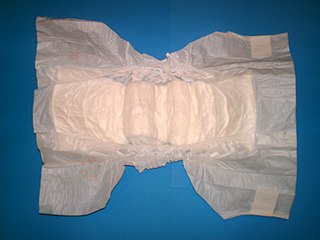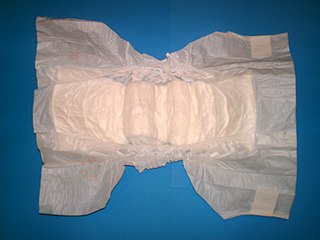
A diaper or a nappy is a type of underwear that allows the wearer to urinate or defecate without using a toilet, by absorbing or containing waste products to prevent soiling of outer clothing or the external environment. When diapers become wet or soiled, they require changing, generally by a second person such as a parent or caregiver. Failure to change a diaper on a sufficiently regular basis can result in skin problems around the area covered by the diaper.

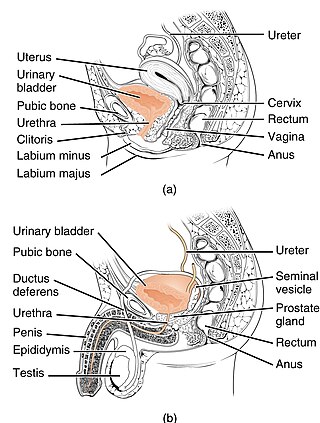
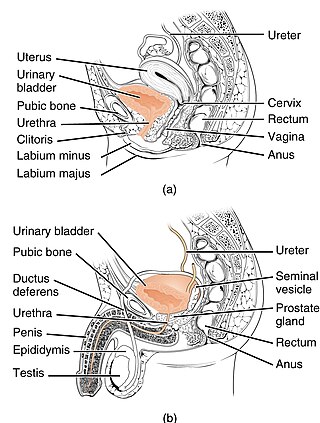
The human urinary system, also known as the urinary tract or renal system, consists of the kidneys, ureters, bladder, and the urethra. The purpose of the urinary system is to eliminate waste from the body, regulate blood volume and blood pressure, control levels of electrolytes and metabolites, and regulate blood pH. The urinary tract is the body's drainage system for the eventual removal of urine. The kidneys have an extensive blood supply via the renal arteries which leave the kidneys via the renal vein. Each kidney consists of functional units called nephrons. Following filtration of blood and further processing, wastes exit the kidney via the ureters, tubes made of smooth muscle fibres that propel urine towards the urinary bladder, where it is stored and subsequently expelled through the urethra during urination. The female and male urinary system are very similar, differing only in the length of the urethra.

Urolagnia is a paraphilia in which sexual excitement is associated with the sight or thought of urine or urination. The term has origins in the Greek language. Golden shower is slang for the practice of urinating on another person for sexual pleasure.
Operant conditioning, also called instrumental conditioning, is a learning process where voluntary behaviors are modified by association with the addition of reward or aversive stimuli. The frequency or duration of the behavior may increase through reinforcement or decrease through punishment or extinction.
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis. UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse. People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.
Classical conditioning is a behavioral procedure in which a biologically potent stimulus is paired with a neutral stimulus. The term classical conditioning refers to the process of an automatic, conditioned response that is paired with a specific stimulus.

Nocturnal enuresis (NE), also informally called bedwetting, is involuntary urination while asleep after the age at which bladder control usually begins. Bedwetting in children and adults can result in emotional stress. Complications can include urinary tract infections.

Enuresis is a repeated inability to control urination. Use of the term is usually limited to describing people old enough to be expected to exercise such control. Involuntary urination is also known as urinary incontinence. The term "enuresis" comes from the Ancient Greek: ἐνούρησις, romanized: enoúrēsis.
The experimental analysis of behavior is a science that studies the behavior of individuals across a variety of species. A key early scientist was B. F. Skinner who discovered operant behavior, reinforcers, secondary reinforcers, contingencies of reinforcement, stimulus control, shaping, intermittent schedules, discrimination, and generalization. A central method was the examination of functional relations between environment and behavior, as opposed to hypothetico-deductive learning theory that had grown up in the comparative psychology of the 1920–1950 period. Skinner's approach was characterized by observation of measurable behavior which could be predicted and controlled. It owed its early success to the effectiveness of Skinner's procedures of operant conditioning, both in the laboratory and in behavior therapy.

Paruresis, also known as shy bladder syndrome, is a type of phobia in which a person is unable to urinate in the real or imaginary presence of others, such as in a public restroom. The analogous condition that affects bowel movement is called parcopresis or shy bowel.
Behaviorism is a systematic approach to understand the behavior of humans and other animals. It assumes that behavior is either a reflex evoked by the pairing of certain antecedent stimuli in the environment, or a consequence of that individual's history, including especially reinforcement and punishment contingencies, together with the individual's current motivational state and controlling stimuli. Although behaviorists generally accept the important role of heredity in determining behavior, they focus primarily on environmental events. The cognitive revolution of the late 20th century largely replaced behaviorism as an explanatory theory with cognitive psychology, which unlike behaviorism examines internal mental states.
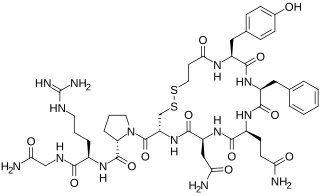
Desmopressin, sold under the trade name DDAVP among others, is a medication used to treat diabetes insipidus, bedwetting, hemophilia A, von Willebrand disease, and high blood urea levels. In hemophilia A and von Willebrand disease, it should only be used for mild to moderate cases. It may be given in the nose, by injection into a vein, by mouth, or under the tongue.

Goodnites are diapers designed for managing bedwetting. Goodnites are produced by Kimberly-Clark. The product has also been seen titled as Huggies Goodnites on official Huggies branded webpages.
Extinction is a behavioral phenomenon observed in both operantly conditioned and classically conditioned behavior, which manifests itself by fading of non-reinforced conditioned response over time. When operant behavior that has been previously reinforced no longer produces reinforcing consequences the behavior gradually stops occurring. In classical conditioning, when a conditioned stimulus is presented alone, so that it no longer predicts the coming of the unconditioned stimulus, conditioned responding gradually stops. For example, after Pavlov's dog was conditioned to salivate at the sound of a metronome, it eventually stopped salivating to the metronome after the metronome had been sounded repeatedly but no food came. Many anxiety disorders such as post traumatic stress disorder are believed to reflect, at least in part, a failure to extinguish conditioned fear.
Frequent urination, or urinary frequency, is the need to urinate more often than usual. Diuretics are medications that increase urinary frequency. Nocturia is the need of frequent urination at night. The most common cause of this condition for women and children is a urinary tract infection. The most common cause of urinary frequency in older men is an enlarged prostate.
Diurnal enuresis is daytime wetting. Nocturnal enuresis is nighttime wetting. Enuresis is defined as the involuntary voiding of urine beyond the age of anticipated control. Both of these conditions can occur at the same time, although many children with nighttime wetting will not have wetting during the day. Children with daytime wetting may have frequent urination, have urgent urination or dribble after urinating.
Urologic diseases or conditions include urinary tract infections, kidney stones, bladder control problems, and prostate problems, among others. Some urologic conditions do not affect a person for that long and some are lifetime conditions. Kidney diseases are normally investigated and treated by nephrologists, while the specialty of urology deals with problems in the other organs. Gynecologists may deal with problems of incontinence in women.
In health care, toileting is the act of assisting a dependent patient with their elimination needs.
Giggle incontinence, giggle enuresis or enuresis risoria is the involuntary release of urine in response to giggling or laughter. The bladder may empty completely or only partially.
The term conditioned emotional response (CER) can refer to a specific learned behavior or a procedure commonly used in classical or Pavlovian conditioning research. It may also be called "conditioned suppression" or "conditioned fear response (CFR)." It is an "emotional response" that results from classical conditioning, usually from the association of a relatively neutral stimulus with a painful or fear-inducing unconditional stimulus. As a result, the formerly neutral stimulus elicits fear. For example, if seeing a dog is paired with the pain of being bitten by the dog, seeing a dog may become a conditioned stimulus that elicits fear.