Related Research Articles

Over-the-counter (OTC) drugs are medicines sold directly to a consumer without a requirement for a prescription from a healthcare professional, as opposed to prescription drugs, which may be supplied only to consumers possessing a valid prescription. In many countries, OTC drugs are selected by a regulatory agency to ensure that they contain ingredients that are safe and effective when used without a physician's care. OTC drugs are usually regulated according to their active pharmaceutical ingredient (API) rather than final products. By regulating APIs instead of specific drug formulations, governments allow manufacturers the freedom to formulate ingredients, or combinations of ingredients, into proprietary mixtures.

A pharmacist, also known as a chemist or a druggist, is a healthcare professional who dispenses medications and who provides advice on their safe use, with the aim of preventing disease and promoting public health. Pharmacists often serve as primary care providers in the community, and may offer other services such as health screenings and immunizations.

A generic drug is a pharmaceutical drug that contains the same chemical substance as a drug that was originally protected by chemical patents. Generic drugs are allowed for sale after the patents on the original drugs expire. Because the active chemical substance is the same, the medical profile of generics is equivalent in performance. A generic drug has the same active pharmaceutical ingredient (API) as the original, but it may differ in some characteristics such as the manufacturing process, formulation, excipients, color, taste, and packaging.

Pharmacy is the science and practice of discovering, producing, preparing, dispensing, reviewing and monitoring medications, aiming to ensure the safe, effective, and affordable use of medicines. It is a miscellaneous science as it links health sciences with pharmaceutical sciences and natural sciences. The professional practice is becoming more clinically oriented as most of the drugs are now manufactured by pharmaceutical industries. Based on the setting, pharmacy practice is either classified as community or institutional pharmacy. Providing direct patient care in the community of institutional pharmacies is considered clinical pharmacy.

A prescription, often abbreviated ℞ or Rx, is a formal communication from a physician or other registered health-care professional to a pharmacist, authorizing them to dispense a specific prescription drug for a specific patient. Historically, it was a physician's instruction to an apothecary listing the materials to be compounded into a treatment—the symbol ℞ comes from the first word of a medieval prescription, Latin: Recipere, that gave the list of the materials to be compounded.
Prescription drug list prices in the United States continually rank among the highest in the world. The high cost of prescription drugs became a major topic of discussion in the 21st century, leading up to the American health care reform debate of 2009, and received renewed attention in 2015. One major reason for high prescription drug prices in the United States relative to other countries is the inability of government-granted monopolies in the American health care sector to use their bargaining power to negotiate lower prices and that the American payer ends up subsidizing the world's R&D spending on drugs.
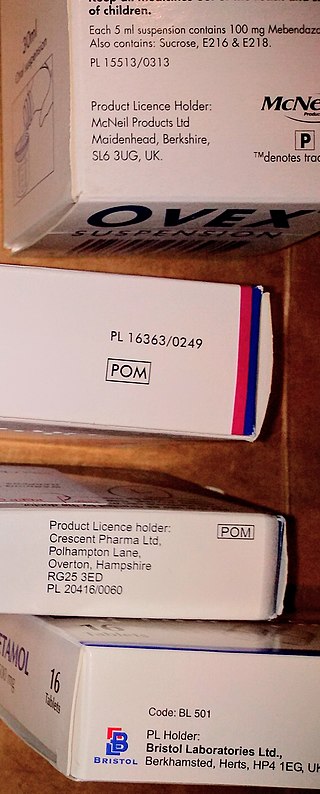
A prescription drug is a pharmaceutical drug that is only permitted to be dispensed to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.
The Pharmaceutical Benefits Scheme (PBS) is a program of the Australian Government that subsidises prescription medication for Australian citizens and permanent residents, as well as international visitors covered by a reciprocal health care agreement. The PBS is separate to the Medicare Benefits Schedule, a list of health care services that can be claimed under Medicare, Australia's universal health care insurance scheme.
An online pharmacy, internet pharmacy, or mail-order pharmacy is a pharmacy that operates over the Internet and sends orders to customers through mail, shipping companies, or online pharmacy web portal.
The NHS treatments blacklist is an informal name for a list of medicines and procedures which will not be funded by public money except in exceptional cases. These include but are not limited to procedures which the National Institute for Health and Care Excellence (NICE) has ruled of limited effectiveness and particular brand name medicines. In 2017 there was a proposal for 3,200 over-the-counter (OTC) drugs to be restricted and 18 procedures to be added to the list. This generated some controversy amongst doctors with some arguing that OTC should be blacklisted instead, and others believing the move did not take into account individual patient needs.
Pharmaceutical policy is a branch of health policy that deals with the development, provision and use of medications within a health care system. It embraces drugs, biologics, vaccines and natural health products.

A pharmacy is a retail shop which provides pharmaceutical drugs, among other products. At the pharmacy, a pharmacist oversees the fulfillment of medical prescriptions and is available to counsel patients about prescription and over-the-counter drugs or about health problems and wellness issues. A typical pharmacy would be in the commercial area of a community.
A formulary is a list of pharmaceutical drugs, often decided upon by a group of people, for various reasons such as insurance coverage or use at a medical facility. Traditionally, a formulary contained a collection of formulas for the compounding and testing of medication. Today, the main function of a prescription formulary is to specify particular medications that are approved to be prescribed at a particular hospital, in a particular health system, or under a particular health insurance policy. The development of prescription formularies is based on evaluations of efficacy, safety, and cost-effectiveness of drugs.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.

Remote dispensing is used in health care environments to describe the use of automated systems to dispense prescription medications without an on-site pharmacist. This practice is most common in long-term care facilities and correctional institutions that do not find it practical to operate a full-service in-house pharmacy.
Pharmacy automation involves the mechanical processes of handling and distributing medications. Any pharmacy task may be involved, including counting small objects ; measuring and mixing powders and liquids for compounding; tracking and updating customer information in databases ; and inventory management. This article focuses on the changes that have taken place in the local, or community pharmacy since the 1960s.
There are approximately 88,000 pharmacies in the United States. Over half are located within drug stores, grocery stores, hospitals, department stores, medical clinics, surgery clinics, universities, nursing homes, prisons, and other facilities. The remaining pharmacies are considered to be independent or privately owned. The top 25 pharmacy chain stores represent about 38,000 pharmacy locations in the U.S. and employ about 149,000 on-staff pharmacists. California has 8,015 pharmacies, the most of any state. Texas, Florida, New York, and Pennsylvania round out the top five states for pharmacy locations. Nationwide, the number of community pharmacies increased by 6.3% between 2007-2015, and the number of pharmacies per 10,000 people (2.11) did not change. However, the number of pharmacies per-capita varies substantially across counties, ranging from 0 to 13.6 per- 10,000 people in 2015.

Telepharmacy is the delivery of pharmaceutical care via telecommunications to patients in locations where they may not have direct contact with a pharmacist. It is an instance of the wider phenomenon of telemedicine, as implemented in the field of pharmacy. Telepharmacy services include drug therapy monitoring, patient counseling, prior authorization and refill authorization for prescription drugs, and monitoring of formulary compliance with the aid of teleconferencing or videoconferencing. Remote dispensing of medications by automated packaging and labeling systems can also be thought of as an instance of telepharmacy. Telepharmacy services can be delivered at retail pharmacy sites or through hospitals, nursing homes, or other medical care facilities.
Pharmacy in the United Kingdom has been an integral part of the National Health Service since it was established in 1948. Unlike the rest of the NHS, pharmacies are largely privately provided apart from those in hospitals, and even these are now often privately run.
Separation of prescribing and dispensing, also called dispensing separation, is a practice in medicine and pharmacy in which the physician who provides a medical prescription is independent from the pharmacist who provides the prescription drug.
References
- 1 2 3 National Audit Office (2007). Prescribing costs in primary care. London: The Stationery Office. ISBN 978-0-10-294517-1.
- 1 2 3 "Automatic Generic Substitution - Clinical Implications for Patients" (PDF). June 2009. Archived from the original (PDF) on 2010-12-28.
- ↑ "Note for guidance on the investigation of bioavailability and bioequivalence" (PDF). London: European Medicines Agency. 2000.
- ↑ "Guideline on the investigation of bioequivalence" (PDF). London: European Medicines Agency. 2008. Archived from the original (PDF) on October 10, 2011.
- ↑ "Patients, physicians, the pharmaceutical industry and the NHS". Royal College of Physicians. February 2009.
- ↑ Thiebaud P, Patel BV, Nichol MB, Berenbeim DM (November 2005). "The effect of switching on compliance and persistence: the case of statin treatment". The American Journal of Managed Care. 11 (11): 670–4. PMID 16268750.
- ↑ Bainbridge JL, Ruscin JM (2009). "Challenges of treatment adherence in older patients with Parkinson's disease". Drugs & Aging. 26 (2): 145–55. doi:10.2165/0002512-200926020-00006. PMID 19220071. S2CID 207296872.
- 1 2 Ansell BJ (July 2008). "Not getting to goal: the clinical costs of noncompliance" (PDF). Journal of Managed Care Pharmacy. 14 (6 Suppl B): 9–15. doi:10.18553/jmcp.2008.14.S6-B.9. PMID 18693783.
- ↑ Carey IM, De Wilde S, Harris T, et al. (2008). "What factors predict potentially inappropriate primary care prescribing in older people? Analysis of UK primary care patient record database". Drugs & Aging. 25 (8): 693–706. doi:10.2165/00002512-200825080-00006. PMID 18665661. S2CID 13582998.
- ↑ PPRS Update. Association of the British Pharmaceutical Industry (10). March 2009.
{{cite journal}}: Missing or empty|title=(help)