Related Research Articles
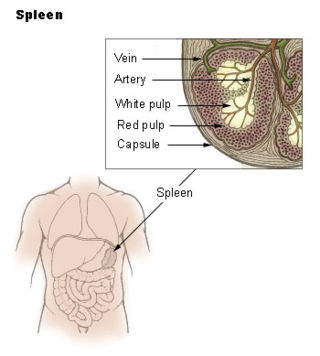
The spleen is an organ found in almost all vertebrates. Similar in structure to a large lymph node, it acts primarily as a blood filter. The word spleen comes from Ancient Greek σπλήν (splḗn).
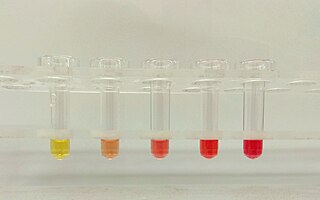
Hemolysis or haemolysis, also known by several other names, is the rupturing (lysis) of red blood cells (erythrocytes) and the release of their contents (cytoplasm) into surrounding fluid. Hemolysis may occur in vivo or in vitro.

The lymphatic system, or lymphoid system, is an organ system in vertebrates that is part of the immune system, and complementary to the circulatory system. It consists of a large network of lymphatic vessels, lymph nodes, lymphoid organs, lymphoid tissues and lymph. Lymph is a clear fluid carried by the lymphatic vessels back to the heart for re-circulation..

Spherocytosis is the presence of spherocytes in the blood, i.e. erythrocytes that are sphere-shaped rather than bi-concave disk shaped as normal. Spherocytes are found in all hemolytic anemias to some degree. Hereditary spherocytosis and autoimmune hemolytic anemia are characterized by having only spherocytes.
A splenectomy is the surgical procedure that partially or completely removes the spleen. The spleen is an important organ in regard to immunological function due to its ability to efficiently destroy encapsulated bacteria. Therefore, removal of the spleen runs the risk of overwhelming post-splenectomy infection, a medical emergency and rapidly fatal disease caused by the inability of the body's immune system to properly fight infection following splenectomy or asplenia.

Hereditary spherocytosis (HS) is a congenital hemolytic disorder, wherein a genetic mutation coding for a structural membrane protein phenotype leads to a spherical shaping of erythrocytic cellular morphology. As erythrocytes are sphere-shaped (spherocytosis), rather than the normal biconcave disk-shaped, their morphology interferes with these cells' abilities to be flexible during circulation throughout the entirety of the body - arteries, arterioles, capillaries, venules, veins, and organs. This difference in shape also makes the red blood cells more prone to rupture under osmotic and/or mechanical stress. Cells with these dysfunctional proteins are degraded in the spleen, which leads to a shortage of erythrocytes resulting in hemolytic anemia.

Hemolytic anemia or haemolytic anaemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.
Immunodeficiency, also known as immunocompromisation, is a state in which the immune system's ability to fight infectious diseases and cancer is compromised or entirely absent. Most cases are acquired ("secondary") due to extrinsic factors that affect the patient's immune system. Examples of these extrinsic factors include HIV infection and environmental factors, such as nutrition. Immunocompromisation may also be due to genetic diseases/flaws such as SCID.
Asplenia refers to the absence of normal spleen function and is associated with some serious infection risks. Hyposplenism is used to describe reduced ('hypo-') splenic functioning, but not as severely affected as with asplenism.
An overwhelming post-splenectomy infection (OPSI) is a rare but rapidly fatal infection occurring in individuals following removal of the spleen. The infections are typically characterized by either meningitis or sepsis, and are caused by encapsulated organisms including Streptococcus pneumoniae. It is a medical emergency and requires immediate treatment. Death has been reported to occur within 12 hours.
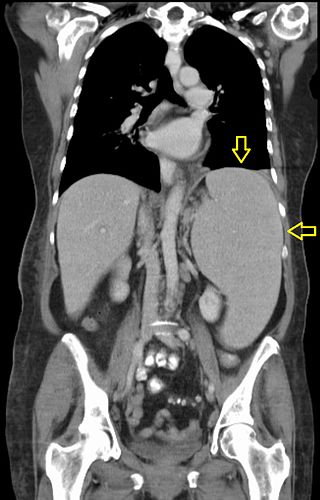
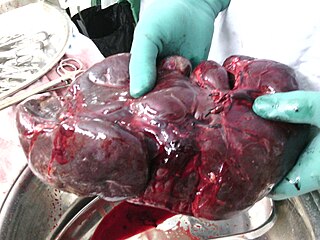
Splenomegaly is an enlargement of the spleen. The spleen usually lies in the left upper quadrant (LUQ) of the human abdomen. Splenomegaly is one of the four cardinal signs of hypersplenism which include: some reduction in number of circulating blood cells affecting granulocytes, erythrocytes or platelets in any combination; a compensatory proliferative response in the bone marrow; and the potential for correction of these abnormalities by splenectomy. Splenomegaly is usually associated with increased workload, which suggests that it is a response to hyperfunction. It is therefore not surprising that splenomegaly is associated with any disease process that involves abnormal red blood cells being destroyed in the spleen. Other common causes include congestion due to portal hypertension and infiltration by leukemias and lymphomas. Thus, the finding of an enlarged spleen, along with caput medusae, is an important sign of portal hypertension.
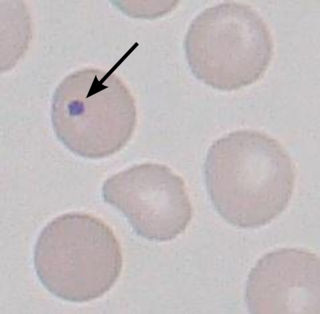
A Howell–Jolly body is a cytopathological finding of basophilic nuclear remnants in circulating erythrocytes. During maturation in the bone marrow, late erythroblasts normally expel their nuclei; but, in some cases, a small portion of DNA remains. The presence of Howell–Jolly bodies usually signifies a damaged or absent spleen, because a healthy spleen would normally filter such erythrocytes.
Warm antibody autoimmune hemolytic anemia (WAIHA) is the most common form of autoimmune haemolytic anemia. About half of the cases are of unknown cause, with the other half attributable to a predisposing condition or medications being taken. Contrary to cold autoimmune hemolytic anemia which happens in cold temperature (28–31 °C), WAIHA happens at body temperature.

Codocytes, also known as target cells, are red blood cells that have the appearance of a shooting target with a bullseye. In optical microscopy these cells appear to have a dark center surrounded by a white ring, followed by dark outer (peripheral) second ring containing a band of hemoglobin. However, in electron microscopy they appear very thin and bell shaped. Because of their thinness they are referred to as leptocytes. On routine smear morphology, some people like to make a distinction between leptocytes and codocytes- suggesting that in leptocytes the central spot is not completely detached from the peripheral ring, i.e. the pallor is in a C shape rather than a full ring.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5–10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.

Sickle cell trait describes a condition in which a person has one abnormal allele of the hemoglobin beta gene, but does not display the severe symptoms of sickle cell disease that occur in a person who has two copies of that allele. Those who are heterozygous for the sickle cell allele produce both normal and abnormal hemoglobin.
Felty's syndrome (FS), also called Felty syndrome, is rare autoimmune disease characterized by the triad of rheumatoid arthritis, enlargement of the spleen and low neutrophil count. The condition is more common in those aged 50–70 years, specifically more prevalent in females than males, and more so in Caucasians than those of African descent. It is a deforming disease that causes many complications for the individual.
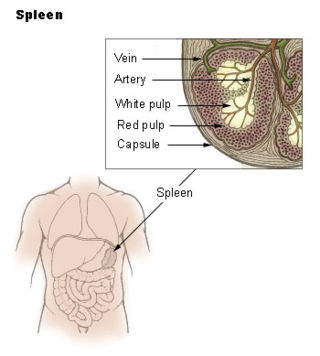
The red pulp of the spleen is composed of connective tissue known also as the cords of Billroth and many splenic sinusoids that are engorged with blood, giving it a red color. Its primary function is to filter the blood of antigens, microorganisms, and defective or worn-out red blood cells.

Splenic infarction is a condition in which blood flow supply to the spleen is compromised, leading to partial or complete infarction in the organ. Splenic infarction occurs when the splenic artery or one of its branches are occluded, for example by a blood clot.
Sickle cell nephropathy is a type of nephropathy associated with sickle cell disease which causes kidney complications as a result of sickling of red blood cells in the small blood vessels. The hypertonic and relatively hypoxic environment of the renal medulla, coupled with the slow blood flow in the vasa recta, favors sickling of red blood cells, with resultant local infarction. Functional tubule defects in patients with sickle cell disease are likely the result of partial ischemic injury to the renal tubules.
References
- ↑ "Autosplenectomy" with sickle cell anemia, gross at WebPath, The Internet Pathology Laboratory for Medical Education at Mercer University School of Medicine. Retrieved September 10, 2011
- 1 2 3 4 5 Brousse, Valentine; Buffet, Pierre; Rees, David (2014-07-01). "The spleen and sickle cell disease: the sick(led) spleen". British Journal of Haematology. 166 (2): 165–176. doi: 10.1111/bjh.12950 . ISSN 1365-2141. PMID 24862308. S2CID 40448991.
- ↑ "Splenectomy Risks - Mayo Clinic". www.mayoclinic.org. Retrieved 2016-03-02.
- ↑ Brigden, Malcolm L. (February 2001). "Detection, Education and Management of the Asplenic or Hyposplenic Patient - American Family Physician". American Family Physician. 63 (3): 499. Retrieved 2016-02-16.
- 1 2 "Splenectomy Results - Mayo Clinic". www.mayoclinic.org. Retrieved 2016-03-03.
- ↑ "What Is the Spleen? Functions & Info | Children's Hospital Pittsburgh". www.chp.edu. Retrieved 2016-03-03.
- ↑ Kirkineska, L (2014). "Functional hyposplenism". Hippokratia. 18 (1): 7–11. PMC 4103047 . PMID 25125944.
- ↑ Di Sabatino, Antonio (April 6, 2011). "Post-splenectomy and hyposplenic states". Lancet. 378 (9785): 86–97. doi:10.1016/s0140-6736(10)61493-6. PMID 21474172. S2CID 30554953.
- ↑ "Red Blood Cell Pit Count". Red Blood Cell Lab. Children's Hospital Oakland Research Institute. 2010. Retrieved March 2, 2016.
- ↑ Henry Knipe; Frank Gaillard. "Autosplenectomy". radiopaedia.org. Retrieved 30 December 2015.
- ↑ Ashley-Koch, A (2000). "Sickle Hemoglobin (Hb S) Allele and Sickle Cell Disease: A HuGE Review" (PDF). American Journal of Epidemiology. 151 (9): 839–845. doi:10.1093/oxfordjournals.aje.a010288. PMID 10791557. Archived from the original (PDF) on 2015-09-06.
- ↑ Santilli, Daniele (2003). "Autosplenectomy and Antiphospholipid Antibodies in Systemic Lupus Erythematosus: A Pathogenic Relationship?". Seminars in Arthritis and Rheumatism. 33 (2): 125–133. doi:10.1016/S0049-0172(03)00004-0. PMID 14625820.