Related Research Articles
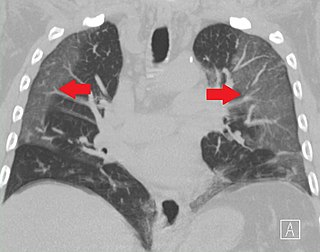
Pulmonary embolism (PE) is a blockage of an artery in the lungs by a substance that has moved from elsewhere in the body through the bloodstream (embolism). Symptoms of a PE may include shortness of breath, chest pain particularly upon breathing in, and coughing up blood. Symptoms of a blood clot in the leg may also be present, such as a red, warm, swollen, and painful leg. Signs of a PE include low blood oxygen levels, rapid breathing, rapid heart rate, and sometimes a mild fever. Severe cases can lead to passing out, abnormally low blood pressure, obstructive shock, and sudden death.
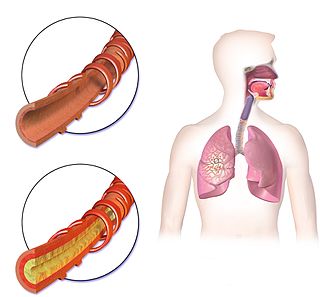
Hemoptysis or haemoptysis is the discharge of blood or blood-stained mucus through the mouth coming from the bronchi, larynx, trachea, or lungs. It does not necessarily involve coughing. In other words, it is the airway bleeding. This can occur with lung cancer, infections such as tuberculosis, bronchitis, or pneumonia, and certain cardiovascular conditions. Hemoptysis is considered massive at 300 mL. In such cases, there are always severe injuries. The primary danger comes from choking, rather than blood loss.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

A chest radiograph, chest X-ray (CXR), or chest film is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine.

A hemothorax is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis, in response to pneumothorax, or rarely in association with other conditions.

Cryptogenic organizing pneumonia (COP), formerly known as bronchiolitis obliterans organizing pneumonia (BOOP), is an inflammation of the bronchioles (bronchiolitis) and surrounding tissue in the lungs. It is a form of idiopathic interstitial pneumonia.

Scimitar syndrome, or congenital pulmonary venolobar syndrome, is a rare congenital heart defect characterized by anomalous venous return from the right lung. This anomalous pulmonary venous return can be either partial (PAPVR) or total (TAPVR). The syndrome associated with PAPVR is more commonly known as Scimitar syndrome after the curvilinear pattern created on a chest radiograph by the pulmonary veins that drain to the inferior vena cava. This radiographic density often has the shape of a scimitar, a type of curved sword. The syndrome was first described by Catherine Neill in 1960.

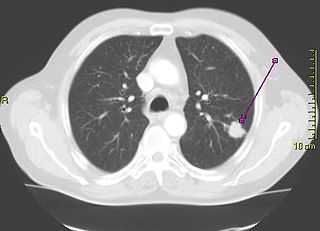
A tuberculoma is a clinical manifestation of tuberculosis which conglomerates tubercles into a firm lump, and so can mimic cancer tumors of many types in medical imaging studies. They often arise within individuals in whom a primary tuberculosis infection is not well controlled. When tuberculomas arise intracranially, they represent a manifestation of CNS tuberculosis. Since these are evolutions of primary complex, the tuberculomas may contain caseum or calcifications.
In chest radiography, the Westermark sign is a sign that represents a focus of oligemia (hypovolemia) seen distal to a pulmonary embolism (PE). While the chest x-ray is normal in the majority of PE cases, the Westermark sign is seen in 2% of patients.

A CT pulmonary angiogram (CTPA) is a medical diagnostic test that employs computed tomography (CT) angiography to obtain an image of the pulmonary arteries. Its main use is to diagnose pulmonary embolism (PE). It is a preferred choice of imaging in the diagnosis of PE due to its minimally invasive nature for the patient, whose only requirement for the scan is an intravenous line.

Usual interstitial pneumonia (UIP) is a form of lung disease characterized by progressive scarring of both lungs. The scarring (fibrosis) involves the pulmonary interstitium. UIP is thus classified as a form of interstitial lung disease.

High-resolution computed tomography (HRCT) is a type of computed tomography (CT) with specific techniques to enhance image resolution. It is used in the diagnosis of various health problems, though most commonly for lung disease, by assessing the lung parenchyma. On the other hand, HRCT of the temporal bone is used to diagnose various middle ear diseases such as otitis media, cholesteatoma, and evaluations after ear operations.

A pulmonary contusion, also known as lung contusion, is a bruise of the lung, caused by chest trauma. As a result of damage to capillaries, blood and other fluids accumulate in the lung tissue. The excess fluid interferes with gas exchange, potentially leading to inadequate oxygen levels (hypoxia). Unlike pulmonary laceration, another type of lung injury, pulmonary contusion does not involve a cut or tear of the lung tissue.

A lung nodule or pulmonary nodule is a relatively small focal density in the lung. A solitary pulmonary nodule (SPN) or coin lesion, is a mass in the lung smaller than three centimeters in diameter. A pulmonary micronodule has a diameter of less than three millimetres. There may also be multiple nodules.
Ground-glass opacity (GGO) is a finding seen on chest x-ray (radiograph) or computed tomography (CT) imaging of the lungs. It is typically defined as an area of hazy opacification (x-ray) or increased attenuation (CT) due to air displacement by fluid, airway collapse, fibrosis, or a neoplastic process. When a substance other than air fills an area of the lung it increases that area's density. On both x-ray and CT, this appears more grey or hazy as opposed to the normally dark-appearing lungs. Although it can sometimes be seen in normal lungs, common pathologic causes include infections, interstitial lung disease, and pulmonary edema.

Bilateral hilar lymphadenopathy is a bilateral enlargement of the lymph nodes of pulmonary hila. It is a radiographic term for the enlargement of mediastinal lymph nodes and is most commonly identified by a chest x-ray.

Pneumatosis is the abnormal presence of air or other gas within tissues.

Pulmonary alveolar microlithiasis (PAM) is a rare, inherited disorder of lung phosphate balance that is associated with small stone formation in the airspaces of the lung. Mutations in the gene SLC34A2 result in loss of a key sodium, phosphate co-transporter, known to be expressed in distal alveolar type II cells, as well as in the mammary gland, and to a lesser extent in intestine, kidney, skin, prostate and testes. As the disease progresses, the lung fields become progressively more dense (white) on the chest xray, and low oxygen level, lung inflammation and fibrosis, elevated pressures in the lung blood vessels, and respiratory failure ensue, usually in middle age. The clinical course of PAM can be highly variable, with some patients remaining asymptomatic for decades, and others progressing more rapidly. There is no effective treatment, and the mechanisms of stone formation, inflammation and scarring are not known.

Mediastinal shift is an abnormal movement of the mediastinal structures toward one side of the chest cavity. A shift indicates a severe imbalance of pressures inside the chest. Mediastinal shifts are generally caused by increased lung volume, decreased lung volume, or abnormalities in the pleural space. Additionally, masses inside the mediastinum or musculoskeletal abnormalities can also lead to abnormal mediastinal arrangement. Typically, these shifts are observed on x-ray but also on computed tomography (CT) or magnetic resonance imaging (MRI). On chest x-ray, tracheal deviation, or movement of the trachea away from its midline position can be used as a sign of a shift. Other structures, like the heart, can also be used as reference points. Below are examples of pathologies that can cause a mediastinal shift and their appearance.
Computed tomography of the chest or chest CT is a group of computed tomography scan protocols used in medical imaging to evaluate the lungs and search for lung disorders.
References
- ↑ Jain, Sanjay N; Modi, Tanvi; Aswani, Yashant; Varma, Ravi U (2019). "Chest radiography in adult critical care unit: A pictorial review". The Indian Journal of Radiology & Imaging. 29 (4): 418–425. doi: 10.4103/ijri.IJRI_329_19 . ISSN 0971-3026. PMC 6958895 . PMID 31949345.
- ↑ "Bat Wing Pulmonary Opacities (Concept Id: C3273929) - MedGen - NCBI" . Retrieved 17 October 2021.
- ↑ Khan, Ali Nawaz; Al-Jahdali, Hamdan; AL-Ghanem, Sarah; Gouda, Alaa (2009). "Reading chest radiographs in the critically ill (Part II): Radiography of lung pathologies common in the ICU patient". Annals of Thoracic Medicine. 4 (3): 149–157. doi: 10.4103/1817-1737.53349 . ISSN 1817-1737. PMC 2714572 . PMID 19641649.
- 1 2 Yudin, Andrey (2014). "Bat Wing, Butterfly, or Angel Wing Sign". Metaphorical Signs in Computed Tomography of Chest and Abdomen. Springer International Publishing. p. 11. doi:10.1007/978-3-319-04013-4_6. ISBN 978-3-319-04012-7 . Retrieved 17 October 2021.