizure may warrant the definition in a more clinical usage where recurrence may be able to be prejudged. Epileptic seizures can vary from brief and nearly undetectable periods to long periods of vigorous shaking due to abnormal electrical activity in the brain. These episodes can result in physical injuries, either directly, such as broken bones, or through causing accidents. In epilepsy, seizures tend to recur and may have no detectable underlying cause. Isolated seizures that are provoked by a specific cause such as poisoning are not deemed to represent epilepsy. People with epilepsy may be treated differently in various areas of the world and experience varying degrees of social stigma due to the alarming nature of their symptoms.

A seizure is a sudden change in behavior, movement or consciousness due to abnormal electrical activity in the brain. Seizures can look different in different people. It can be uncontrolled shaking of the whole body or a person spacing out for a few seconds. Most seizures last less than two minutes. They are then followed by confusion/drowsiness before the person returns to normal. If a seizure lasts longer than 5 minutes, it is a medical emergency and needs immediate treatment.
Anticonvulsants are a diverse group of pharmacological agents used in the treatment of epileptic seizures. Anticonvulsants are also increasingly being used in the treatment of bipolar disorder and borderline personality disorder, since many seem to act as mood stabilizers, and for the treatment of neuropathic pain. Anticonvulsants suppress the excessive rapid firing of neurons during seizures. Anticonvulsants also prevent the spread of the seizure within the brain.
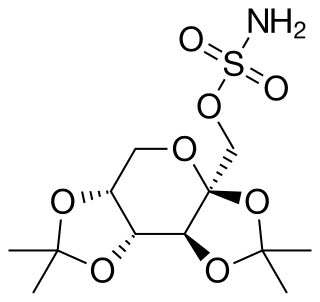
Topiramate, sold under the brand name Topamax among others, is a medication used to treat epilepsy and prevent migraines. It has also been used in alcohol dependence and essential tremor. For epilepsy this includes treatment for generalized or focal seizures. It is taken orally.

Lamotrigine, sold under the brand name Lamictal among others, is a medication used to treat epilepsy and stabilize mood in bipolar disorder. For epilepsy, this includes focal seizures, tonic-clonic seizures, and seizures in Lennox-Gastaut syndrome. In bipolar disorder, lamotrigine has not been shown to reliably treat acute depression in any groups except for the severely depressed; but for patients with bipolar disorder who are not currently symptomatic, it appears to reduce the risk of future episodes of depression.
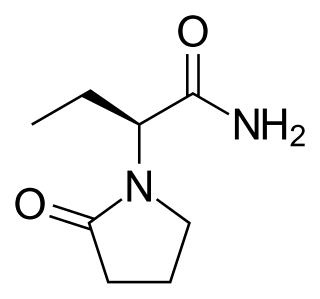
Levetiracetam, sold under the brand name Keppra among others, is a novel antiepileptic drug (medication) used to treat epilepsy. It is used for partial-onset, myoclonic, or tonic–clonic seizures, and is taken either by mouth as an immediate or extended release formulation or by injection into a vein.
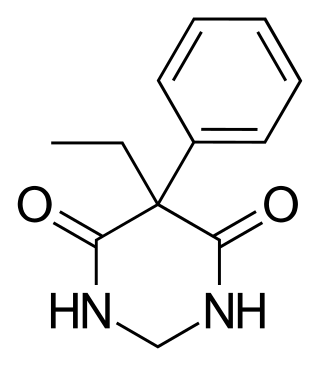
Primidone, sold under various brand names, is a barbiturate medication that is used to treat partial and generalized seizures and essential tremors. It is taken by mouth.
Long-term or "continuous" video-electroencephalography (EEG) monitoring is a diagnostic technique commonly used in patients with epilepsy. It involves the long-term hospitalization of the patient, typically for days or weeks, during which brain waves are recorded via EEG and physical actions are continuously monitored by video. In epileptic patients, this technique is typically used to capture brain activity during seizures. The information gathered can be used for initial prognosis or long-term care management.
Sudden unexpected death in epilepsy (SUDEP) is a fatal complication of epilepsy. It is defined as the sudden and unexpected, non-traumatic and non-drowning death of a person with epilepsy, without a toxicological or anatomical cause of death detected during the post-mortem examination.
Racine stages are a categorization of rodent epileptic seizures proposed by Ronald J. Racine in 1972. Prior to Racine's research in animal epilepsy models, a quantifiable means to describe seizure intensities and their causes was not readily available. Racine's work allowed for studies among different laboratories to be compared and understood more clearly.

Seletracetam is a pyrrolidone-derived drug of the racetam family that is structurally related to levetiracetam. It was under development by UCB Pharmaceuticals as a more potent and effective anticonvulsant drug to replace levetiracetam but its development has been halted.

Lacosamide, sold under the brand name Vimpat among others, is a medication used for the treatment of partial-onset seizures and primary generalized tonic-clonic seizures. It is used by mouth or intravenously.
Post-traumatic epilepsy (PTE) is a form of acquired epilepsy that results from brain damage caused by physical trauma to the brain. A person with PTE experiences repeated post-traumatic seizures more than a week after the initial injury. PTE is estimated to constitute 5% of all cases of epilepsy and over 20% of cases of acquired epilepsy.

Spike-and-wave is a pattern of the electroencephalogram (EEG) typically observed during epileptic seizures. A spike-and-wave discharge is a regular, symmetrical, generalized EEG pattern seen particularly during absence epilepsy, also known as ‘petit mal’ epilepsy. The basic mechanisms underlying these patterns are complex and involve part of the cerebral cortex, the thalamocortical network, and intrinsic neuronal mechanisms.
Kindling is a commonly used model for the development of seizures and epilepsy in which the duration and behavioral involvement of induced seizures increases after seizures are induced repeatedly. Kindling is also referred as an animal visual model of epilepsy that can be produced by focal electrical stimulation in the brain. This is mainly used in visualising epilepsy in humans. The kindling model was first proposed in the late 1960s by Graham V. Goddard and colleagues. Although kindling is a widely used model, its applicability to human epilepsy is controversial.
A convulsant is a drug which induces convulsions and/or epileptic seizures, the opposite of an anticonvulsant. These drugs generally act as stimulants at low doses, but are not used for this purpose due to the risk of convulsions and consequent excitotoxicity. Most convulsants are antagonists at either the GABAA or glycine receptors, or ionotropic glutamate receptor agonists. Many other drugs may cause convulsions as a side effect at high doses but only drugs whose primary action is to cause convulsions are known as convulsants. Nerve agents such as sarin, which were developed as chemical weapons, produce convulsions as a major part of their toxidrome, but also produce a number of other effects in the body and are usually classified separately. Dieldrin which was developed as an insecticide blocks chloride influx into the neurons causing hyperexcitability of the CNS and convulsions. The Irwin observation test and other studies that record clinical signs are used to test the potential for a drug to induce convulsions. Camphor, and other terpenes given to children with colds can act as convulsants in children who have had febrile seizures.

Perampanel, sold under the brand name Fycompa, is an anti-epileptic medication developed by Eisai Co. that is used in addition to other drugs to treat partial seizures and generalized tonic-clonic seizures for people older than twelve years. It was first approved in 2012, and as of 2016, its optimal role in the treatment of epilepsy relative to other drugs was not clear. It was the first antiepileptic drug in the class of selective non-competitive antagonist of AMPA receptors.
Generally, seizures are observed in patients who do not have epilepsy. There are many causes of seizures. Organ failure, medication and medication withdrawal, cancer, imbalance of electrolytes, hypertensive encephalopathy, may be some of its potential causes. The factors that lead to a seizure are often complex and it may not be possible to determine what causes a particular seizure, what causes it to happen at a particular time, or how often seizures occur.
Gene therapy is being studied for some forms of epilepsy. It relies on viral or non-viral vectors to deliver DNA or RNA to target brain areas where seizures arise, in order to prevent the development of epilepsy or to reduce the frequency and/or severity of seizures. Gene therapy has delivered promising results in early stage clinical trials for other neurological disorders such as Parkinson's disease, raising the hope that it will become a treatment for intractable epilepsy.
Drug-resistant epilepsy (DRE), also known as refractory epilepsy, intractable epilepsy, or pharmacoresistant epilepsy refers to a state in which an individual with a diagnosis of epilepsy is unresponsive to multiple first line therapies. Based on the 2010 guidelines from the International League against Epilepsy (ILAE), DRE is officially diagnosed following a lack of therapeutic relief in the form of continued seizure burden after trialing at least two antiepileptic drugs (AEDs) at the appropriate dosage and duration. The probability that the next medication will achieve seizure freedom drops with every failed AED. For example, after two failed AEDs, the probability that the third will achieve seizure freedom is around 4%. Drug-resistant epilepsy is commonly diagnosed after several years of uncontrolled seizures, however, in most cases, it is evident much earlier. Approximately 30% of people with epilepsy have a drug-resistant form. Achieving seizure control in DRE patients is critical as uncontrolled seizures can lead to irreversible damage to the brain, cognitive impairment, and increased risk for sudden unexpected death in epilepsy called SUDEP. Indirect consequences of DRE include seizure related injuries and/or accidents, impairment in daily life, adverse medication effects, increased co-morbidities especially psychological, and increased economic burden, etc.
References
- ↑ Sarkisian, Matthew R. (31 May 2001). "Overview of the Current Animal Models for Human Seizure and Epileptic Disorders". Epilepsy & Behavior. 2 (3): 201–216. doi:10.1006/ebeh.2001.0193. PMID 12609365.
- ↑ Chang, Bernard S.; Lowenstein, Daniel H. (25 September 2003). "Epilepsy". New England Journal of Medicine. 349 (13): 1257–1266. doi:10.1056/NEJMra022308. PMID 14507951.
- ↑ Löscher, Wolfgang (31 May 2011). "Critical review of current animal models of seizures and epilepsy used in the discovery and development of new antiepileptic drugs". Seizure. 20 (5): 359–368. doi: 10.1016/j.seizure.2011.01.003 . PMID 21292505 . Retrieved 1 August 2012.
- ↑ Batot, Gaelle; Metcalf, Cameron S.; Bell, Laura A.; Pauletti, Alberto; Wilcox, Karen S.; Bröer, Sonja (2022-06-23). "A Model for Epilepsy of Infectious Etiology using Theiler's Murine Encephalomyelitis Virus". Journal of Visualized Experiments (184). doi:10.3791/63673. ISSN 1940-087X. PMC 11060116 . PMID 35816000.
- ↑ Cela, Elvis; McFarlan, Amanda R.; Chung, Andrew J.; Wang, Taiji; Chierzi, Sabrina; Murai, Keith K.; Sjöström, P. Jesper (March 27, 2019). "An Optogenetic Kindling Model of Neocortical Epilepsy". Scientific Reports. 9 (1): 5236. doi:10.1038/s41598-019-41533-2. ISSN 2045-2322. PMC 6437216 . PMID 30918286.